Imagine running freely through a field as a child, only to stop suddenly—not because you’re tired, but because your chest tightens, your breath shortens, and invisible hands seem to grip your lungs. For millions of people around the world, that isn’t imagination. It’s daily reality. Asthma is more than just a nuisance; it’s a chronic condition that can be frightening, life-disrupting, and sometimes life-threatening. But understanding it—really understanding it—is the first step toward regaining control.
Asthma is one of the most prevalent chronic diseases in the world, affecting over 300 million people globally. It does not discriminate by age, gender, or nationality. Its symptoms can come on like a whisper or a storm. Yet with science, compassion, and a clearer grasp of what asthma truly is, we can shift the narrative from fear to empowerment. To breathe freely again, we must begin by understanding what’s gone wrong deep inside the body.
The Body’s Betrayal: What Is Asthma?
At its core, asthma is an inflammatory disease of the airways—the tubes that carry air in and out of your lungs. These airways are lined with smooth muscles, mucus-producing glands, and sensitive tissues. In a healthy person, these tubes expand and contract effortlessly, allowing air to flow freely. But in a person with asthma, the story is very different.
When asthma flares, the lining of the airways becomes inflamed and swollen. Muscles surrounding the tubes tighten. Mucus is overproduced, clogging the passageways. This triple assault narrows the airway dramatically, making it harder to breathe in and, more importantly, harder to breathe out. The result is wheezing, coughing, shortness of breath, and that terrifying feeling of suffocating in your own body.
These episodes—called asthma attacks—can be mild, moderate, or severe. Some last minutes, others hours or even days. And while they can sometimes seem to appear out of nowhere, there is always a trigger, even if it’s not immediately visible.
A Perfect Storm: What Causes Asthma?
Asthma is not caused by a single factor. It is a multifactorial disease, the result of a complex interplay between genetics, environmental exposure, immune system behavior, and early-life experiences. Science has made great strides in unpacking the puzzle, but the story remains nuanced and deeply personal for each individual.
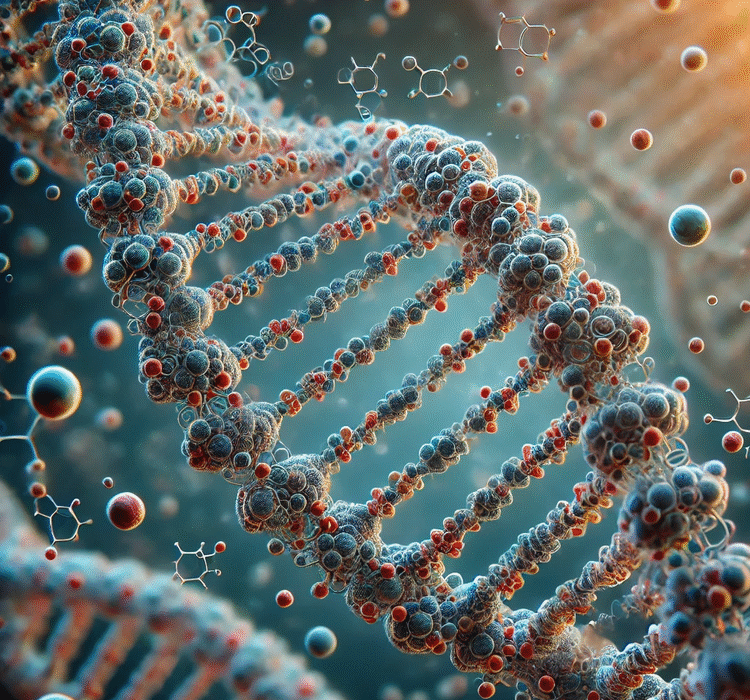
Genetics plays a powerful role. If one or both parents have asthma, the chances that their child will also develop it increase significantly. Certain genes influence how reactive the airway tissues are, how much IgE (an antibody linked to allergic responses) is produced, and how the immune system responds to common allergens. But genes alone do not cause asthma—they merely set the stage.
Environmental exposures—especially early in life—may determine whether that genetic script gets read or silenced. Exposure to allergens like dust mites, mold, cockroach droppings, pet dander, and pollen can sensitize the immune system. Repeated respiratory infections in childhood, particularly from respiratory syncytial virus (RSV), can inflame and scar the developing airways. Even the way we are born—vaginal delivery versus cesarean section—has been shown to influence our microbiome, and therefore our immune system and asthma risk.
The hygiene hypothesis suggests that children growing up in ultra-clean environments may be more likely to develop asthma because their immune systems are not adequately “trained” by exposure to microbes. Conversely, children raised on farms, surrounded by animals and soil microbes, often have lower asthma rates. It’s a startling paradox of modern life: the cleaner we are, the more allergic and asthmatic we may become.
The Triggers We Live With
Once asthma has developed, it rarely goes away. It becomes a part of you—sometimes silent, sometimes loud. The key to living with asthma lies in identifying and avoiding its triggers. These triggers vary widely among individuals, but they share one thing in common: they set off the inflammatory cascade that narrows the airways and steals the breath.
For many, allergens are the chief culprits. House dust mites, pollen from trees and grasses, pet dander, and molds can all provoke allergic asthma, which is the most common subtype. When these allergens enter the airways, the immune system responds with overzealous fervor, releasing histamine and other inflammatory chemicals that tighten and clog the airways.
Air pollution—both outdoor and indoor—is another major contributor. Fine particulate matter from car exhaust, factory emissions, cigarette smoke, and even cooking fumes can irritate the lungs. In urban environments, the combination of pollution and allergens often makes asthma symptoms worse.
Respiratory infections, especially viruses like the common cold or flu, are a common trigger for asthma attacks. Even a simple cold can lead to days of wheezing and tightness in the chest. Weather changes, cold air, exercise, and even strong emotions like anxiety or laughter can also set off symptoms.
For some people, their job is the problem. Occupational asthma, triggered by exposure to chemicals, dust, or fumes at work, is an underrecognized but significant issue. Bakers exposed to flour dust, healthcare workers exposed to latex, or construction workers breathing in chemicals may develop asthma over time.
The Invisible Inflammation
What makes asthma particularly insidious is that the inflammation in the lungs is often present even when there are no symptoms. This silent inflammation is what turns a manageable condition into a chronic battle. Over time, repeated inflammation can lead to airway remodeling—permanent structural changes in the lungs that make the airways thicker, scarred, and less flexible.
This means that controlling symptoms is not enough. The true goal of asthma management is controlling the underlying inflammation—preventing not just the cough or wheeze today, but the structural damage that could make breathing harder tomorrow.
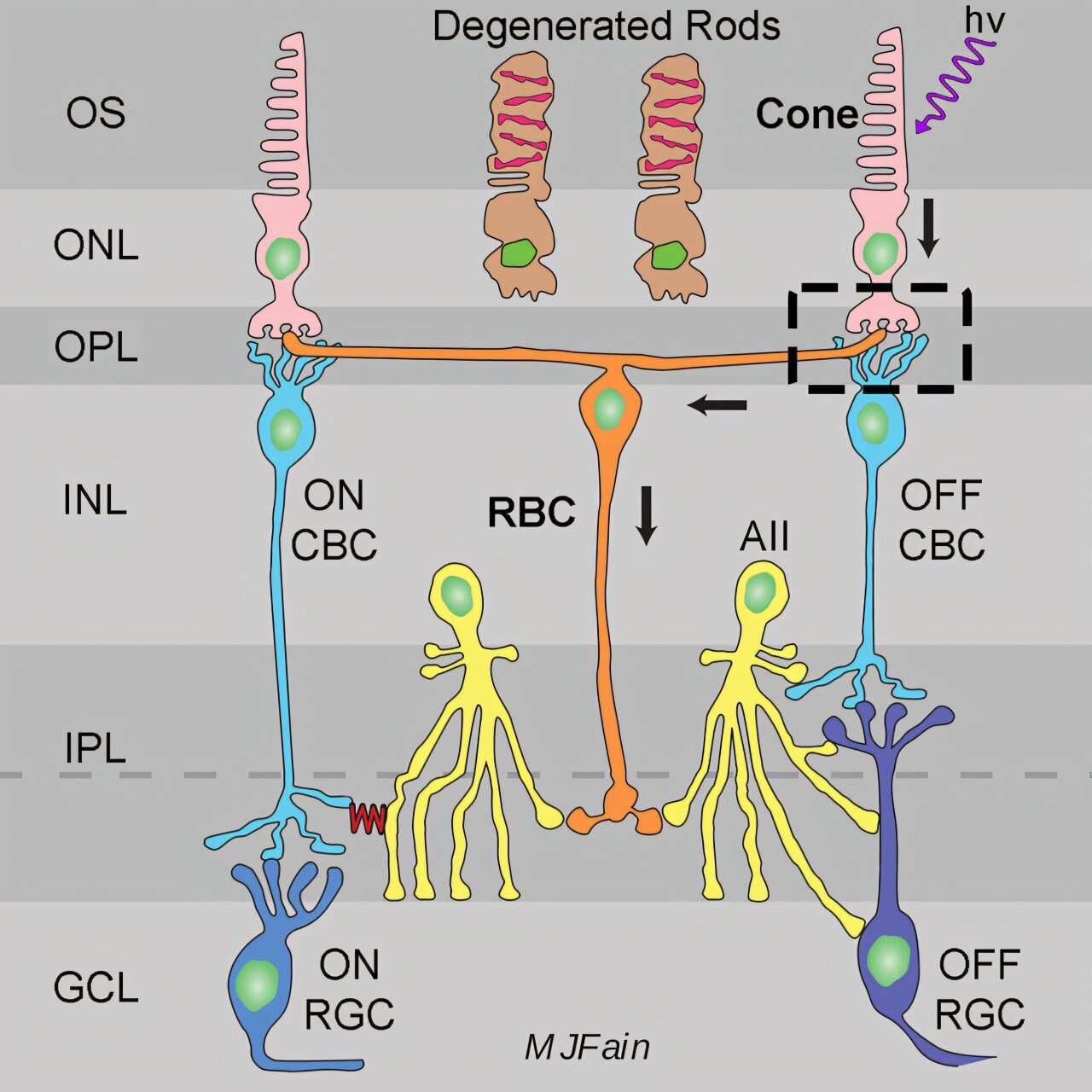
Medical science now recognizes that asthma is not a single disease but a syndrome—an umbrella term for several different patterns of inflammation. Some people have eosinophilic asthma, where white blood cells called eosinophils drive the inflammation. Others have neutrophilic or mixed-type asthma. Understanding the specific type of asthma a person has is essential to choosing the right treatment.
The Tools We Have
Thanks to decades of research, we now have an arsenal of tools to manage asthma effectively. The cornerstone of treatment is the inhaler—a compact, often life-saving device that delivers medication directly to the lungs. There are two main types: rescue inhalers and controller inhalers.
Rescue inhalers, like albuterol, provide quick relief by relaxing the muscles around the airways. They are used during an asthma attack or when symptoms suddenly worsen. But they are not a cure. Relying too heavily on them is a sign that asthma is not well controlled.
Controller inhalers, often containing inhaled corticosteroids, reduce inflammation over time. These must be used daily, even when symptoms are absent, to maintain stability and prevent future attacks. When used correctly, they can dramatically reduce hospital visits and improve quality of life.
In more severe cases, newer treatments are available. Biologic therapies—targeted drugs like omalizumab, mepolizumab, and dupilumab—block specific molecules involved in the inflammatory process. These are revolutionizing asthma care for those whose disease was previously resistant to standard therapies.
Allergy immunotherapy, such as allergy shots or tablets, can help desensitize the immune system over time. And for some, treating comorbidities like acid reflux, obesity, or sleep apnea can also improve asthma control.
The Mind-Body Connection
Asthma does not only affect the lungs—it affects the mind. Living with a chronic disease that can flare unpredictably often leads to anxiety and depression. Panic can worsen asthma symptoms, and breathlessness can induce panic. This vicious cycle is more common than most doctors acknowledge.
Mindfulness-based stress reduction, breathing techniques, and psychological counseling have been shown to help. Learning to listen to the body without judgment, to recognize early warning signs of a flare, and to remain calm during symptoms can make a meaningful difference.
The breath is not just a biological function—it is an emotional one. We sigh when we’re sad, gasp when we’re shocked, breathe quickly when we’re anxious. Asthma hijacks that sacred link between emotion and breath. Reclaiming it is a vital part of healing.
Childhood Asthma: A Fragile Beginning
For children, asthma can be particularly cruel. It interrupts play, learning, and sleep. It sends parents into midnight panic and results in missed school days and ER visits. Childhood asthma often begins early in life, and while some children “outgrow” their symptoms, others carry the disease into adulthood.
The causes of childhood asthma mirror those of adults: genetics, allergens, infections, and environmental toxins. But there is growing concern that our modern environment—polluted air, lack of outdoor play, excessive screen time, and poor diets—may be increasing the risk.
Fortunately, with early diagnosis and treatment, children with asthma can lead full, active lives. Education is key. Teaching parents, teachers, and the children themselves how to use inhalers, recognize triggers, and manage symptoms can prevent unnecessary suffering.
Living with Asthma, Not Under It
Asthma cannot yet be cured, but it can be controlled. Millions of people around the world live vibrant, active lives with asthma—running marathons, climbing mountains, singing on stage. What sets them apart is not the absence of disease but the presence of knowledge, preparation, and support.
Personalized asthma action plans—created with a healthcare provider—help individuals know exactly what to do when symptoms worsen. These plans outline daily medication use, early warning signs, and when to seek emergency help.
Technology has also entered the picture. Smart inhalers that track usage, apps that monitor air quality, and digital peak flow meters are empowering people with asthma to manage their condition more effectively than ever before.
Support networks, whether in-person or online, offer emotional strength and practical advice. No one with asthma needs to feel alone. With community, understanding, and science, asthma becomes not a prison but a challenge that can be overcome.
A Hopeful Horizon
Research into asthma is advancing rapidly. Scientists are studying the microbiome of the lungs, the role of epigenetics in gene expression, and new ways to modulate the immune response. Vaccines for RSV and improved biologic therapies promise better prevention and control. Precision medicine—tailoring treatment to the individual’s specific disease subtype—is becoming a reality.
But perhaps the most profound change is in how we view asthma. Not as a weakness or a stigma, but as a condition that can be understood, managed, and lived with. A reminder of the fragile beauty of breath—and the incredible strength it takes to fight for it.
Asthma may constrict the airways, but it does not have to constrict the spirit. Every breath taken in defiance of the disease is an act of courage. Every child who learns to use their inhaler is an act of empowerment. Every parent who loses sleep monitoring their child’s breathing is an act of love.
Breathing Forward
Asthma teaches us never to take a breath for granted. It reminds us how deeply connected we are to the world around us—its allergens, its toxins, its climate, and its rhythms. It calls for compassion: for the child gasping on the playground, for the elderly woman wheezing in the night, for the worker choking on fumes.
It also teaches resilience. People with asthma learn to listen to their bodies, to adapt, to persevere. They learn to balance caution with courage. And in that balance, there is strength.
To control asthma is not simply to use medication—it is to reclaim breath as a birthright. It is to live fully, despite the invisible war in the lungs. It is to breathe forward into life, knowing that every exhale is a victory.