For decades, breast cancer research has been a story of progress mingled with heartbreak. Screening tools have become more precise, treatments more effective, and survival rates steadily higher. Yet for many survivors, even after the cheers and tears of finishing treatment, one haunting question remains: Will my cancer come back?
For about 30% of breast cancer survivors, the answer is tragically yes. When relapse happens, it is often incurable, requiring lifelong therapy that manages—but never eliminates—the disease. This shadow of recurrence hangs over survivors, sometimes for years or even decades, silently shaping their lives.
Now, for the first time, a groundbreaking clinical trial led by researchers at the Abramson Cancer Center of the University of Pennsylvania and Penn’s Perelman School of Medicine has offered a glimmer of hope against this silent threat. Published in Nature Medicine, the study demonstrates that dormant cancer cells—the stealthy seeds of recurrence—can not only be detected, but also effectively treated with repurposed drugs that are already available.
The findings suggest something once unthinkable: the possibility of stopping breast cancer relapse before it ever happens.
The Hidden Enemy: Dormant Tumor Cells
Cancer does not always die when treatment ends. In some survivors, tiny clusters of cells linger quietly in the body. These “sleeper cells,” also known as minimal residual disease (MRD), lie dormant in tissues such as bone marrow, invisible to scans and undetectable through standard follow-up tests.
The danger is not immediate. These cells may remain silent for years, even decades. But at any moment, they can “wake up,” multiply, and spread, triggering metastatic breast cancer—the incurable stage of the disease.
Different subtypes of breast cancer relapse on different timelines. Aggressive types like triple-negative and HER2+ often return within a few years, while estrogen receptor-positive (ER+) breast cancers may resurface 10, 20, or even 30 years later. The unpredictability has left patients and doctors alike in limbo, without a way to know who is truly cancer-free and who is carrying hidden threats.
“The lingering fear of cancer returning is something that hangs over many breast cancer survivors after they celebrate the end of treatment,” explained Dr. Angela DeMichele, the principal investigator of the study. “Right now, we just don’t know when or if someone’s cancer will come back—that’s the problem we set out to solve.”
A Surprising Weakness in Cancer’s Armor
The new study reveals an unexpected insight: dormant cancer cells are biologically distinct from active tumor cells.
Dr. Lewis Chodosh, chair of Cancer Biology at Penn and senior author of the study, has spent years studying the unique biology of these sleeper cells. His earlier work uncovered that dormant cells survive by relying on specific survival pathways—autophagy (a kind of cellular recycling process) and mTOR signaling (a pathway that regulates cell growth and metabolism).
What’s remarkable is that drugs already approved by the FDA for other conditions can target these very pathways. And unlike standard cancer drugs, which fail against actively growing tumors, these drugs appear to work specifically against dormant cells.
“Surprisingly, we’ve found that certain drugs that ‘don’t’ work against actively growing cancers can be very effective against these sleeper cells,” said Chodosh. “This tells us that the biology of dormant tumor cells is very different from active cancer cells.”
In preclinical experiments with mice, these repurposed drugs successfully eliminated MRD, prolonging survival and preventing recurrence. The discovery opened the door to a bold new clinical strategy: treating breast cancer while it’s “sleeping.”
The CLEVER Trial: Turning Science into Hope
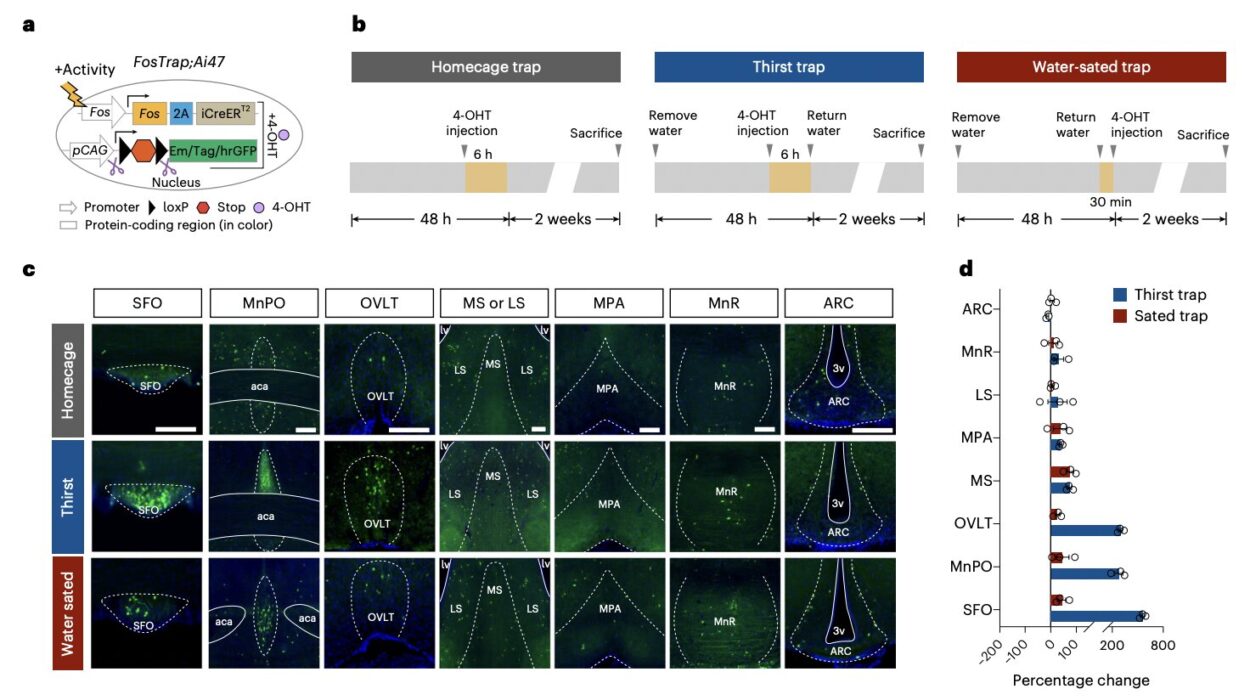
Building on these insights, the team launched the CLEVER clinical trial (a randomized Phase II study) to test whether dormant cancer cells could be cleared in human survivors.
The trial enrolled 51 breast cancer survivors who had completed treatment within the past five years and showed no signs of disease on standard scans. Researchers screened participants’ bone marrow for dormant tumor cells, identifying those with MRD.
Patients with MRD were randomly assigned to receive six cycles of treatment with either:
- one of the repurposed drugs, or
- a combination of both drugs.
The results were remarkable. Dormant tumor cells were successfully cleared in 80% of participants after six to twelve months of treatment. Even more striking were the long-term outcomes:
- Patients who received one drug had a three-year recurrence-free survival rate of over 90%.
- Patients who received both drugs had a recurrence-free survival rate of 100%.
After a median follow-up of 42 months, only two patients experienced a recurrence.
For survivors who have lived with the constant uncertainty of relapse, these numbers are nothing short of extraordinary.
Moving Beyond “Wait and See”
Until now, the standard approach after breast cancer treatment has been vigilance: regular scans, check-ups, and the agonizing wait for any signs of recurrence. For patients with MRD, there was no option other than to hope their cancer never resurfaced.
Dr. DeMichele emphasized that this study marks a pivotal shift. “We want to be able to give patients a better option than ‘wait and see’ after they complete breast cancer treatment. We’re encouraged by these results that we’re on the right track.”
The CLEVER trial is just the beginning. Larger trials—such as the ABBY and PALAVY clinical studies—are already underway across multiple cancer centers to validate and expand on these findings. If successful, they could lead to a new standard of care: detecting and eliminating dormant cancer cells before they become deadly.
The Human Impact: Living Without the Shadow
Beyond the science, this breakthrough touches something deeply human: peace of mind.
Every cancer survivor knows the strange mix of joy and fear that comes with the end of treatment. Ringing the bell to mark the final chemotherapy session, or hearing the words “no evidence of disease,” is a powerful milestone. But often, joy is tempered by a quiet anxiety: What if it comes back?
By giving survivors a real chance to eliminate the invisible threat of dormant cells, this new approach doesn’t just extend survival—it restores hope. It allows patients to envision a future free from the shadow of recurrence, where cancer is truly behind them, not lurking just out of sight.
A Glimpse Into the Future of Cancer Treatment
The significance of this trial goes beyond breast cancer. If dormant cells can be identified and treated in breast cancer survivors, the same strategy could potentially apply to other cancers known to recur years later, such as prostate, ovarian, or melanoma.
The idea of treating cancer during its “silent phase” represents a paradigm shift. It suggests that one day, we might move from simply managing advanced cancer to preventing it altogether.
For now, the CLEVER trial represents a first, crucial step. It proves that the biology of dormancy can be exploited, that MRD can be detected in real time, and that we may already have the tools—hidden in plain sight among existing drugs—to fight back.
More information: Targeting dormant tumor cells to prevent recurrent breast cancer: a randomized phase 2 trial, Nature Medicine (2025). DOI: 10.1038/s41591-025-03877-3