Beneath the surface of our bodies lies a complex scaffold of bones and joints, silently supporting us through every motion and milestone. Strong and resilient as they are, bones and joints are not impervious to harm. Among the less known but potentially devastating threats to our musculoskeletal system are bone and joint infections. These infections, though relatively rare compared to other types, can lead to long-term disability, chronic pain, and even life-threatening complications if not treated swiftly and effectively.
What makes these infections particularly dangerous is their ability to hide in plain sight. Symptoms can be subtle at first, and the immune system often struggles to reach the dense, closed-off environment of bones and joints. Once bacteria, fungi, or other pathogens gain access, they can set up camp in these protected havens, evading treatment and quietly doing damage.
To truly grasp the nature of bone and joint infections, we must journey through the anatomy of bones, the defenses of our immune system, and the clever strategies pathogens use to outsmart them. Understanding this invisible battlefield reveals not only the dangers of infection but also the triumphs of modern medicine in fighting back.
The inner workings of bone and joint structure
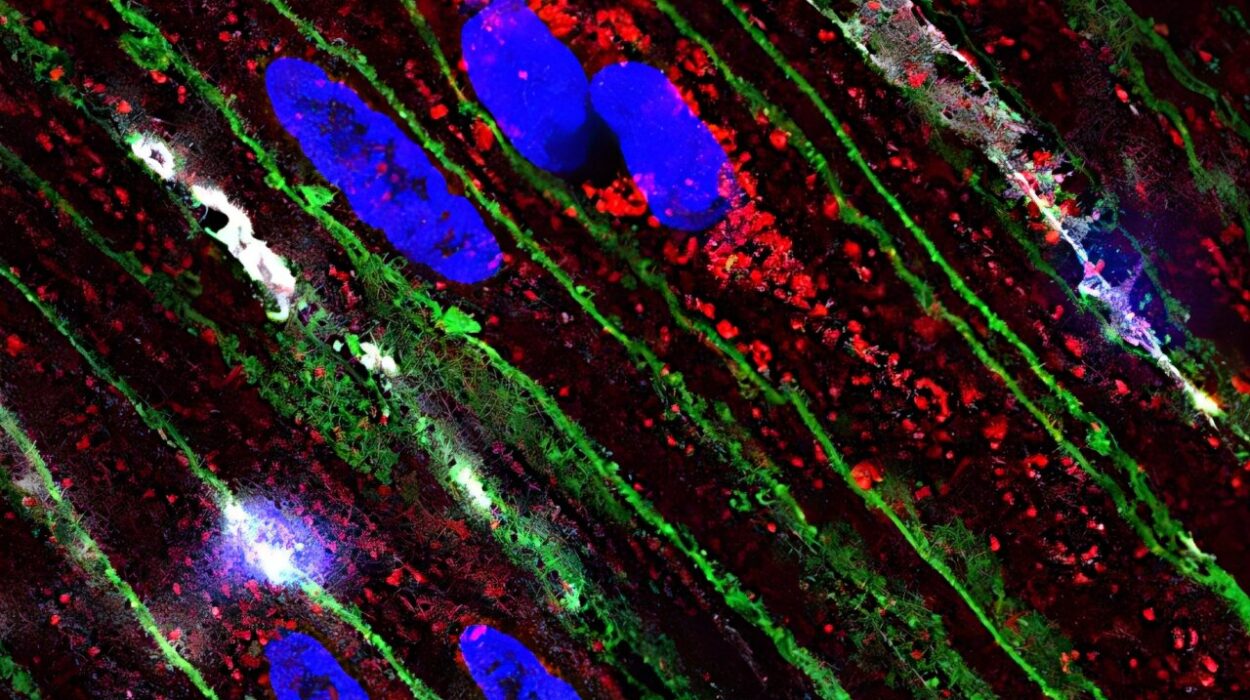
Bones are more than just static rods of calcium. They are living tissues composed of cells, blood vessels, nerves, and a rich network of marrow and connective proteins. Osteoblasts build bone, osteoclasts break it down, and osteocytes maintain its health. The inner cavity of long bones houses bone marrow, where immune cells are born and blood cells are manufactured.
Joints, the junctions where bones meet, are equally complex. Some are fixed like the sutures of the skull, while others like the knee or shoulder are marvels of mechanical engineering. Synovial joints, in particular, are lined with a thin membrane that produces synovial fluid—an oily substance that reduces friction and nourishes cartilage. This fluid also provides an easy entry point for pathogens if they manage to breach the body’s outer defenses.
While the bloodstream normally delivers nutrients and immune cells to tissues efficiently, bones and joints are less accessible. Their relatively poor blood supply can make it harder for the immune system to detect and eliminate invaders once an infection sets in.
How pathogens invade the skeletal system
There are three main ways pathogens can reach bones and joints. The first and most common route is through the bloodstream, especially during a systemic infection like bacteremia or sepsis. A simple skin infection, untreated urinary tract infection, or even dental procedure can release bacteria into the blood, which may then lodge in a bone, particularly in areas with rich vascular growth like the ends of long bones in children.
The second route is direct inoculation through trauma, surgery, or orthopedic implants. A broken bone that pierces the skin creates an open gateway for bacteria, as does a surgical procedure like a joint replacement. While modern sterile techniques have vastly reduced the risk, surgical infections still occur, particularly in cases of poor wound healing or immunocompromised patients.
The third route involves contiguous spread from a nearby infected tissue. An untreated skin abscess, infected diabetic foot ulcer, or cellulitis can spread directly into underlying bone, a scenario often seen in cases of chronic osteomyelitis in people with peripheral vascular disease or diabetes.
Once inside, pathogens face a surprisingly welcoming environment. Bone marrow is rich in nutrients and iron, and synovial fluid provides a relatively immune-privileged space. Certain bacteria, especially Staphylococcus aureus, are equipped with proteins that help them cling to bone matrix and evade destruction by white blood cells.
The most common culprits behind the scenes
Bone and joint infections are most often caused by bacteria, with Staphylococcus aureus being the prime offender. This microbe is notorious for its virulence and its arsenal of tricks. It can form biofilms—slimy matrices that shield it from antibiotics and immune cells—and can hide inside osteoblasts, making it nearly impossible to eliminate.
Other bacteria implicated in these infections include Streptococcus pyogenes, Pseudomonas aeruginosa, and Escherichia coli. In neonates, Group B Streptococcus and Haemophilus influenzae can invade rapidly, while older adults might be more prone to infections by gram-negative bacilli or polymicrobial sources, especially in cases of pressure ulcers or diabetic foot infections.
In immunocompromised individuals, such as those undergoing chemotherapy or living with HIV/AIDS, fungal infections like Candida or Aspergillus can also target bones and joints. Tuberculosis, though declining in many parts of the world, remains a significant cause of spinal osteomyelitis (Pott’s disease) in certain regions.
When infection meets the bone
Osteomyelitis is the medical term for infection of the bone. It can present acutely, subacutely, or chronically, depending on how fast it develops and how long it has been present. In children, acute osteomyelitis often affects the metaphysis—the growing end of long bones like the femur or tibia. They may present with fever, localized pain, limping, or refusal to move the affected limb. Blood tests often show elevated markers of inflammation, and imaging such as MRI can reveal swelling and early bone changes.
In adults, chronic osteomyelitis may develop after trauma, surgery, or in association with poor blood supply. Symptoms may be more subtle—persistent pain, swelling, low-grade fever, or draining wounds. These infections can smolder for years, flaring up intermittently and forming sinus tracts that leak pus.
Another common site of bone infection is the spine. Vertebral osteomyelitis can cause back pain, stiffness, and eventually neurological deficits if the infection spreads to the spinal cord. Diagnosis is often delayed because symptoms mimic other conditions like degenerative disc disease or mechanical back strain.
When joints are under attack
Septic arthritis is an infection within a joint, usually caused by bacteria but sometimes fungi or viruses. It is a medical emergency, capable of destroying cartilage and causing irreversible joint damage in a matter of days.
In children, the hip and knee are commonly affected. They may refuse to bear weight, cry during diaper changes, or have a swollen, warm joint. In adults, large joints like the knee, shoulder, or elbow are frequent targets. Risk factors include recent joint surgery, rheumatoid arthritis, prosthetic joints, or intravenous drug use.
One unique and important form of joint infection is prosthetic joint infection (PJI). Despite careful surgical practices, artificial hips and knees can sometimes become infected. This presents a unique challenge, as the bacteria form biofilms on the implant’s surface, rendering antibiotics far less effective. Treatment often requires not just antibiotics but surgical intervention to remove and replace the prosthetic hardware.
How infections are detected and diagnosed
Because the symptoms of bone and joint infections can mimic other conditions—arthritis, injuries, or even tumors—accurate diagnosis requires a combination of clinical suspicion, imaging, and laboratory testing.
Physicians begin with a careful history and physical examination, looking for signs like fever, localized tenderness, swelling, redness, or reduced joint mobility. Blood tests such as white blood cell count, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) help detect systemic inflammation.
Imaging studies play a crucial role. X-rays may show bone destruction or joint space narrowing, but changes can lag behind symptoms. MRI is more sensitive and can detect early bone marrow edema, abscesses, and soft tissue involvement. In some cases, nuclear medicine bone scans or PET-CT may be used for detecting deep or multifocal infections.
Definitive diagnosis, however, often requires direct sampling. Aspiration of joint fluid or bone biopsy allows microbiologists to culture the pathogen and determine its antibiotic susceptibility. Identifying the causative organism is essential for tailoring effective treatment.
The road to treatment and recovery
Treating bone and joint infections is no simple task. Unlike superficial infections, these pathogens burrow into dense tissue and protected spaces. The blood supply to bones and joints is limited, and biofilms complicate antibiotic delivery.
In most cases, treatment begins with intravenous antibiotics—sometimes for four to six weeks or more. These may be followed by oral antibiotics to complete a longer course, particularly for chronic osteomyelitis. The choice of drug depends on the specific organism and its resistance profile. In some cases, such as methicillin-resistant Staphylococcus aureus (MRSA), powerful antibiotics like vancomycin or linezolid may be required.
Surgical intervention is often needed. This may include debridement (removal of infected tissue), drainage of abscesses, or hardware removal in prosthetic infections. In some cases of chronic osteomyelitis or failed treatments, more drastic measures like bone resection or amputation may be necessary to control the spread.
Recovery can be slow and requires not only physical rehabilitation but emotional resilience. Patients may need long-term antibiotics through a central line, regular imaging, and ongoing monitoring for recurrence. But with prompt diagnosis and comprehensive care, many recover fully and regain function.
How chronic diseases complicate infections
Not all individuals are equally vulnerable to bone and joint infections. Those with chronic illnesses like diabetes, peripheral vascular disease, or immune suppression are at heightened risk. In diabetic patients, for instance, poor blood flow and nerve damage can mask the early signs of infection. A minor foot injury can evolve into chronic osteomyelitis without pain or visible symptoms until it becomes advanced.
Rheumatoid arthritis and lupus, both autoimmune diseases, increase the risk of septic arthritis—both due to the disease itself and the immunosuppressive medications used to treat them. Cancer patients, transplant recipients, and those on long-term steroids or chemotherapy also face increased vulnerability.
These populations require closer monitoring, and even minor symptoms like joint swelling or unexplained fever should prompt evaluation for infection.
The global burden and its disproportionate impact
While bone and joint infections are a global health issue, they do not affect all populations equally. In high-income countries, most infections result from surgical complications or trauma. In low- and middle-income countries, untreated wounds, poor access to healthcare, and diseases like tuberculosis contribute significantly to the burden.
Spinal tuberculosis continues to be a leading cause of vertebral osteomyelitis in developing nations, often presenting late with deformity and neurological impairment. In rural areas, limited imaging availability and diagnostic tools delay detection, allowing infections to become advanced before care is initiated.
Efforts to reduce the global burden must address not only medical treatments but also systemic inequities—improving access to clean water, sanitation, surgical safety, and antibiotic stewardship.
Future directions and evolving therapies
Advances in microbiology, imaging, and biomaterials are reshaping the approach to bone and joint infections. Researchers are exploring new antibiotics, biofilm-disrupting agents, and targeted drug delivery systems that penetrate bone more effectively.
Phage therapy—the use of viruses that infect and destroy bacteria—is gaining attention for drug-resistant infections. In some cases, individualized phage cocktails have successfully treated otherwise untreatable osteomyelitis.
On the surgical front, techniques for one-stage prosthetic replacement during infection (rather than two-stage removal and reimplantation) are improving outcomes. Antimicrobial coatings on implants, antibiotic-loaded bone cement, and 3D-printed scaffolds are offering new possibilities in infection prevention and reconstruction.
Artificial intelligence and machine learning are also beginning to aid diagnosis by analyzing subtle imaging features or predicting infection risk after surgery.
A quiet battle with lasting consequences
Though less visible than heart disease or cancer, bone and joint infections are no less consequential. They strike at the core of mobility, independence, and quality of life. For those affected, the journey often involves pain, uncertainty, and a protracted recovery.
Yet understanding the biological dance between pathogen and host offers hope. It reminds us of the marvel of our immune defenses, the ingenuity of modern science, and the importance of vigilance. From a child’s limping gait to an elderly patient’s inflamed knee, these infections whisper their presence in subtle signs. And with the right tools, we can learn to listen—and to heal.