Endometriosis is one of the most misunderstood and underdiagnosed medical conditions affecting women and people assigned female at birth. For centuries, its symptoms were dismissed as “normal menstrual pain” or attributed to hysteria, anxiety, or emotional fragility. Yet, endometriosis is a very real and often debilitating disease—one that can impact fertility, daily functioning, and overall quality of life.
At its core, endometriosis is a condition in which tissue resembling the endometrium—the lining of the uterus—begins to grow outside of the uterus. These growths can appear on the ovaries, fallopian tubes, bladder, intestines, and other organs in the pelvic region. In rare cases, they may even be found beyond the pelvis, such as in the lungs or diaphragm.
Unlike the normal endometrium, which sheds during menstruation, this misplaced tissue has no way to exit the body. It responds to hormonal cycles by thickening and breaking down, but instead of leaving the body, it becomes trapped, causing inflammation, scarring, and adhesions. Over time, this leads to pain that is often severe and chronic.
The condition affects an estimated 1 in 10 women of reproductive age worldwide, though the true prevalence may be higher because of delayed or missed diagnoses. Despite its frequency, endometriosis remains shrouded in stigma and misunderstanding, leaving millions to suffer in silence.
The Emotional and Social Impact of Endometriosis
Before diving into the biology, it is crucial to acknowledge the human side of endometriosis. For many, the condition is not just about physical pain but also about the emotional weight it carries. Patients often face years of being told their pain is “normal,” leading to feelings of isolation, frustration, and mistrust of the healthcare system.
Pain during menstruation can mean missing school or work, straining relationships, and constantly planning life around cycles. For some, infertility becomes an additional heartbreaking reality. This invisible illness can affect mental health, leading to anxiety, depression, and feelings of diminished self-worth.
Endometriosis is more than a gynecological disorder—it is a whole-body, whole-life condition that deserves compassionate understanding as much as scientific investigation.
The Causes of Endometriosis: Unraveling the Mystery
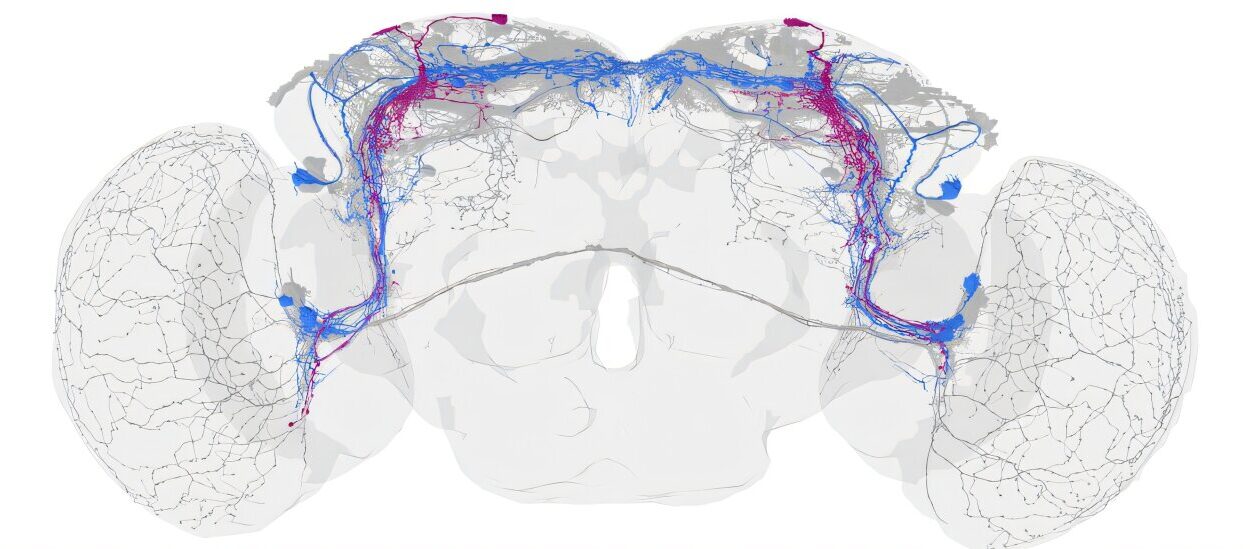
One of the great challenges of endometriosis is that its exact cause remains unknown. Researchers have identified several theories, and it is likely that the condition arises from a combination of genetic, hormonal, immune, and environmental factors.
Retrograde Menstruation Theory
This is the most widely accepted explanation. It suggests that during menstruation, some of the menstrual blood flows backward through the fallopian tubes into the pelvic cavity instead of leaving the body. This blood contains endometrial cells, which then implant themselves on pelvic organs and continue to grow. However, since retrograde menstruation occurs in many women who never develop endometriosis, other factors must also be involved.
Genetic Predisposition
Endometriosis tends to run in families. Women with a mother or sister who has the condition are more likely to develop it. This points to a hereditary component that may increase susceptibility.
Immune System Dysfunction
Some scientists believe that in endometriosis, the immune system fails to recognize and destroy misplaced endometrial cells. Instead of being eliminated, these cells survive, implant, and proliferate.
Hormonal Influence
Endometriosis is estrogen-dependent, meaning it thrives in environments where estrogen is present. Higher levels of this hormone stimulate the growth and persistence of endometrial-like tissue outside the uterus.
Stem Cell and Embryonic Theories
Some researchers suggest that endometriosis may arise from stem cells that differentiate abnormally, or from remnants of embryonic tissue that develop into endometrial lesions later in life.
Environmental Factors
Exposure to certain environmental toxins, such as dioxins, has been proposed as a risk factor. These substances may disrupt hormonal balance or impair immune function, though evidence is still being studied.
In truth, no single theory explains all cases. Endometriosis is likely multifactorial—a puzzle where genetics, immunity, hormones, and environment all play roles.
Symptoms of Endometriosis: Recognizing the Warning Signs
Endometriosis manifests differently from person to person. Some individuals experience excruciating pain, while others may have minimal symptoms but still face fertility challenges. The variability makes diagnosis complex.
The hallmark symptom is pelvic pain, especially linked to menstruation, but it is important to recognize the wider spectrum of signs:
- Painful periods (dysmenorrhea): Cramping and pain that may begin before menstruation and extend well into the cycle. The pain is often far worse than typical menstrual cramps.
- Chronic pelvic pain: Discomfort or pain in the pelvis that may persist throughout the month.
- Pain during intercourse (dyspareunia): Deep pain during or after sex is common due to endometrial growths on pelvic structures.
- Pain with bowel movements or urination: This may occur especially during menstruation if lesions are present on the bladder or intestines.
- Heavy menstrual bleeding (menorrhagia): Some individuals experience unusually heavy or prolonged periods.
- Infertility: Endometriosis can damage reproductive structures, interfere with ovulation, or cause inflammation that makes conception difficult.
- Other symptoms: Fatigue, bloating, nausea, or digestive issues (often leading to misdiagnosis as irritable bowel syndrome).
It is important to note that symptom severity does not always correlate with disease severity. Someone with extensive endometriosis may have little pain, while another with minimal lesions may experience severe pain.
Diagnosis: Why Endometriosis Is Often Missed
One of the greatest challenges in managing endometriosis is its diagnosis. On average, it can take 7 to 10 years from the onset of symptoms for a patient to receive an accurate diagnosis.
Several factors contribute to this delay:
- Menstrual pain is often normalized and dismissed by society and even by healthcare providers.
- Symptoms overlap with other conditions like pelvic inflammatory disease, ovarian cysts, or irritable bowel syndrome.
- Diagnostic confirmation requires surgical intervention, which is invasive and not always accessible.
Medical History and Physical Exam
The diagnostic journey usually begins with a detailed discussion of symptoms and a pelvic exam. While this can reveal areas of tenderness or masses, it cannot confirm endometriosis.
Imaging Tests
Ultrasound, especially transvaginal ultrasound, can help identify cysts associated with endometriosis (endometriomas). MRI scans may also be used to visualize pelvic structures in more detail. However, these imaging techniques cannot detect all lesions.
Laparoscopy: The Gold Standard
The only definitive way to diagnose endometriosis is through laparoscopy, a minimally invasive surgical procedure. A surgeon inserts a small camera through an incision in the abdomen to directly view and sometimes biopsy suspicious tissue. This not only confirms the diagnosis but also allows for removal of lesions during the same procedure.
Treatment of Endometriosis: Managing a Lifelong Condition
There is currently no cure for endometriosis, but a range of treatments can manage symptoms, improve quality of life, and address infertility. Treatment depends on the severity of symptoms, the patient’s age, and reproductive goals.
Pain Management
Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen are often used to reduce pain and inflammation. While helpful for some, they may not be sufficient for severe cases.
Hormonal Therapies
Because endometriosis is hormone-dependent, therapies that regulate or suppress hormones are a cornerstone of treatment. Options include:
- Combined oral contraceptives: Birth control pills that reduce or eliminate menstruation, thereby decreasing pain.
- Progestins and progesterone-releasing IUDs: These suppress endometrial growth.
- GnRH agonists and antagonists: These drugs induce a temporary “medical menopause,” drastically lowering estrogen levels and shrinking endometrial tissue.
- Aromatase inhibitors: Less commonly used but effective in lowering estrogen production.
These therapies help manage symptoms but do not cure the condition, and symptoms often return once treatment stops.
Surgical Options
Surgery plays a crucial role in diagnosis and treatment.
- Laparoscopic excision or ablation: Surgeons remove or destroy endometrial implants, adhesions, and cysts. This can significantly relieve pain and improve fertility.
- Hysterectomy: In severe cases where other treatments fail, removal of the uterus—and sometimes the ovaries—may be considered. However, this is a last resort, particularly for those who wish to preserve fertility.
Fertility Treatments
For patients struggling with infertility, assisted reproductive technologies like in vitro fertilization (IVF) can bypass some of the barriers caused by endometriosis. Surgery to remove lesions may also improve the chances of natural conception.
Lifestyle and Complementary Approaches
Although medical and surgical treatments are central, many patients find additional relief through holistic approaches:
- Regular exercise and stress management techniques (yoga, meditation, deep breathing).
- Anti-inflammatory diets rich in whole foods, omega-3 fatty acids, and reduced processed sugar.
- Heat therapy, acupuncture, or physical therapy for pelvic floor dysfunction.
These do not replace medical treatments but can provide valuable complementary support.
Living With Endometriosis: Resilience and Advocacy
Endometriosis is not a condition with quick fixes. It often requires long-term management and adjustment. Yet, with proper care, many individuals can lead fulfilling lives.
Support groups and advocacy organizations play an essential role in breaking the silence around the disease. By sharing stories, raising awareness, and pushing for better research, the global endometriosis community is slowly dismantling the stigma that has long surrounded the condition.
Resilience is at the heart of living with endometriosis. It is about finding strategies that work, building supportive relationships, and not allowing the disease to define identity or limit dreams.
The Future of Endometriosis Research
Despite being common, endometriosis remains underfunded and underresearched. However, recent years have seen growing momentum in scientific exploration. Researchers are working to:
- Develop less invasive diagnostic tools, such as blood tests or biomarkers.
- Understand the genetic and immune mechanisms that drive the disease.
- Create targeted therapies that shrink or eliminate lesions without severe side effects.
The future holds promise, but it also requires sustained investment, both financial and societal, in recognizing endometriosis as a serious health condition worthy of attention.
Conclusion: A Call for Awareness and Compassion
Endometriosis is more than just a gynecological disorder—it is a condition that touches every aspect of life, from physical pain to emotional well-being and social participation. Its causes are complex, its symptoms diverse, and its treatments often imperfect. Yet, understanding and compassion can transform the journey.
Raising awareness, advocating for earlier diagnosis, investing in research, and providing comprehensive treatment options are not just medical goals—they are moral imperatives. Every person living with endometriosis deserves to have their pain validated, their health prioritized, and their life supported.
Endometriosis is not simply about surviving monthly cycles of pain; it is about reclaiming the possibility of a full, thriving life.