Cervical cancer is one of those conditions that quietly develops inside the body, often without any obvious signs until it has reached advanced stages. It begins in the cervix—the narrow passage that connects the lower part of the uterus to the vagina—and if left unchecked, it can have devastating consequences for a woman’s health, fertility, and life itself.
Yet there is something uniquely important about cervical cancer: it is one of the most preventable forms of cancer. With modern medical science, early detection tools, and vaccines that target the root cause, the majority of cervical cancer cases can be avoided. This fact alone makes the disease both heartbreaking—because too many women still suffer and die unnecessarily—and hopeful, because the tools for prevention and treatment are already in our hands.
To truly understand cervical cancer, we must explore its causes, the way it manifests, how doctors diagnose it, and the evolving treatments that are saving lives around the world.
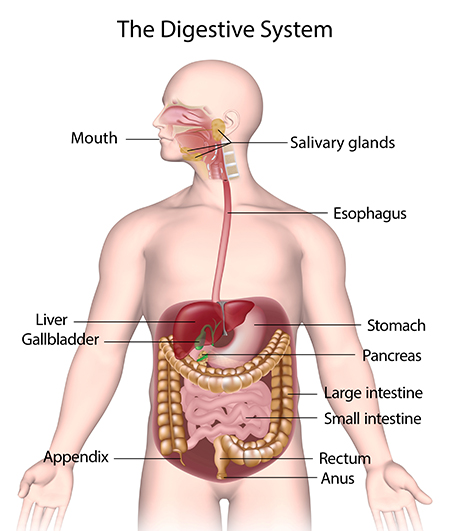
The Cervix: Understanding the Battleground
The cervix may be small, but it plays a vital role in a woman’s reproductive system. It acts as a gateway: it allows menstrual blood to leave the uterus, produces cervical mucus that helps or hinders sperm movement depending on the menstrual cycle, and dilates during childbirth to allow the passage of a baby.
Because it is constantly exposed to both the internal uterine environment and the external vaginal environment, the cervix is particularly vulnerable to infections. Among these infections, one stands out as the main driver of cervical cancer: the human papillomavirus (HPV).
Causes of Cervical Cancer
Human Papillomavirus (HPV) Infection
The overwhelming majority of cervical cancer cases are caused by persistent infection with high-risk strains of HPV. This virus is extremely common—most sexually active people will be exposed to it at some point in their lives. In many cases, the body’s immune system clears the infection naturally. But sometimes, the virus lingers. When high-risk strains, such as HPV-16 and HPV-18, persist, they can trigger genetic changes in cervical cells, eventually leading to cancer.
HPV spreads primarily through sexual contact, but it does not require penetration; skin-to-skin genital contact is often enough. The virus is stealthy, usually causing no symptoms in its early stages, which is why many people do not realize they are infected.
Additional Risk Factors
While HPV is the key cause, not every HPV infection leads to cervical cancer. Several other factors influence whether an infection develops into cancer:
- Weakened immune system: Conditions such as HIV or medications that suppress immunity make it harder for the body to fight off HPV.
- Smoking: Tobacco introduces harmful chemicals that damage cervical cells and make HPV infections more persistent.
- Early sexual activity and multiple partners: These increase exposure to HPV.
- Long-term use of oral contraceptives: Some studies suggest a link between extended use and higher cervical cancer risk, though the benefits and risks must be weighed carefully.
- Socioeconomic barriers: Limited access to screening and healthcare can delay diagnosis and treatment, making the disease deadlier in underserved communities.
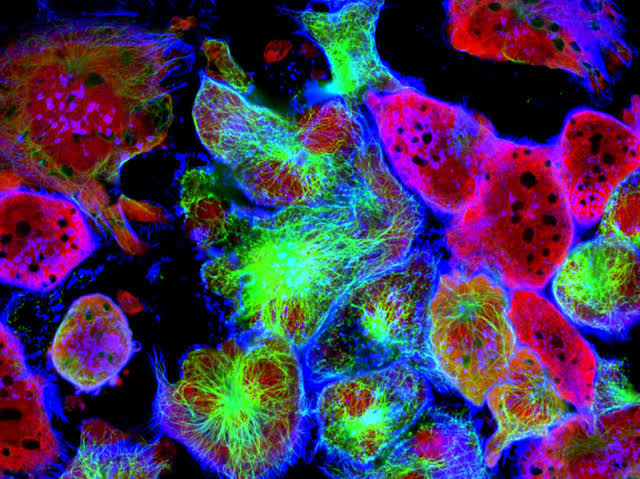
How Cervical Cancer Develops
Cancer does not appear overnight. Cervical cancer develops slowly, moving through identifiable stages:
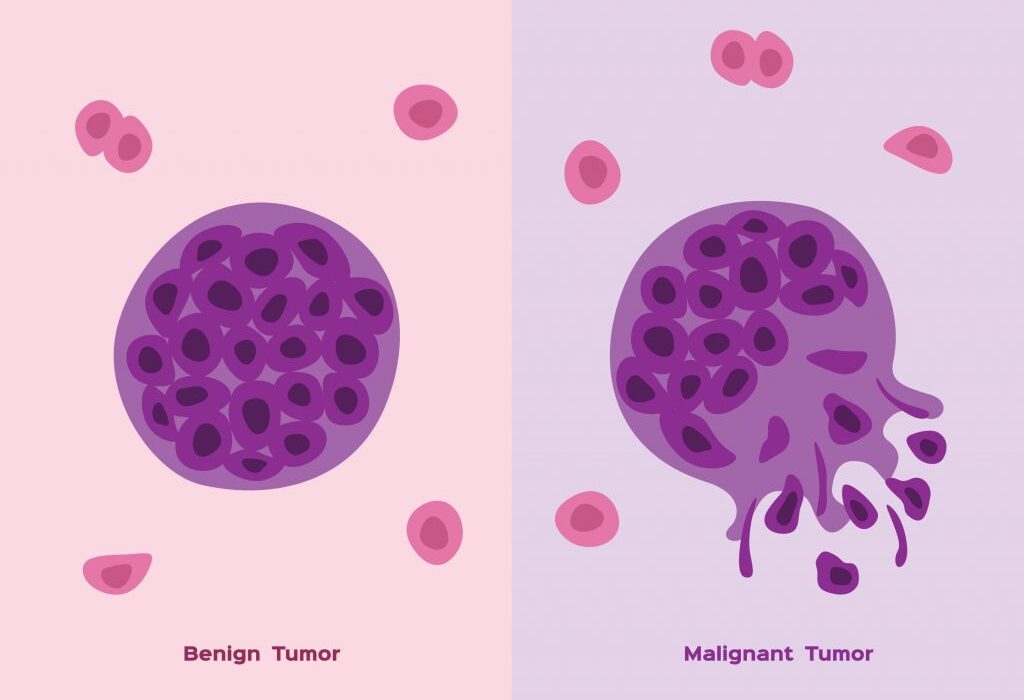
- Normal cervical cells are healthy and functioning as they should.
- HPV infection introduces genetic disruptions.
- Precancerous changes (cervical intraepithelial neoplasia or CIN): Cells start to look abnormal under the microscope, but they have not yet invaded deeper tissues.
- Carcinoma in situ: Abnormal cells spread across the cervix surface but still remain contained.
- Invasive cervical cancer: The cells break through the basement membrane of the cervix, spreading into deeper tissues and potentially to other organs.
Because the progression is usually slow—often taking 10 to 15 years—screening offers a critical opportunity to detect and treat precancerous changes before they become life-threatening.
Symptoms of Cervical Cancer
One of the greatest dangers of cervical cancer is its silence. In its early stages, it rarely causes noticeable symptoms. Women can carry precancerous or cancerous cells for years without knowing. This is why regular screening is essential.
When symptoms do appear, they often include:
- Abnormal vaginal bleeding: This may occur between menstrual periods, after sexual intercourse, or after menopause.
- Unusual vaginal discharge: It may be watery, bloody, or foul-smelling.
- Pelvic pain or pain during sex: This may signal that the cancer has grown and is affecting surrounding tissues.
In advanced stages, additional symptoms may include swelling in the legs, difficulty urinating, blood in urine, or severe back and pelvic pain, reflecting the spread of cancer beyond the cervix.
Diagnosis of Cervical Cancer
Pap Smear (Pap Test)
The Pap smear remains one of the most effective tools in the fight against cervical cancer. During this test, a healthcare provider collects cells from the cervix and examines them under a microscope for abnormalities. Regular Pap tests have dramatically reduced cervical cancer rates in countries where they are widely used.
HPV Testing
Because HPV infection is the leading cause, testing for the virus has become a cornerstone of cervical cancer screening. HPV tests can identify whether high-risk strains are present, even before cells show abnormal changes.
Colposcopy and Biopsy
If a Pap test or HPV test suggests abnormalities, the next step is a colposcopy—a procedure where the doctor uses a special magnifying device to closely examine the cervix. If suspicious areas are seen, a biopsy is taken for laboratory analysis to confirm the presence of precancerous or cancerous cells.
Imaging and Staging
If cancer is confirmed, imaging tests such as MRI, CT, or PET scans may be used to determine how far it has spread. Staging is crucial in guiding treatment decisions, ranging from localized (confined to the cervix) to advanced stages (spread to other parts of the body).
Treatment of Cervical Cancer
Treatment depends on the stage of the disease, the patient’s age, general health, and desire for future fertility. Over the years, treatments have evolved to not only save lives but also preserve quality of life.
Surgery
In early-stage cervical cancer, surgery is often the first line of treatment. Options include:
- Conization: Removal of a cone-shaped section of abnormal tissue, often used for precancerous lesions.
- Hysterectomy: Removal of the uterus and cervix. This may be total or radical, depending on how far the cancer has spread. For some women, this ends the possibility of pregnancy, which makes counseling and support essential.
- Trachelectomy: In selected cases, surgeons can remove the cervix while leaving the uterus intact, preserving the possibility of future pregnancies.
Radiation Therapy
Radiation uses high-energy beams to destroy cancer cells. It is often combined with chemotherapy in advanced stages. Side effects may include fatigue, skin irritation, and changes in bladder or bowel function, but advancements in technology have reduced these risks.
Chemotherapy
Chemotherapy uses drugs to kill cancer cells or stop them from dividing. It is typically given intravenously and may be used in combination with radiation (chemoradiation). Side effects include nausea, hair loss, and lowered immunity, but supportive care has improved outcomes.
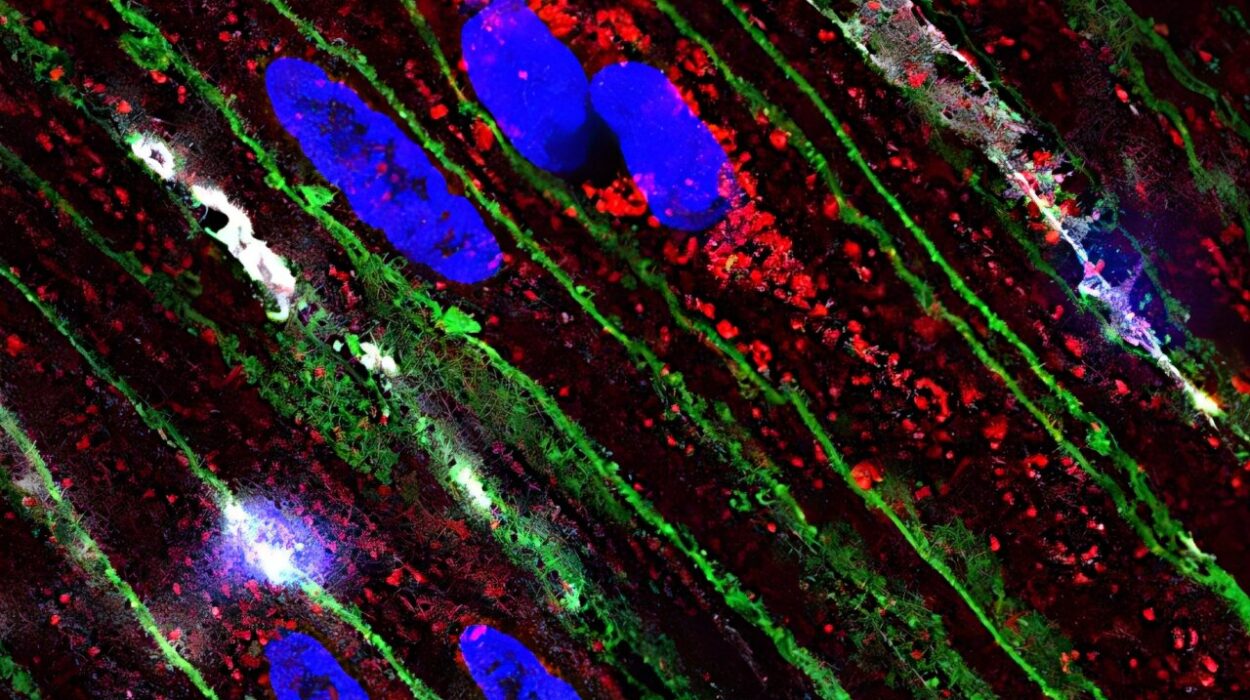
Targeted Therapy and Immunotherapy
The future of cervical cancer treatment lies in personalized medicine. Targeted therapies, such as bevacizumab (an anti-angiogenic drug that prevents tumor blood supply), and immunotherapies, such as checkpoint inhibitors, are opening new possibilities for patients with advanced disease. These treatments harness the body’s own immune system or attack specific cancer pathways, offering hope for longer survival and improved quality of life.
Living with Cervical Cancer
Cervical cancer is not just a medical condition—it is an emotional, social, and psychological journey. Diagnosis often comes with shock, fear, and uncertainty. Treatment can affect fertility, body image, and sexual health, all of which profoundly influence self-esteem and relationships.
Survivorship programs, counseling, and support groups play an important role in helping women cope with the challenges of treatment and recovery. Healthcare is moving toward holistic care—treating not just the disease, but the person as a whole.
Prevention: The Greatest Victory
The most powerful tool against cervical cancer is prevention. Unlike many cancers, we know the primary cause and have vaccines to combat it.
HPV Vaccination
Vaccines such as Gardasil and Cervarix protect against high-risk HPV strains, including types 16 and 18. Vaccination is most effective when given before exposure to the virus, which is why it is recommended for preteens (both boys and girls), though it can also benefit older individuals. Countries that have implemented widespread HPV vaccination programs have already seen dramatic declines in HPV infections and precancerous lesions.
Regular Screening
Pap smears and HPV testing remain essential, even in vaccinated populations, because vaccines do not cover all cancer-causing strains. Screening ensures that precancerous changes are caught early, when they are most treatable.
Healthy Lifestyle Choices
Avoiding smoking, practicing safe sex, and maintaining a strong immune system through good nutrition, exercise, and sleep can all reduce the risk of cervical cancer.
Global Burden and Inequality
While cervical cancer rates have declined in high-income countries with strong vaccination and screening programs, it remains a leading cause of cancer deaths among women in low- and middle-income countries. Here, limited access to healthcare, cultural barriers, and lack of awareness prevent many women from receiving life-saving care.
Addressing cervical cancer globally is not just a medical issue but a matter of equity and justice. Every woman, regardless of where she is born, deserves protection against this preventable disease.
The Future of Cervical Cancer Care
Medical research continues to push boundaries. Advances in genomics may allow doctors to predict which HPV infections are most likely to cause cancer. New vaccines may expand protection against additional strains. Artificial intelligence is being tested to improve screening accuracy, especially in resource-limited areas.
The vision of a world where cervical cancer is eliminated is no longer a fantasy. The WHO has even set a global goal: to reduce new cervical cancer cases by 40% and save 5 million lives by 2050 through vaccination, screening, and treatment.
A Message of Hope
Cervical cancer is a disease that embodies both tragedy and possibility. Tragedy, because too many women still die from it—often young mothers whose deaths ripple across families and communities. Possibility, because it is preventable, detectable, and treatable with the tools we already possess.
To fight cervical cancer is to fight for women’s health, dignity, and equality. It is to ensure that no woman loses her life to a disease that could have been stopped in its earliest stages. The battle is not over, but with vaccines, education, and global cooperation, a world free of cervical cancer is within our reach.