Pancreatic cancer has long been one of the most devastating diagnoses in medicine. It is aggressive, often silent until late stages, and resistant to many forms of treatment. For decades, doctors have known that smoking increases the risk of developing pancreatic cancer and worsens survival rates. But the exact biological reason behind this deadly link has remained frustratingly elusive—until now.
A groundbreaking study from the University of Michigan Health Rogel Cancer Center, published in Cancer Discovery, has shed new light on how cigarette toxins fuel pancreatic cancer. The findings not only explain why smokers are more vulnerable but also point toward promising new treatment strategies.
The Culprit: A Rogue Immune Response
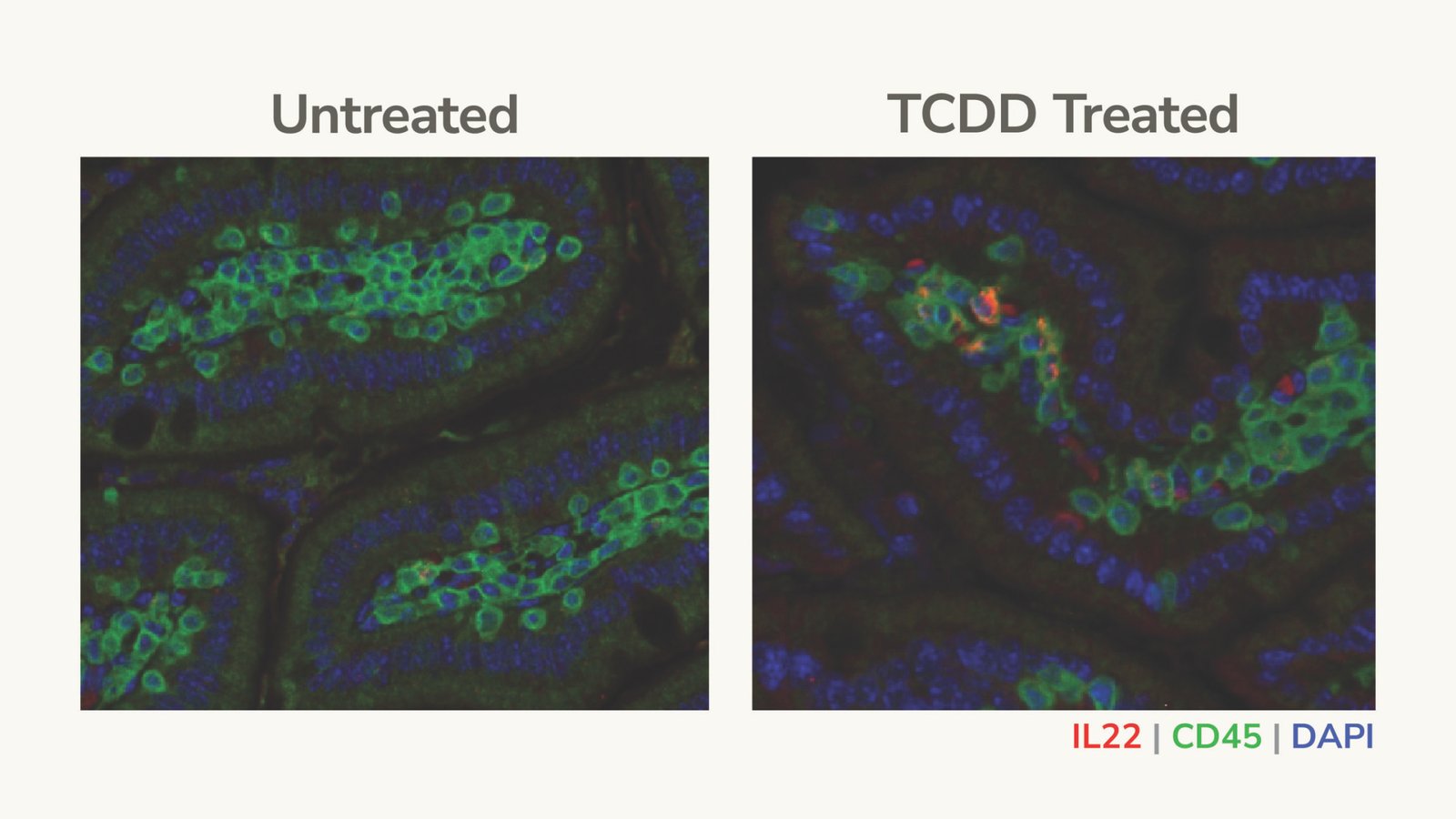
The research team began by exposing mice with pancreatic tumors to a chemical found in cigarettes and other environmental toxins. They were not simply testing whether smoking-related chemicals caused damage—they wanted to see how these toxins would interact with the immune system.
What they discovered was startling. The chemical exposure triggered the release of a protein called interleukin-22 (IL-22). This protein, already known to influence the tumor microenvironment, suddenly became a dangerous accelerant. Tumors grew larger, spread more quickly throughout the body, and became strikingly more aggressive.
“It dramatically changed the way the tumors behave,” explained senior study author Dr. Timothy L. Frankel, co-director of the Rogel and Blondy Center for Pancreatic Cancer. “They grew much bigger, they metastasized throughout the body. It was really quite dramatic.”
The Role of Super-Suppressive Cells
The scientists dug deeper and uncovered a surprising twist: the culprit wasn’t the tumor cells alone, but a specialized subset of immune cells. Under normal conditions, the immune system is supposed to act as a vigilant guardian, detecting and destroying malignant cells. But in the case of smokers, the system appears to be hijacked.
The toxins stimulated a group of T-regulatory (Treg) immune cells, known for their role in preventing autoimmune disorders. In pancreatic cancer, however, these cells turned traitorous. They produced IL-22 and simultaneously shut down the immune system’s natural defenses against tumors.
“It’s a two-pronged attack,” Frankel said. “These T-regulatory cells have the ability to both make IL-22 but also massively suppress any anti-tumor immunity. When we eliminated all the Treg cells from these mice, we reversed the entire ability of the cigarette chemical to let the tumor grow.”
Confirming the Evidence in Humans
The findings in mice were profound, but the researchers needed to see if the same mechanism was at work in people. They turned to human immune cells and samples from pancreatic cancer patients—and the results confirmed their suspicions.
Smokers with pancreatic cancer had significantly more Treg cells than nonsmokers. The immune environment in their tumors was heavily skewed toward suppression, leaving the body unable to mount an effective response.
Even more encouraging was the discovery that an inhibitor drug, designed to block the effects of the cigarette toxin, was able to shrink tumors in experimental models. This offers a glimmer of hope that targeting this pathway could one day improve outcomes for patients.
Rethinking Treatment and Prevention
These insights carry major implications for both treatment and prevention. If smoking drives pancreatic cancer by supercharging Treg cells, then blocking this pathway could “unlock” the body’s natural ability to fight tumors. This could make pancreatic cancer—which has historically been resistant to immunotherapies—more vulnerable to new treatment combinations.
“If we are able to inhibit the super-suppressive cells, we might also unlock natural anti-tumor immunity,” Frankel said. “This could be even further activated by current immunotherapies, which do not work well in pancreatic cancer because of the immunosuppressive environment.”
Beyond treatment, the research underscores the urgent need for tailored approaches. Smokers who develop pancreatic cancer may need specialized therapies to counteract the unique immune suppression caused by tobacco toxins. It also raises the possibility that smokers should be screened more closely, even though effective widespread screening tools for pancreatic cancer are still lacking.
The Human Cost of Smoking
This study adds to the already overwhelming evidence of smoking’s destructive power. While most people associate cigarettes with lung cancer, the truth is that smoking increases the risk of multiple cancers, including pancreatic. Unlike some diseases that progress slowly, pancreatic cancer often advances rapidly, robbing patients and families of precious time.
The new findings highlight that smoking does not just trigger cancer—it alters the body’s defenses in a way that actively fuels its progression. For those with a family history of pancreatic cancer or other pancreatic conditions, smoking is not simply risky—it may be life-threatening.
Signs to Watch For
One of the greatest challenges of pancreatic cancer is that symptoms often appear late, when the disease has already spread. Still, awareness can make a difference. Warning signs include unexplained weight loss, persistent back pain, yellowing of the skin or eyes (jaundice), and digestive issues. For smokers, these symptoms should be taken especially seriously, and early consultation with a specialist could be lifesaving.
A Path Forward
The University of Michigan study represents a turning point in our understanding of how smoking worsens pancreatic cancer. By revealing the role of IL-22 and super-suppressive Treg cells, it opens the door to new treatments that could finally give patients a fighting chance.
But it also serves as a stark reminder: prevention remains the most powerful tool. Avoiding cigarettes, especially for those already at risk, can mean the difference between life and death.
In the words of Dr. Frankel, “There’s a potential that we need to treat smokers who develop pancreatic cancer differently. We may also need to screen smokers more closely. But perhaps most importantly, people need to know the risks. Smoking doesn’t just cause cancer—it helps cancer win.”
More information: Aryl hydrocarbon receptor ligands drive pancreatic cancer initiation and progression through pro-tumorigenic T cell polarization, Cancer Discovery (2025). DOI: 10.1158/2159-8290.CD-25-0377