For nearly two decades, a couple had lived through the heartbreak that so many others know all too well—the endless cycles of hope and disappointment that accompany infertility. After years of failed treatments, countless appointments, and emotional exhaustion, they were told what no one wanting a child wants to hear: there was little to no chance of having a biological baby.
Yet, against the odds, hope was reborn—not through luck, but through science. At Columbia University’s Fertility Center, researchers achieved something that once seemed impossible: the world’s first successful pregnancy using an AI-guided technique to find viable sperm in a man with azoospermia, a condition in which semen contains no detectable sperm. This extraordinary achievement, detailed in The Lancet, represents a profound leap forward in reproductive medicine and the power of human innovation.
Understanding the Challenge of Male Infertility
Infertility affects millions of couples worldwide, and in roughly 40% of these cases, the cause lies with male factors. For men with azoospermia, the situation is especially heartbreaking. Despite normal-looking semen samples, a closer look under the microscope reveals a field devoid of life—no visible sperm, only cellular debris.
Dr. Zev Williams, Director of the Columbia University Fertility Center and senior author of the study, explains, “A semen sample can appear totally normal, but when you look under the microscope you discover just a sea of cellular debris, with no sperm visible. Many couples with male-factor infertility are told they have little chance of having a biological child.”
For decades, the only options for such men were invasive surgical procedures that attempted to extract sperm directly from the testes. These methods, though sometimes successful, were painful, expensive, and carried risks of inflammation, vascular injury, and temporary hormonal imbalance. For many, they yielded nothing at all.
Meanwhile, technicians in a handful of specialized labs would manually comb through processed semen samples under powerful microscopes, searching for even a single viable sperm. It was a process that could take hours—or even days—requiring skill, patience, and a fair bit of luck. And still, most searches ended in failure.
The challenge was clear: finding a better way to detect the rare, viable sperm cells that might still exist in men with azoospermia—without destroying them in the process.
The Birth of a New Idea
The solution began with a team of dreamers—scientists and clinicians at Columbia University who refused to accept the limits of current methods. Led by Dr. Williams and assisted by Dr. Hemant Suryawanshi, an assistant professor of reproductive sciences, they brought together experts in advanced imaging, microfluidics, and reproductive endocrinology. Their mission was as simple as it was monumental: find a way to detect the undetectable.
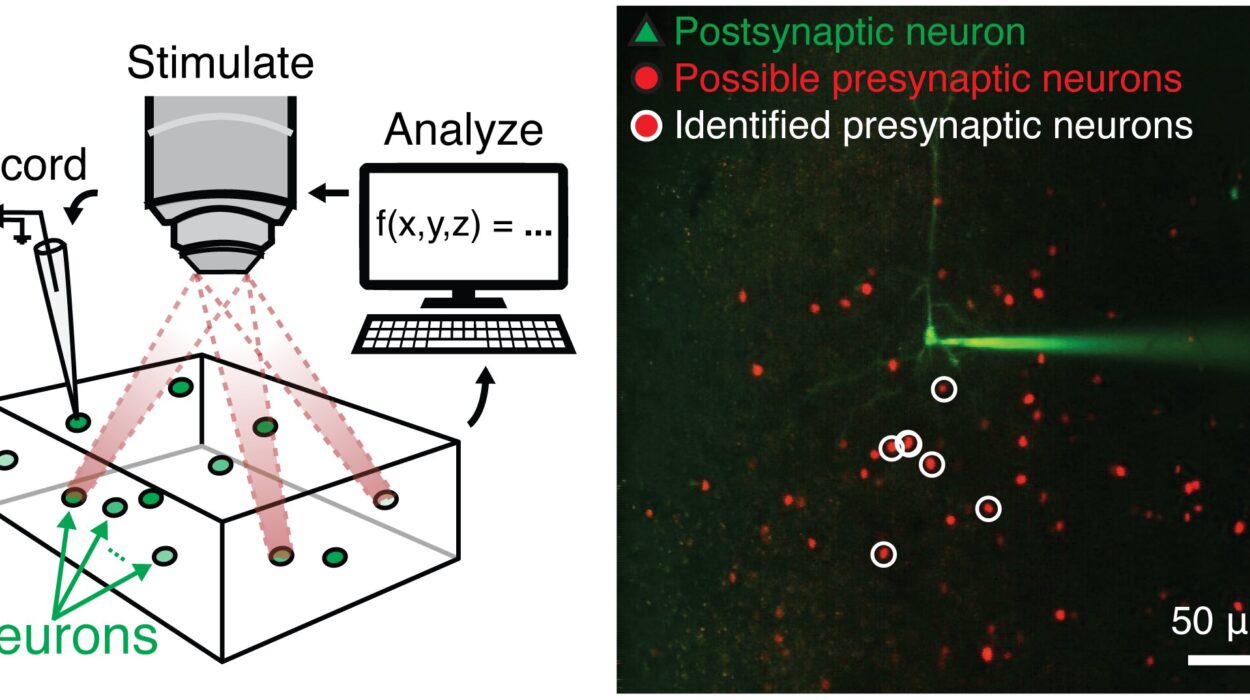
The result of their collaboration was a revolutionary technique known as STAR, short for Sperm Tracking and Recovery. This method would harness the combined power of artificial intelligence, robotics, and high-speed imaging to do what the human eye and hand could not—search through millions of microscopic images and isolate a living sperm cell, all in a fraction of the time.
“Our team included experts in advanced imaging techniques, microfluidics, and reproductive endocrinology to tackle each individual step required to find and isolate rare sperm,” says Dr. Suryawanshi. The result was a seamless integration of biology and technology—one that could redefine the possibilities of human reproduction.
How STAR Works: The Marriage of AI and Biology
The STAR system works much like an incredibly patient, tireless scientist. It begins by scanning a semen sample from a man with azoospermia, capturing over eight million high-resolution images in under an hour. Where a human technician might search manually for hours and still miss the target, STAR’s artificial intelligence algorithms analyze these millions of frames, looking for the distinctive shapes and movements of sperm cells hidden among debris.
Once the AI identifies a potential sperm, the system uses a microfluidic chip—a device embedded with tiny, hair-like channels—to isolate the exact region of the sample containing the sperm cell. Then, within milliseconds, a robotic arm gently retrieves the cell, ensuring it remains viable for use in fertilization.
This combination of AI precision, microengineering, and robotic delicacy allows scientists to do what once seemed impossible: recover living sperm from samples that appeared completely sterile.
The process is also fast, efficient, and far less damaging than traditional centrifuge-based methods, which often harm fragile sperm cells. In the hands of researchers at Columbia, STAR became not just a technological marvel but a beacon of hope.
The First STAR Baby
The technology was put to the test in one of the most challenging cases imaginable—a couple who had spent nearly 20 years trying to conceive. The man had undergone multiple IVF cycles at different centers, several exhaustive manual sperm searches, and even two surgical extractions. Each time, the result was the same: no viable sperm, no embryo, no child.
But with STAR, everything changed.
When the patient provided a 3.5 milliliter semen sample, the AI-powered system went to work. Over the course of about two hours, it analyzed 2.5 million images and identified two living sperm cells. That’s all—two cells in millions of frames of cellular debris.
Those two cells were then carefully retrieved and used to fertilize two eggs. The result was nothing short of miraculous: both embryos developed successfully, and one led to a healthy pregnancy—the first in the world achieved through an AI-guided sperm recovery method.
“You only need one healthy sperm to create an embryo,” Dr. Williams said. For this couple, one was enough to make their dream come true.
A Breakthrough With Global Implications
While this first success involved just a single case, the implications are vast. If larger studies confirm the effectiveness of STAR, it could transform the treatment of male infertility worldwide. Millions of men diagnosed with azoospermia may soon have a chance—perhaps for the first time—to father a biological child.
What makes STAR especially promising is that it is non-invasive and scalable. Unlike surgical extraction, it does not damage tissue or disrupt hormonal balance. Its use of artificial intelligence also means that it can analyze samples more accurately and efficiently than human technicians, potentially making fertility treatments more accessible and less expensive in the long run.
Beyond clinical applications, STAR represents a remarkable example of how technology can enhance the deepest human experiences—hope, love, and creation. It blurs the line between science and miracle, showing how innovation can heal not just bodies, but hearts.
The Human Side of a Technological Revolution
Behind every scientific milestone are real people—researchers, patients, families—whose dedication and perseverance make the impossible possible. For the Columbia team, STAR was more than an experiment. It was a mission to give families hope where there had been none.
For the couple at the heart of this story, the success is deeply personal. Their journey through nearly two decades of infertility embodies what countless others endure: the rollercoaster of emotions, the physical strain, the financial burden, and the quiet grief of unfulfilled dreams. To have that pain answered by a child’s heartbeat is a testament to both human resilience and scientific brilliance.
For Dr. Williams and his team, this success is only the beginning. “The field has really been challenged to find a better way to identify and retrieve viable sperm cells in men with exceedingly low sperm counts,” he said. “This technology offers a real path forward.”
The Future of Fertility Science
The STAR technique is now being tested in larger clinical trials to determine its broader efficacy and reliability. If results continue to be positive, AI-guided sperm recovery could become a standard part of fertility treatments for men with severe infertility.
As technology continues to advance, AI may soon assist in every stage of assisted reproduction—from identifying viable sperm and eggs to predicting embryo success rates and optimizing implantation. In a future where human life begins at the intersection of compassion and computation, breakthroughs like STAR remind us that technology’s greatest power lies not in replacing humanity, but in restoring it.
More information: First clinical pregnancy following AI-based microfluidic sperm detection and recovery in non-obstructive azoospermia, The Lancet (2025). DOI: 10.1016/S0140-6736(25)01623-X