In the United States, a quiet but potent public health intervention has been flowing through our taps for nearly 80 years. Since 1945, fluoride has been added to community water systems to protect teeth from decay—a measure so widespread and normalized that most Americans hardly give it a second thought. But what if that were to change? What if, tomorrow, fluoride disappeared from every faucet in America?
A new, data-rich study from researchers at Mass General Brigham, published in JAMA Health Forum, offers a sobering answer. Using a high-powered simulation model based on national health data, the team projected the dental, financial, and quality-of-life costs if fluoride were to vanish from public water systems. The findings are striking: without fluoridation, the nation’s children—especially those who are publicly insured or uninsured—could face a dramatic rise in tooth decay, with billions in added dental care costs.
Why Fluoride? A Public Health Success Story
To understand the implications of removing fluoride, it’s important to recognize how it works—and why it’s been hailed as one of the greatest public health achievements of the 20th century.
“Fluoride replaces weaker ions within tooth enamel, making it stronger and less susceptible to tooth decay caused by bacteria,” explains Dr. Lisa Simon, MD, DMD, senior author of the study and a physician at Brigham and Women’s Hospital. When children consume fluoride—primarily through drinking water—it integrates into their developing teeth, fortifying enamel even before the teeth emerge. Once the teeth are in, fluoride continues to act as a shield, making them more resistant to the acids produced by cavity-causing bacteria.
The benefits of fluoride are particularly pronounced in children, whose teeth are still forming and who often lack regular access to comprehensive dental care. This is especially true in lower-income communities, where disparities in oral health outcomes remain stark.
A Natural Experiment in Canada
The warning signs of removing fluoride are not theoretical. Calgary, Canada, provides a real-world example. After discontinuing water fluoridation in 2011, the city saw a notable increase in childhood tooth decay. Other cities and countries that have rolled back fluoridation have reported similar trends.
“We have strong comparative data from places like Calgary, which show that when fluoride is eliminated, dental disease increases,” says Simon. “Our study offers a window into what might happen in the U.S. if water fluoridation ceased.”
Modeling the Dental Domino Effect
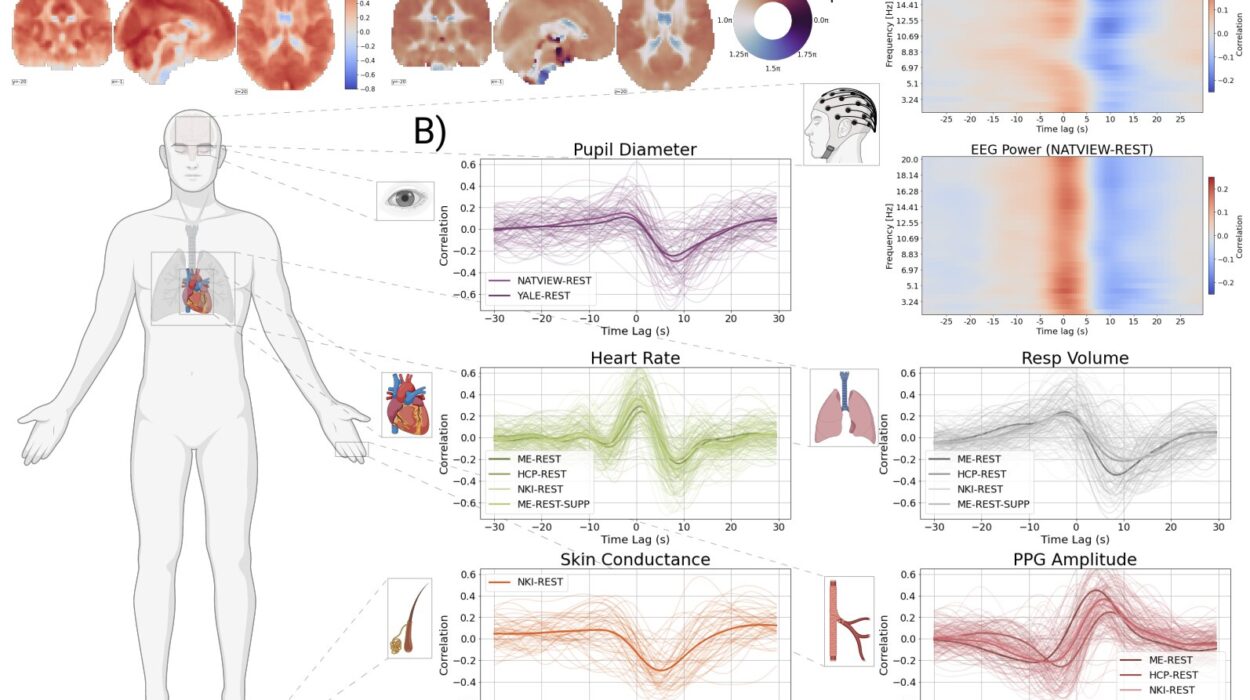
To predict the ripple effects of a national fluoride ban, Simon and her research team turned to the National Health and Nutrition Examination Survey (NHANES), a highly regarded dataset that collects health data from thousands of Americans. They specifically focused on oral health records for 8,484 children aged 0 to 19—a population for whom fluoride is most crucial.
With this information in hand, the researchers developed a microsimulation model—a kind of digital twin of the American pediatric population. This allowed them to simulate two future worlds: one in which current fluoride levels were maintained, and another in which fluoride was entirely removed from public water systems.
Over simulated 5- and 10-year time horizons, the model tracked changes in tooth decay, associated treatment costs, and quality-of-life impacts. It even accounted for indirect consequences, like complications from untreated decay—abscesses, missed school days, and pain-related behavioral issues.
The results were, in a word, alarming.
Tooth Decay by the Numbers
Under a fluoride-free scenario, the model predicted an additional 25.4 million decayed teeth over five years among U.S. children—a 7.5 percentage point increase. That translates to one additional cavity for every three children in the country.
Children from lower-income households bore the brunt of the burden. Those covered by Medicaid or without insurance accounted for most of the rise in dental disease. These are the same populations already facing barriers to regular dental visits, making preventive measures like fluoridation all the more essential.
Financially, the consequences were staggering. The study estimated an additional $9.8 billion in dental treatment costs over five years, rising to $19.4 billion after ten years. And these figures are likely conservative—they don’t include long-term complications or indirect economic impacts like missed school and work.
“Most of the increased cost could be attributed to publicly insured children, meaning it would be a direct public health cost,” says Simon. In other words, the price of inaction would land squarely on taxpayers.
Balancing Benefits and Risks
One of the most controversial aspects of fluoridation has always been safety. Detractors often point to fluorosis—a mild cosmetic condition that causes white streaks or spots on the teeth—as evidence of fluoride’s dangers. The new study did account for this. In the fluoride-free scenario, the number of fluorosis cases dropped by just 200,000—a small trade-off compared to the 25.4 million additional cavities predicted.
Importantly, the study did not attempt to model cognitive or neurodevelopmental effects of fluoride exposure. While such concerns have been raised in the past, Simon emphasizes that “current levels of fluoride in public water are not associated with worse neurobehavioral outcomes.” These levels fall well within the safety guidelines set by leading authorities, including the Environmental Protection Agency (EPA), the Centers for Disease Control and Prevention (CDC), and the National Toxicology Program.
Fluoride as a Social Equalizer
The findings highlight an often-overlooked truth about public health: preventive interventions like water fluoridation serve as powerful equalizers. They offer broad protection, but their benefits are felt most acutely by those who would otherwise slip through the cracks.
Dental care in the U.S. remains a tale of inequality. Privately insured families may have regular checkups, sealants, and early interventions, but millions of children lack that safety net. For these families, fluoride in drinking water may be the only consistent dental protection they receive.
That makes fluoride not just a mineral, but a matter of equity.
“Fluoride is one of the few interventions we can provide universally, across every tap,” says Sung Eun Choi, Ph.D., first author of the study and an assistant professor at Harvard School of Dental Medicine. “It doesn’t require an appointment, insurance, or even transportation—it just needs access to clean water.”
The Invisible Armor We Take for Granted
Perhaps the most remarkable thing about fluoridation is how unremarkable it seems. There’s no pill to take, no procedure to undergo, no daily effort required. It works silently and invisibly, strengthening enamel with every sip of water. Like vaccines and seat belts, its impact is most visible in its absence—when the protection is gone, risk comes rushing in.
Public trust in science and government policy is more fragile today than in decades past. Fluoride, like other public health measures, has not been immune to skepticism. Misleading claims have gained traction online, and in some communities, fluoridation has become a political flashpoint.
The new study aims to cut through the noise with rigorous, data-driven projections. “We know fluoride works,” says Simon. “Now we’re able to show just how much it works—and how much people stand to lose if we get rid of it.”
A Call to Prevention, Not Reaction
The study’s timing couldn’t be more critical. Dental decay remains the most common chronic disease in children, more prevalent than asthma or obesity. Despite medical advances, many children continue to suffer preventable pain, infections, and missed school days due to untreated cavities.
And while new dental technologies like silver diamine fluoride and tele-dentistry offer exciting frontiers, they cannot replace the foundational role of fluoride in community prevention.
The message is clear: fluoride in water isn’t just a scientific recommendation—it’s a public safeguard. Without it, the nation would face not only a surge in cavities but a widening gulf in dental health equity. The risks aren’t abstract; they’re written on the teeth of millions of children.
The Future of Fluoridation: Informed by Data, Grounded in Equity
As debates over public health policies continue to unfold, this new modeling study provides crucial evidence to guide decision-making. It doesn’t rely on speculation but on real-world data, translated into projected outcomes that policymakers, clinicians, and communities can understand.
Fluoridation is not a panacea for all dental ills, but it is a proven, low-cost, and high-impact tool in the arsenal against tooth decay. The choice to maintain or eliminate it carries far-reaching consequences—not only for individual smiles but for the health and finances of the nation as a whole.
In the words of Simon: “Fluoride isn’t magic, but it’s close. It’s simple, effective, and equitable. And we ignore its power at our peril.”
Reference: Sung Eun Choi et al, Projected Outcomes of Removing Fluoride From US Public Water Systems, JAMA Health Forum (2025). DOI: 10.1001/jamahealthforum.2025.1166