Polycystic Ovary Syndrome, or PCOS, is more than just a medical diagnosis. It is a journey that millions of women around the world are walking every day—often silently, sometimes in frustration, and always in search of answers. For some, PCOS means months of missed periods, unexplained weight gain, or acne that won’t go away. For others, it is the heartbreaking struggle with infertility or the worry of long-term health risks like diabetes and heart disease.
Yet, PCOS is also a story of resilience. It is about women learning to understand their bodies in new ways, advocating for better care, and finding hope through treatment, lifestyle changes, and community. To truly understand PCOS, we must go beyond symptoms and statistics. We must see it as both a biological condition and a lived experience that affects health, identity, and quality of life.
What Is PCOS?
Polycystic Ovary Syndrome is a complex hormonal disorder that affects people with ovaries, most often during their reproductive years. It is one of the most common endocrine disorders in women, with estimates suggesting that between 6% and 15% of women worldwide may be affected, depending on the diagnostic criteria used.
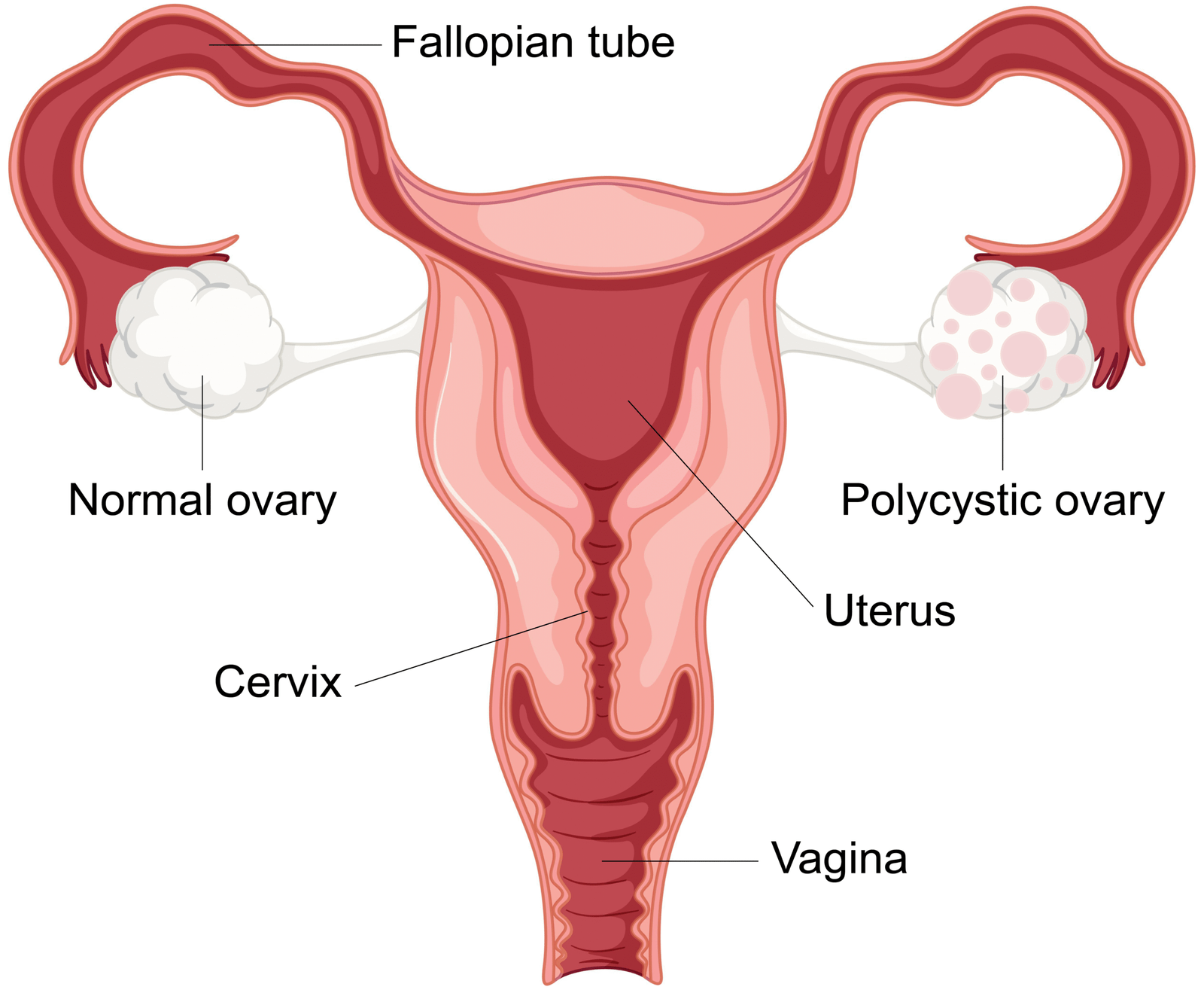
The name itself can be misleading. “Polycystic” refers to the presence of multiple small cysts on the ovaries, but not every woman with PCOS develops these cysts. In fact, the condition is less about cysts and more about hormonal imbalance—particularly excess androgens (male hormones such as testosterone) and problems with ovulation.
PCOS is a syndrome rather than a single disease, meaning it is defined by a cluster of symptoms that vary widely from person to person. Some women may experience irregular cycles but little else. Others may deal with multiple symptoms affecting their skin, weight, metabolism, and fertility.
The Hormonal Imbalance at the Heart of PCOS
At its core, PCOS is a condition of disrupted hormone signaling. In a healthy cycle, hormones from the brain coordinate with the ovaries to regulate ovulation and menstrual bleeding. In PCOS, this communication is impaired.
The ovaries often produce higher-than-normal levels of androgens. While androgens are present in all women in small amounts, excess levels can interfere with the development and release of eggs (ovulation). Instead of a mature egg being released, many follicles may remain underdeveloped—appearing as “cysts” on an ultrasound.
Another key factor is insulin resistance. Many women with PCOS have cells that do not respond properly to insulin, the hormone that regulates blood sugar. As a result, the body compensates by producing more insulin. High insulin levels, in turn, stimulate the ovaries to produce more androgens, creating a vicious cycle that worsens symptoms.
This combination of insulin resistance and excess androgens explains much of PCOS’s complexity, linking reproductive issues with metabolic and dermatological symptoms.
Causes of PCOS: Untangling a Web of Factors
The exact cause of PCOS remains uncertain, but researchers believe it arises from an interplay of genetic, hormonal, and environmental influences.
Genetic Susceptibility
PCOS tends to run in families, suggesting a strong genetic component. Women with mothers or sisters who have PCOS are more likely to develop it themselves. However, no single “PCOS gene” has been identified. Instead, multiple genes appear to influence hormone regulation, insulin sensitivity, and ovarian function.
Hormonal Dysregulation
Abnormal levels of luteinizing hormone (LH) and follicle-stimulating hormone (FSH) may disrupt normal ovulation. Elevated LH promotes androgen production in the ovaries, contributing to the imbalance seen in PCOS.
Insulin Resistance and Lifestyle Factors
Insulin resistance is both a cause and a consequence of PCOS. It may be influenced by genetics but is also strongly affected by lifestyle—diet, physical activity, and body weight. Notably, women of all body sizes can develop PCOS, but excess body fat can exacerbate hormonal disruptions.
Environmental Influences
Some studies suggest that endocrine-disrupting chemicals (such as BPA found in plastics) may play a role in altering hormonal balance, though evidence is still emerging. Stress, sleep patterns, and diet are also being studied as contributing factors.
Symptoms of PCOS: A Spectrum of Experiences
PCOS manifests differently in every woman, which is why it often goes undiagnosed or misdiagnosed for years.
Menstrual Irregularities
The most common symptom is irregular or absent periods, caused by lack of consistent ovulation. Some women may have cycles spaced more than 35 days apart, while others may have fewer than eight periods per year.
Infertility
Because ovulation is unpredictable or absent, PCOS is one of the leading causes of infertility. However, it does not mean pregnancy is impossible; many women with PCOS conceive naturally or with medical assistance.
Signs of Hyperandrogenism
Excess androgens can cause physical changes such as acne, oily skin, excessive facial or body hair (hirsutism), and thinning hair on the scalp (androgenic alopecia). These symptoms can significantly affect self-esteem and emotional well-being.
Polycystic Ovaries
On ultrasound, some women with PCOS have enlarged ovaries with multiple small follicles. However, not all women with these “polycystic” ovaries have PCOS, and not all women with PCOS have this feature.
Metabolic Issues
Insulin resistance can lead to weight gain, particularly around the abdomen. Women with PCOS are at higher risk for type 2 diabetes, high cholesterol, and high blood pressure.
Emotional and Psychological Impact
The effects of PCOS extend beyond physical health. Anxiety, depression, and low self-esteem are common, driven both by hormonal influences and the challenges of managing chronic symptoms.
Diagnosis of PCOS: A Puzzle with Many Pieces
Diagnosing PCOS can be challenging, as no single test confirms it. Doctors typically use a combination of medical history, physical examination, blood tests, and imaging.
The most widely used criteria are the Rotterdam criteria, which state that a diagnosis of PCOS requires at least two of the following three features:
- Irregular or absent ovulation
- Clinical or biochemical signs of excess androgens
- Polycystic ovaries on ultrasound
Before confirming PCOS, other conditions that mimic its symptoms (such as thyroid disorders, hyperprolactinemia, or adrenal disorders) must be ruled out.
Blood tests may measure hormone levels (testosterone, LH, FSH, prolactin, thyroid hormones) and assess metabolic health (glucose tolerance, cholesterol). An ultrasound may reveal enlarged ovaries with multiple small follicles, but as noted, this feature alone is not sufficient for diagnosis.
Treatment of PCOS: A Multifaceted Approach
There is no single cure for PCOS, but it can be managed effectively through a combination of lifestyle changes, medication, and supportive care tailored to each woman’s needs.
Lifestyle Management
Healthy lifestyle choices are the cornerstone of PCOS management, especially for women with insulin resistance.
- Nutrition: A balanced diet rich in whole grains, lean proteins, healthy fats, fruits, and vegetables can stabilize blood sugar and support hormone regulation. Reducing processed foods and added sugars is particularly helpful.
- Physical Activity: Regular exercise improves insulin sensitivity, promotes weight management, and reduces cardiovascular risk. Both aerobic activities and strength training are beneficial.
- Weight Management: For women who are overweight, even modest weight loss (5–10% of body weight) can improve menstrual regularity and fertility.
Medications
Doctors may prescribe different medications depending on the woman’s primary concerns.
- Hormonal Birth Control: Pills, patches, or intrauterine devices can regulate menstrual cycles, reduce androgen levels, and improve acne and hirsutism.
- Metformin: Originally a diabetes drug, metformin improves insulin sensitivity and may help regulate periods and promote weight loss.
- Fertility Treatments: For women trying to conceive, medications like clomiphene citrate or letrozole can induce ovulation. In some cases, assisted reproductive technologies such as in vitro fertilization (IVF) are used.
- Anti-Androgen Medications: Drugs like spironolactone may reduce unwanted hair growth and acne, though they are not suitable during pregnancy.
Cosmetic and Supportive Treatments
Hair removal methods, dermatological treatments for acne, and counseling for emotional support are often important parts of comprehensive care.
Long-Term Health Risks of PCOS
PCOS is not only about reproductive health. It carries significant long-term risks if not managed properly. Women with PCOS have higher rates of type 2 diabetes, metabolic syndrome, cardiovascular disease, and endometrial cancer.
Mental health risks are equally important. Chronic stress, body image struggles, and infertility challenges contribute to higher rates of anxiety and depression. A holistic approach to treatment must address both physical and emotional dimensions.
Living with PCOS: Beyond the Medical Model
Living with PCOS is often a daily negotiation—managing symptoms, planning around irregular cycles, and coping with the unpredictability of the condition. Many women find strength in community, whether through support groups, online forums, or advocacy organizations.
Self-care practices—such as mindful eating, stress management techniques, and prioritizing mental health—can make a profound difference. PCOS is not a reflection of personal failure but a medical condition that requires compassion, patience, and persistence.
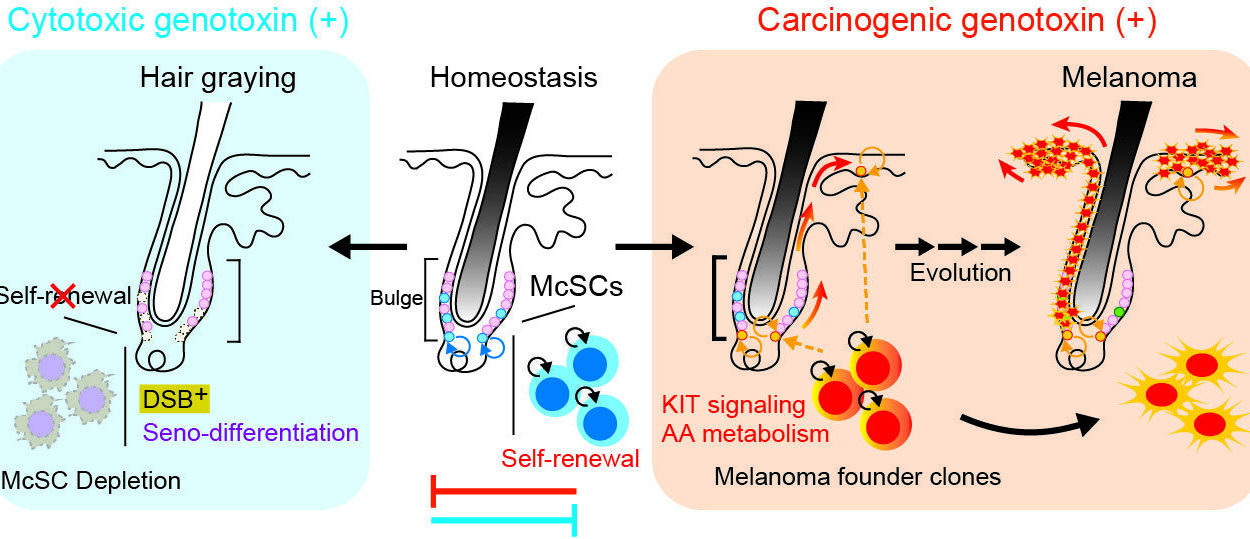
Hope on the Horizon: Research and Innovation
Research on PCOS is expanding, with scientists exploring its genetic roots, immune connections, and links to the gut microbiome. New treatments are being investigated, from inositol supplements to novel fertility therapies. Greater awareness and advocacy are also driving improvements in care, ensuring that women no longer feel dismissed or unheard when they seek help.
PCOS as a Story of Strength
Polycystic Ovary Syndrome is complex, frustrating, and at times overwhelming. But it is also a reminder of human resilience. Women with PCOS navigate not only their bodies’ hormonal storms but also the social and emotional challenges that come with them. In doing so, they are rewriting the narrative—from one of silent struggle to one of strength, knowledge, and empowerment.
PCOS is not the end of possibility. With the right diagnosis, treatment, and support, women with PCOS can lead healthy, fulfilling lives, build families, and protect their long-term health. Understanding PCOS fully—its causes, symptoms, diagnosis, and treatment—is the first step in replacing confusion with clarity, fear with confidence, and isolation with solidarity.