You may look in the mirror every day and see your face, your skin, your outer self staring back. But how often do you stop to wonder about the incredible organ that is your skin? It protects you, cools you, senses your world, and heals itself. And yet, for most of us, it’s something we notice only when it’s itching, breaking out, or turning red.
Welcome to the world of dermatology—a specialized branch of medicine that deals with the science, structure, function, and diseases of the skin, hair, nails, and mucous membranes. Far more than simply treating acne or prescribing creams, dermatology is at the intersection of aesthetics, internal medicine, pathology, immunology, and surgery. It is a discipline that helps maintain the physical and emotional health of individuals across the world.
In this article, we will journey into the fascinating realm of dermatology, uncovering how our skin works, what makes it suffer, how it heals, and how medical science is continually pushing the boundaries to keep it healthy and beautiful. Prepare to discover that dermatology isn’t just skin-deep—it’s profoundly human.
The Skin: Your Body’s Living Armor
To understand dermatology, you must first appreciate the skin itself. The skin is not a simple covering—it’s the largest and one of the most complex organs in the human body. On average, it accounts for about 16% of your body weight and spans approximately 20 square feet in adults.
It has three primary layers:
Epidermis: The outermost layer, which serves as a barrier against environmental damage, microbes, and dehydration. It contains keratinocytes (which produce keratin), melanocytes (which produce pigment), and immune cells.
Dermis: The middle layer, filled with collagen, blood vessels, nerves, sweat glands, sebaceous glands (which produce oil), and hair follicles. It gives the skin its elasticity and strength.
Hypodermis (or subcutaneous layer): A deeper layer made mostly of fat and connective tissue that insulates the body and cushions internal organs.
This trilayered structure is more than anatomy. It’s an ecosystem—a living, breathing interface between you and the world. The skin protects, senses, regulates, and even communicates. It can flush in anger, pale in fear, or sweat with anxiety. Through it, you feel heat, pain, pleasure, and danger.
Dermatology, then, is the study of how this miraculous organ functions and fails—and how to preserve and restore it.
A Brief History of Dermatology: From Ancient Remedies to Modern Science
Dermatology is not a modern invention. Humans have always been aware of skin diseases. Ancient Egyptian, Greek, Chinese, and Ayurvedic texts describe treatments for leprosy, psoriasis, rashes, and boils. Clay masks, herbal pastes, and mineral applications were some of the earliest forms of dermatologic therapy.
The term “dermatology” derives from the Greek derma (skin) and logos (study). But it wasn’t until the 18th and 19th centuries that dermatology began to evolve as a distinct medical discipline. French physicians like Jean-Louis Alibert and British doctors such as Robert Willan were pioneers in classifying skin diseases systematically. By the 20th century, dermatology had blossomed into a full-fledged medical specialty with subspecialties including surgical, pediatric, and cosmetic dermatology.
Today, dermatologists work in clinics, hospitals, research labs, and cosmetic centers around the world. They manage diseases that range from mild and cosmetic to life-threatening and systemic. From treating a simple wart to diagnosing lupus, dermatology spans the full spectrum of medical complexity.
Common Skin Conditions: The Everyday Battles
One of the most visible roles of dermatology is the treatment of common skin conditions, which affect people of all ages, ethnicities, and lifestyles. These conditions may not always be life-threatening, but they can deeply affect a person’s confidence, comfort, and quality of life.
Acne: Perhaps the most well-known skin issue, acne occurs when hair follicles become clogged with oil and dead skin cells. It affects millions, especially teenagers, and can persist into adulthood. Treatments include topical medications, antibiotics, hormonal therapy, and isotretinoin.
Eczema (Atopic Dermatitis): A chronic inflammatory condition characterized by red, itchy, and dry skin. It often appears in early childhood and can flare periodically. The causes are complex, involving genetics, immune dysfunction, and environmental triggers.
Psoriasis: A chronic autoimmune disease where skin cells multiply too quickly, leading to thick, scaly patches. It’s not contagious, but it can be deeply distressing. Psoriasis may also be linked with joint inflammation in a condition known as psoriatic arthritis.
Rosacea: A facial skin disorder that causes redness, visible blood vessels, and sometimes pustules. Though more common in fair-skinned individuals, it can affect anyone and often worsens with triggers like alcohol, heat, and stress.
Fungal Infections: From athlete’s foot to ringworm, fungal infections are common and usually easily treated. They thrive in warm, moist environments and often spread in communal settings.
Vitiligo: A condition where melanocytes (pigment-producing cells) are destroyed, leading to white patches on the skin. It has no known cure and is often emotionally difficult for patients, especially in societies that value uniform skin tone.
Dermatologists are trained to diagnose these and hundreds of other skin conditions, often using nothing more than a visual examination and a patient’s history. When needed, they employ biopsies, lab tests, or imaging to arrive at a diagnosis.
Skin Cancer: Dermatology’s Life-Saving Role
One of the most critical roles of dermatology is the detection and treatment of skin cancer, the most common form of cancer worldwide.
There are several types of skin cancer:
Basal Cell Carcinoma (BCC): The most common but least dangerous. It grows slowly and rarely spreads but can be disfiguring if untreated.
Squamous Cell Carcinoma (SCC): More likely to spread than BCC and typically linked to cumulative sun exposure.
Melanoma: The deadliest form, originating in pigment-producing melanocytes. If caught early, it’s highly curable—but if it spreads, it can be fatal.
Early detection is key. Dermatologists recommend regular skin checks, especially for individuals with fair skin, a history of sunburns, or a family history of skin cancer. They often use tools like dermatoscopes to magnify and examine skin lesions more closely and may take biopsies to confirm a diagnosis.
Treatment options include surgical excision, cryotherapy, topical chemotherapy, Mohs surgery (a tissue-sparing technique), and even immunotherapy in advanced cases.
Pediatric Dermatology: Caring for Young Skin
Children aren’t just miniature adults—their skin is different in structure, sensitivity, and response to disease. Pediatric dermatologists focus on conditions unique to children, such as:
- Infantile hemangiomas (benign blood vessel tumors)
- Diaper rash
- Cradle cap (seborrheic dermatitis)
- Birthmarks
- Genetic skin diseases like epidermolysis bullosa
Early intervention is crucial, both medically and emotionally. Skin conditions in childhood can leave lasting physical and psychological effects, so dermatologists work closely with parents, pediatricians, and specialists to offer compassionate, effective care.
Cosmetic Dermatology: Science Meets Beauty
Beyond treating diseases, dermatology also ventures into the world of cosmetic enhancement. This branch addresses aesthetic concerns like aging, hyperpigmentation, scars, and unwanted hair or fat.
Modern cosmetic dermatology uses advanced tools:
Botulinum toxin (Botox): Temporarily reduces facial wrinkles by relaxing muscles.
Dermal fillers: Injected into the skin to add volume, reduce wrinkles, or enhance features.
Laser therapy: Used to treat scars, sunspots, birthmarks, or vascular lesions.
Chemical peels: Improve skin texture and tone by removing the outermost layers of dead skin.
Microneedling and PRP (Platelet-Rich Plasma): Stimulate collagen production and skin rejuvenation.
While some dismiss cosmetic dermatology as vanity-driven, it can dramatically improve self-esteem and mental health. Treating a disfiguring birthmark, removing severe acne scars, or simply helping someone feel confident in their skin is a legitimate and powerful application of dermatologic science.
Dermatologic Surgery: Precision and Art
In many cases, dermatologists perform surgical procedures. This may involve removing skin cancers, moles, cysts, or performing corrective surgeries.
One of the most celebrated techniques is Mohs Micrographic Surgery, used primarily for treating basal and squamous cell carcinomas. This technique involves removing skin layer by layer and examining each under a microscope until no cancerous cells remain. It offers the highest cure rate and preserves as much healthy tissue as possible—essential for cosmetically sensitive areas like the face.
Other surgical procedures include:
- Scar revision
- Nail surgery
- Excision of lipomas and cysts
- Reconstructive surgery following tumor removal
These procedures require not only medical expertise but a keen eye for detail and aesthetics.
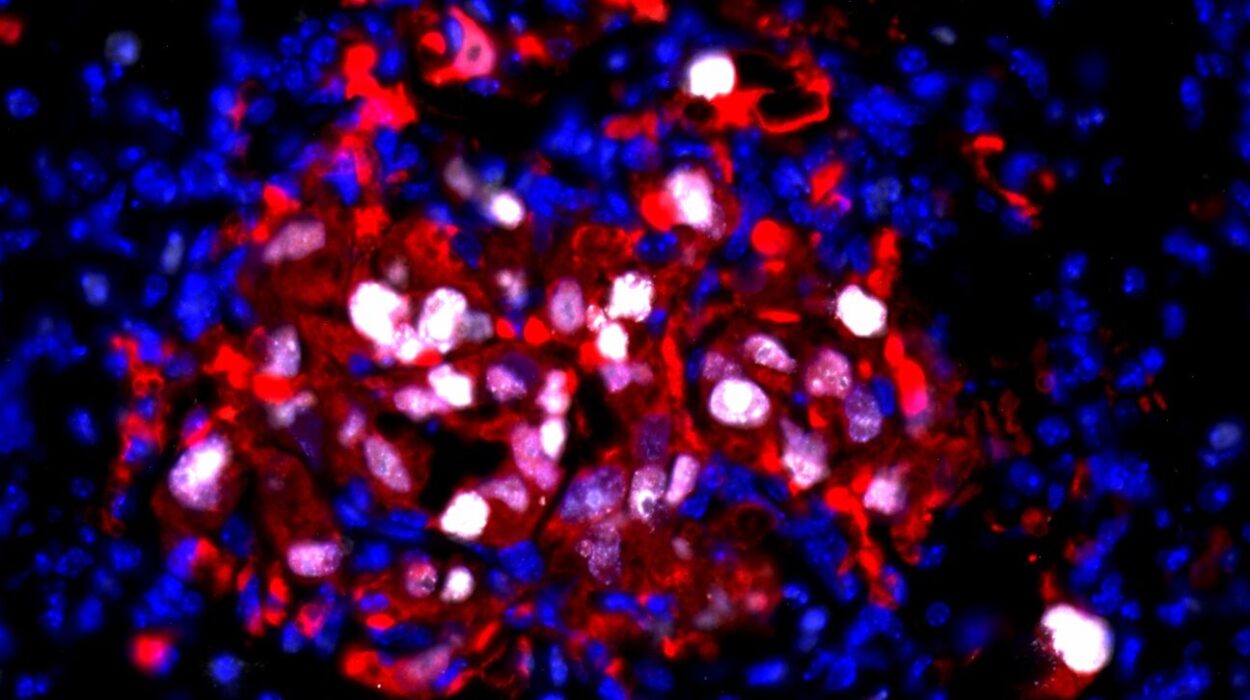
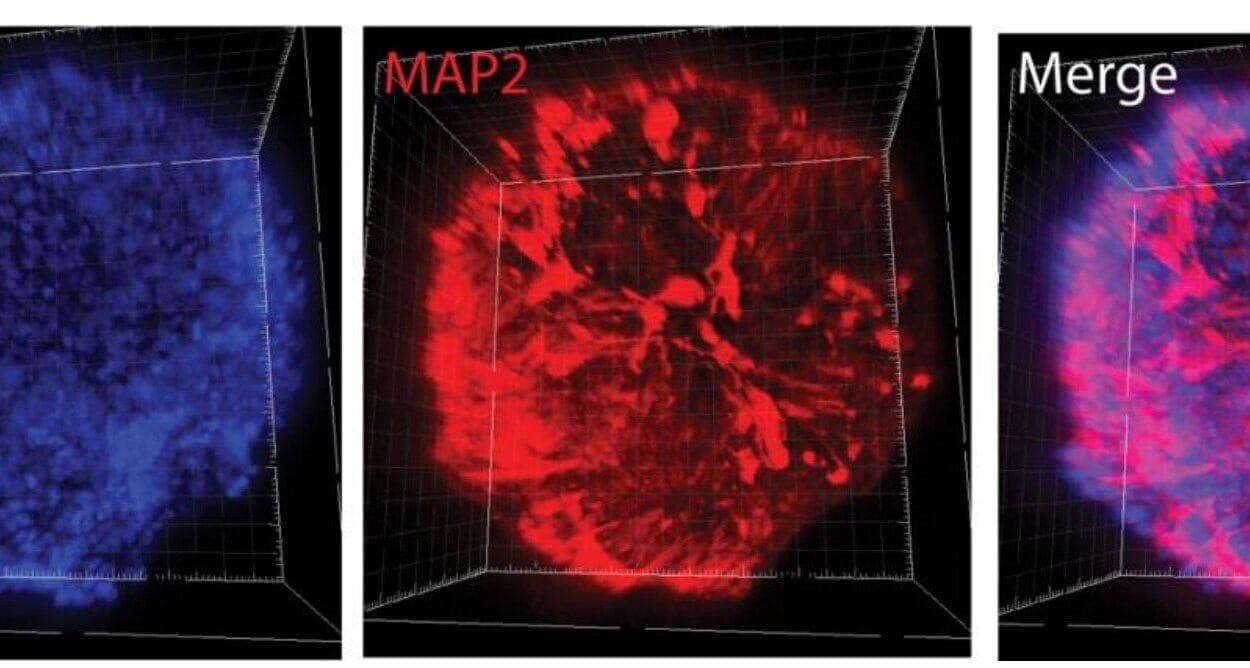
Dermatopathology: Diagnosing Skin Under the Microscope
Some dermatologists specialize in dermatopathology, the microscopic analysis of skin biopsies. By examining tissue samples stained and sliced into thin layers, they can diagnose cancers, infections, autoimmune conditions, and rare skin disorders that defy clinical diagnosis.
This subspecialty requires a deep understanding of both dermatology and pathology, and it plays a vital role in accurate treatment planning. While a rash may look similar on the surface, the cells beneath may tell a very different story.
Psychodermatology: When Mind and Skin Interact
The link between mind and skin is intimate and complex. Stress can trigger flare-ups of psoriasis, eczema, or acne. Depression and anxiety often accompany chronic skin diseases. Some conditions, like trichotillomania (hair-pulling disorder) or delusional parasitosis (false belief of infestation), are psychiatric in nature but manifest on the skin.
Psychodermatology is a growing field that examines the psychological impact of skin disease—and vice versa. Dermatologists in this field often work closely with psychologists and psychiatrists to offer holistic care, treating both the symptom and the source.
Innovations and the Future of Dermatology
Dermatology is evolving rapidly, propelled by advances in genetics, artificial intelligence, regenerative medicine, and biotechnology.
Teledermatology is expanding access to care, especially in underserved areas. Patients can now send images of skin lesions and receive remote diagnoses, speeding up treatment and reducing costs.
Genomic medicine is offering personalized treatment plans based on individual genetic profiles. Conditions like melanoma can now be targeted with precision drugs based on specific mutations.
3D printing and tissue engineering are beginning to offer hope for regenerating skin lost to burns, trauma, or disease.
AI-powered diagnostic tools are being trained to identify skin cancer and other conditions with remarkable accuracy—though human oversight remains critical.
The future of dermatology lies in precision, inclusivity, and integration, with a focus on not only treating disease but enhancing wellness, preventing illness, and celebrating diversity in skin of every shade, texture, and age.
Conclusion: A Science of Humanity
Dermatology is a mirror to our inner and outer lives. It reflects our genetics, our environments, our emotions, and even our cultures. Whether through the treatment of a simple rash or the management of a life-threatening cancer, dermatology connects biology with identity, medicine with beauty, and science with soul.
To study skin is to study life itself—not just the surface, but the layers that make us who we are.
So the next time you look in the mirror, take a moment to appreciate the masterpiece that is your skin—and the science that helps keep it healthy, radiant, and uniquely yours.