At the Institute of Neuroscience, Chinese Academy of Sciences, researchers have achieved something that sounds almost like science fiction: they grew human brain cells in the lab, transplanted them into mice, and found that these cells not only integrated into the brain’s wiring but also improved symptoms of anxiety and depression in the animals.
The cells in question were a special type of dopamine-producing neuron, known as A10 midbrain dopaminergic neurons. These neurons play a crucial role in the brain’s reward and emotion circuits. When they malfunction, people are more vulnerable to conditions such as depression, schizophrenia, and even drug addiction.
In their new study, published in Cell Stem Cell, scientists demonstrated that stem-cell-derived A10-like neurons could rebuild damaged mood circuits and suppress depression-like behavior in mice. This breakthrough not only offers a glimpse of new treatments for depression but also provides deeper insight into how our brains manage emotions and motivation.
Why Dopamine Neurons Matter
Dopamine is often called the brain’s “pleasure chemical,” but its role is much more complex. It doesn’t simply make us feel happy—it drives motivation, decision-making, movement, and even how we learn from rewards and punishments.
In particular, neurons from the ventral tegmental area (VTA)—a group of dopamine cells known as the A10 system—form connections with several regions: the nucleus accumbens, which processes reward; the amygdala, which governs fear and emotion; the olfactory tubercle, linked to sensory and reward integration; and the medial prefrontal cortex, which handles cognition and planning.
When the A10 system goes awry, people may struggle with loss of motivation, inability to feel pleasure, or distorted emotional regulation—all hallmarks of depression and related psychiatric conditions.
The Global Weight of Depression
Depression is not just a fleeting sadness; it is the most common neuropsychiatric disorder in the world. It affects hundreds of millions of people and is projected by the World Health Organization to become the third leading cause of global disease burden by 2030.
Current treatments, from antidepressant medications to psychotherapy, help many but not all patients. Even with the best available therapies, a large number of people continue to suffer with persistent symptoms. That’s why scientists are searching for new, biologically grounded strategies that target the root causes of mood disorders.
Growing Human Neurons in the Lab
Stem cells—immature cells capable of becoming any type of body cell—offer a unique opportunity. In recent years, scientists have used them to generate specific types of neurons, such as A9 dopamine neurons for experimental Parkinson’s disease therapy. However, producing A10 dopamine neurons, the ones most important for mood regulation, has remained a major challenge.
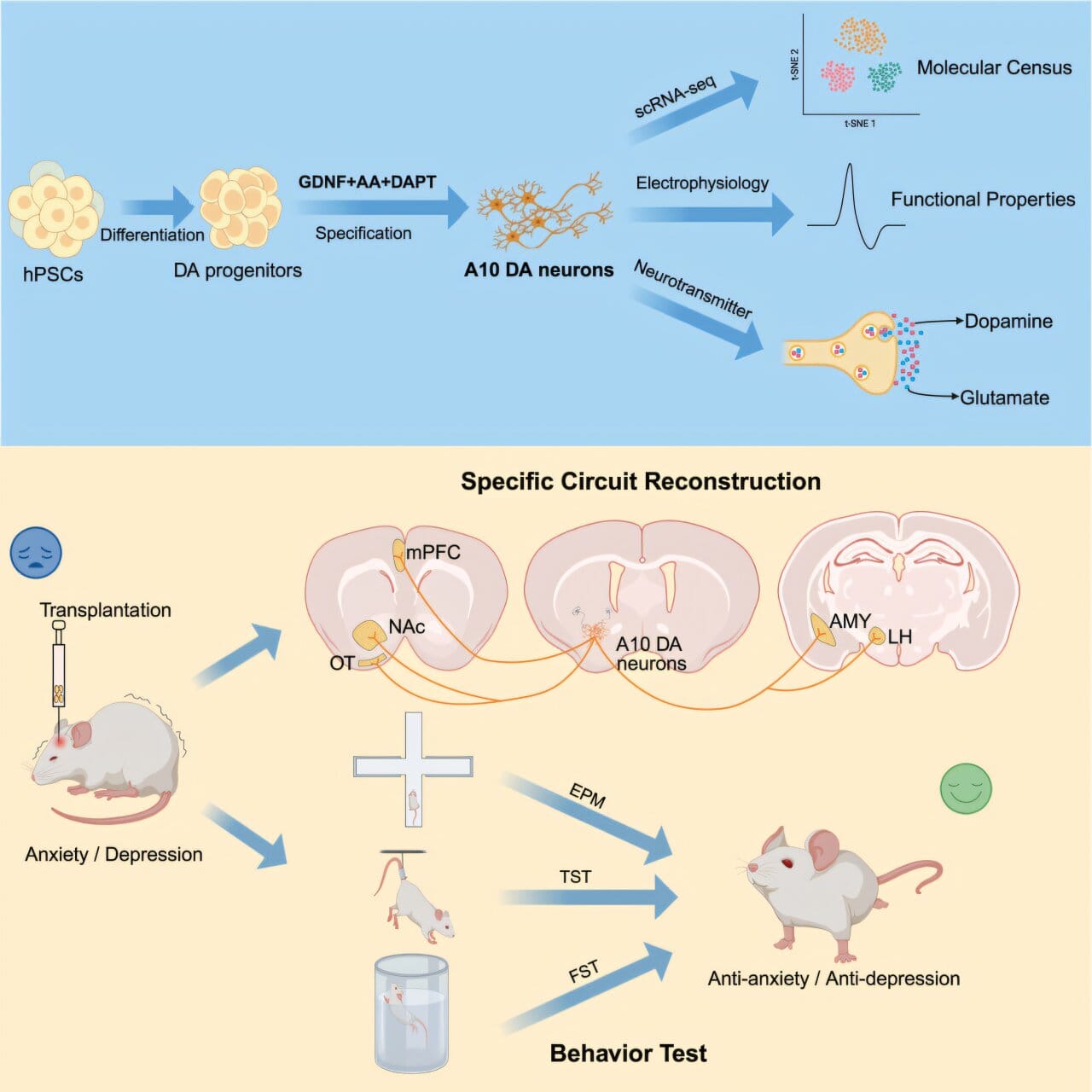
The new study overcame this barrier. Researchers developed a differentiation method—a kind of recipe—that guides human pluripotent stem cells into becoming A10-like neurons. When treated with a three-molecule mix, the stem cells produced the highest yield of A10 neurons, making up about 70% of dopamine-positive cells.
Advanced single-cell sequencing confirmed the identity of these neurons: around 62% were A10-like, with a smaller portion (16%) resembling A9 neurons. This level of precision marked a major leap in stem-cell engineering.
Transplanting Neurons into the Brain
Once the researchers had grown the A10-like neurons, they transplanted them into the brains of mice. The grafts were placed in regions central to mood and reward—the nucleus accumbens and the ventral tegmental area.
The transplanted neurons not only survived but began forming connections with the mouse brain. Axons from the human neurons extended into the amygdala, medial prefrontal cortex, and lateral hypothalamus—the very same targets that natural A10 neurons connect with in humans.
This integration was not superficial. The transplanted neurons showed the unique electrical properties of A10 neurons, including higher membrane resistance, longer rebound delays, and faster firing patterns than their A9 counterparts. In other words, they weren’t just present—they were functioning like authentic brain cells.
Turning Neurons On and Off
To test whether the grafted neurons could actually influence mood, scientists engineered some of them with tiny molecular “switches.” These switches allowed the neurons to be turned on or off with light or drugs—a technique known as optogenetics or chemogenetics.
When the neurons were activated, the mice showed clear improvements in behavior. They displayed fewer signs of anxiety and depression in standard laboratory tests, such as reduced immobility in stress-induced tasks. Brain chemistry analysis confirmed that dopamine release in the nucleus accumbens increased, directly linking the transplanted cells to mood improvement.
What This Means for Depression Research
The results are profound. For the first time, human stem-cell-derived A10-like neurons were shown to reconstruct the brain’s mesocorticolimbic circuit—the network that regulates reward, motivation, and emotion—and to produce measurable antidepressant and anxiolytic effects in living animals.
This suggests that in the future, similar strategies might be used in humans to repair damaged mood circuits. Unlike conventional antidepressants, which broadly alter brain chemistry, this approach could restore the specific pathways that underlie depression.
Challenges and Future Directions
While the findings are exciting, translating them into human therapy will take time. Safety is a critical concern: transplanted neurons must not cause tumors, immune rejection, or inappropriate overgrowth. Researchers must also refine the precision of differentiation to ensure that transplanted neurons are the right subtype and integrate in a controlled way.
Yet the study provides a compelling proof of principle. By using human stem cells to engineer the exact types of neurons disrupted in psychiatric illness, scientists may eventually move beyond treating symptoms toward repairing the very circuits that generate them.
A Glimpse of Hope
For millions of people living with depression, the disorder can feel like a weight pressing down on life itself. This research does not yet offer a cure, but it opens a new window of hope—a vision of medicine where damaged brain pathways can be rebuilt, and where mood and motivation can be restored not by masking symptoms but by addressing their biological roots.
As one of the authors concluded, the success of these experiments suggests a future where cell-based therapies for depression become a reality. Just as stem-cell-based treatments are already being tested for Parkinson’s disease, it may not be long before we see similar approaches for mental health.
In the end, this work is a reminder of the extraordinary resilience of the brain and the growing power of science to help it heal. The story of stem-cell-derived A10 neurons is not just about mice—it is about a future where human suffering from depression may be met with new, life-changing solutions.
More information: Wei Yan et al, Human stem cell-derived A10 dopaminergic neurons specifically integrate into mouse circuits and improve depression-like behaviors, Cell Stem Cell (2025). DOI: 10.1016/j.stem.2025.07.007