Male fertility is one of the most overlooked aspects of human health, yet it is a cornerstone of reproduction, family, and even the survival of our species. Conversations about fertility often center on women, but nearly half of all infertility cases involve male factors. Despite this, many men rarely think about their reproductive health until faced with challenges in conceiving.
Male fertility is not only about sperm count; it reflects a man’s overall health, lifestyle, environment, and even psychological well-being. It is shaped by biology but also by choices, habits, and circumstances. Understanding it is more than just a matter of science—it is a matter of humanity, identity, and legacy.
To grasp the science of male fertility, we must explore the intricate journey of sperm production, the influence of hormones, the fragility of reproductive biology, and the ways lifestyle and environment either nurture or sabotage this delicate process. From there, we can understand how to protect and improve fertility, ensuring that men have the tools and knowledge to safeguard this vital aspect of life.
The Biological Basis of Male Fertility
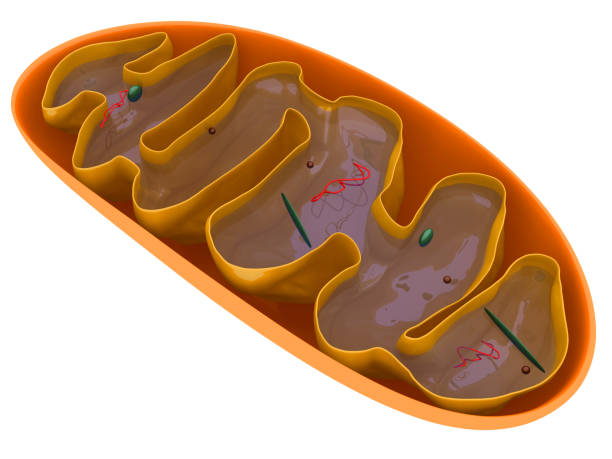
At the core of male fertility is spermatogenesis—the biological process by which sperm are produced in the testes. This remarkable cycle takes about 64 to 74 days, during which immature germ cells develop into mature, motile sperm capable of fertilizing an egg.
The testes house tiny coiled structures called seminiferous tubules, where sperm production begins. Specialized cells called Sertoli cells provide nourishment and structural support, while Leydig cells, located outside the tubules, produce testosterone, the hormone essential for sperm development and male sexual function.
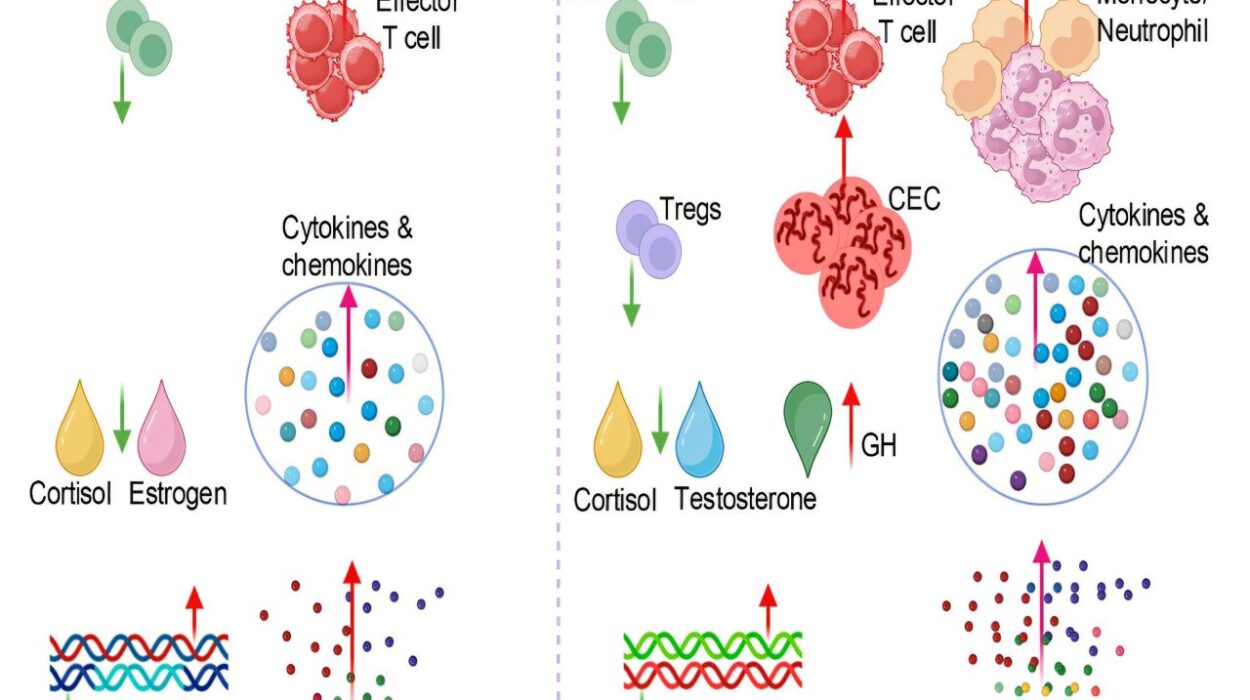
Spermatogenesis is a finely tuned dance of hormones and cellular processes. The hypothalamus in the brain releases gonadotropin-releasing hormone (GnRH), which signals the pituitary gland to produce luteinizing hormone (LH) and follicle-stimulating hormone (FSH). LH stimulates testosterone production, while FSH works with testosterone to drive sperm production. If any part of this chain falters, fertility can suffer.
Every day, a healthy man produces millions of sperm, but quantity alone does not guarantee fertility. Sperm must also be healthy in structure (morphology) and movement (motility). Defects in shape or sluggish movement can prevent sperm from reaching or penetrating the egg.
Sperm Quality: More Than Just Numbers
Semen analysis is the most common test for male fertility, and it measures several key factors:
- Sperm count: the number of sperm in each milliliter of semen.
- Motility: the percentage of sperm that move efficiently.
- Morphology: the shape and structure of sperm, which influence their ability to penetrate the egg.
- Volume and consistency of semen, which help transport sperm during ejaculation.
A man with a low sperm count may still be fertile if his sperm are highly motile and structurally normal. Conversely, even men with normal counts may struggle with fertility if most of their sperm are poorly shaped or immobile.
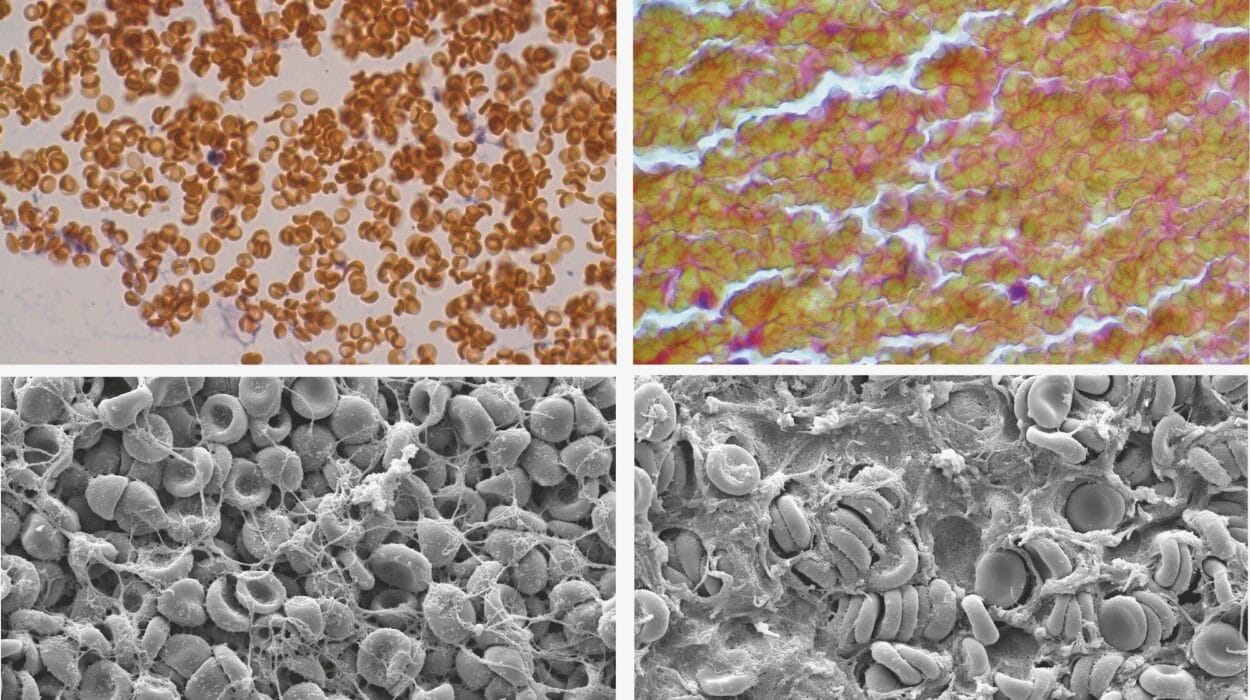
Sperm are fragile, vulnerable to heat, toxins, oxidative stress, and DNA damage. Unlike eggs, which women are born with, sperm are continuously produced, making them more susceptible to environmental and lifestyle influences.
Male Fertility and Age
Age is often discussed in the context of female fertility, but it matters for men, too. While men can remain fertile much longer than women, sperm quality tends to decline with age. Research shows that older men are more likely to have lower motility, higher DNA fragmentation, and increased risks of passing genetic mutations to offspring.
Children of older fathers may face higher risks of certain conditions, including autism spectrum disorders and schizophrenia, though these associations are complex and not solely determined by paternal age. Nevertheless, it highlights that male fertility, like all biology, is influenced by time.
Lifestyle Factors That Shape Fertility
One of the most remarkable truths about male fertility is how profoundly it is shaped by lifestyle. Everyday choices about diet, exercise, sleep, and stress have measurable effects on sperm quality.
Nutrition and Fertility
Sperm are tiny, but they are metabolically active cells that need proper fuel. A diet rich in antioxidants, vitamins, minerals, and healthy fats supports sperm production and protects against oxidative stress—a major cause of DNA damage in sperm.
Key nutrients include zinc, selenium, vitamin C, vitamin E, folate, and omega-3 fatty acids. These nutrients support sperm count, motility, and morphology by reducing oxidative stress, stabilizing cell membranes, and aiding DNA synthesis.
Conversely, diets high in processed foods, trans fats, and excessive alcohol contribute to inflammation and poor sperm health. Obesity is particularly harmful; it alters hormone balance, increases scrotal temperature, and promotes oxidative damage.
Exercise and Fertility
Regular physical activity improves circulation, regulates hormones, and supports healthy weight—all beneficial for fertility. However, extreme exercise, especially endurance training or anabolic steroid use, can suppress testosterone and harm sperm production.
The balance is key: moderate, consistent exercise fosters fertility, while extremes can disrupt it.
Sleep and Fertility
Sleep is often neglected, but it plays a crucial role in hormonal regulation. Men who sleep poorly or less than six hours per night often show reduced testosterone levels and poorer sperm quality. Sleep deprivation also contributes to stress, obesity, and metabolic issues, all of which impair fertility.
Stress and Fertility
Psychological stress triggers the release of cortisol, which interferes with the hypothalamic-pituitary-gonadal axis, the hormonal system that regulates fertility. Stress can lower testosterone, reduce libido, and negatively affect sperm production.
Moreover, stress often leads to unhealthy coping habits such as smoking, drinking, or overeating, compounding its effects on fertility.
Environmental Threats to Male Fertility
The modern world presents unique threats to reproductive health. Sperm are particularly sensitive to environmental toxins, pollutants, and even heat.
- Chemicals: Pesticides, heavy metals, industrial solvents, and endocrine-disrupting chemicals (like BPA and phthalates found in plastics) can reduce sperm count and motility.
- Radiation and heat: Frequent use of hot tubs, laptops placed on laps, or tight clothing can raise scrotal temperature and impair spermatogenesis.
- Pollution: Air pollution has been linked to increased oxidative stress and sperm DNA damage.
Men living in polluted urban environments or working in industries with chemical exposure face greater risks, highlighting the need for protective measures and broader public health interventions.
Medical Conditions That Impact Fertility
Several medical conditions directly affect male fertility:
- Varicocele: Enlarged veins in the scrotum that raise testicular temperature and impair sperm production.
- Infections: Sexually transmitted infections (like chlamydia or gonorrhea) or mumps orchitis can damage reproductive tissues.
- Hormonal imbalances: Low testosterone or disrupted signaling between the brain and testes can halt sperm production.
- Genetic conditions: Disorders like Klinefelter syndrome can reduce fertility or cause azoospermia (absence of sperm).
- Chronic illnesses: Diabetes, obesity, and autoimmune diseases can all negatively affect fertility through hormonal and vascular disruptions.
Modern medicine offers treatments—from surgery for varicocele to hormone therapy or assisted reproductive technologies (ART) like IVF and ICSI (intracytoplasmic sperm injection)—but prevention and lifestyle optimization remain crucial.
Improving Male Fertility: What Science Says
Enhancing male fertility is rarely about one “magic bullet.” Instead, it is about creating conditions that support the body’s natural ability to produce healthy sperm. Science points to several practical strategies:
- Balanced diet: Prioritize whole foods, antioxidants, lean proteins, and healthy fats.
- Regular moderate exercise: Support circulation and hormone balance without overtraining.
- Adequate sleep: Aim for 7–9 hours of restorative sleep nightly.
- Stress management: Mindfulness, meditation, yoga, or even simple deep-breathing exercises can help.
- Limiting toxins: Reduce alcohol, quit smoking, and avoid exposure to pesticides and plastics when possible.
- Protecting the testes from heat: Wear looser clothing, avoid prolonged sitting with laptops on the lap, and limit hot tub use.
- Medical support: Seek evaluation for conditions like varicocele, infections, or hormonal imbalances if conception is difficult.
These practices not only improve fertility but also enhance overall health, reinforcing the idea that reproductive wellness mirrors broader well-being.
Male Fertility and Identity
Fertility is not merely a biological function—it is intertwined with identity, masculinity, and self-worth. Struggles with fertility can deeply affect mental health, leading to feelings of inadequacy, shame, or depression.
It is vital to recognize that male infertility does not equate to diminished masculinity. Fertility is a medical condition, not a measure of strength, virility, or character. Breaking the silence around male infertility is crucial for supporting emotional well-being and encouraging men to seek medical help without stigma.
The Role of Assisted Reproductive Technology
For couples facing infertility, assisted reproductive technologies have revolutionized possibilities. Techniques such as in vitro fertilization (IVF), intracytoplasmic sperm injection (ICSI), and sperm retrieval from testicular tissue can overcome severe male fertility challenges.
These advances, however, raise ethical, financial, and emotional questions. They underscore both the fragility and the resilience of human reproduction—the ability to intervene when nature falters, while also reminding us of the profound responsibility that comes with creating life.
The Future of Male Fertility Science
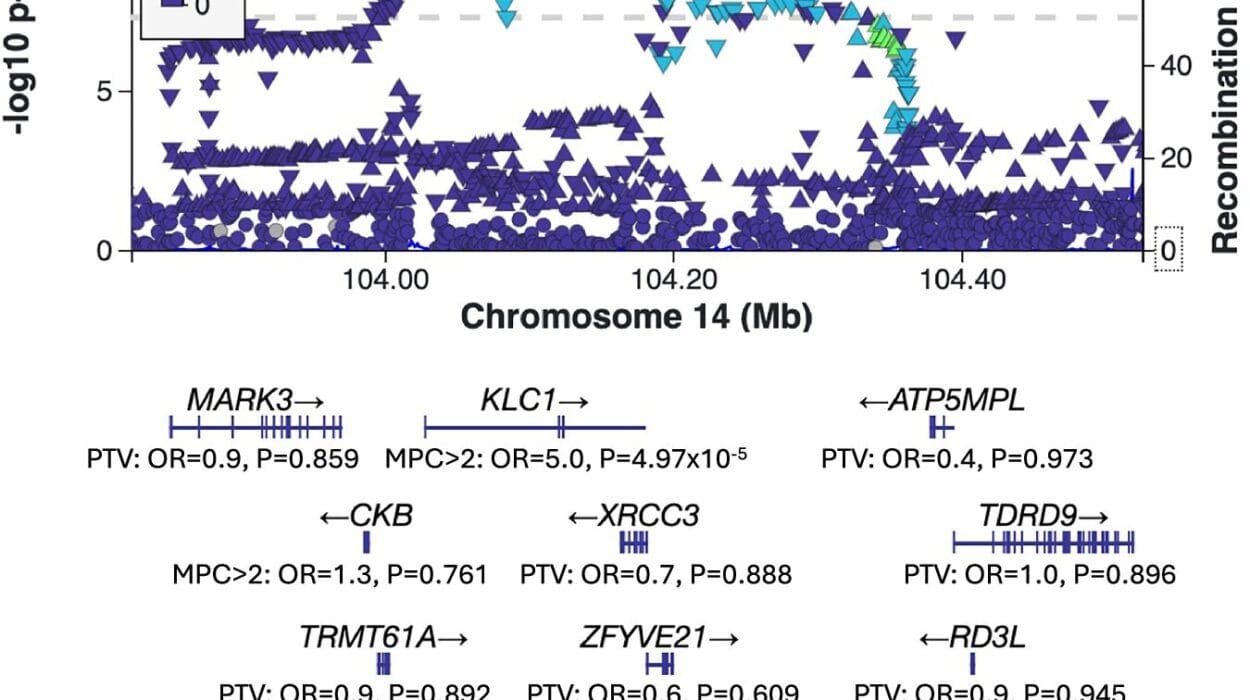
Research on male fertility is accelerating. Scientists are exploring stem-cell therapies to restore sperm production, genetic editing to correct inherited infertility, and advanced diagnostics to detect subtle sperm abnormalities.
There is growing interest in the role of the microbiome—the community of microbes in the body—in shaping fertility, as well as in epigenetics, which studies how lifestyle and environment influence gene expression across generations.
The future may bring personalized fertility medicine, where men receive tailored interventions based on their genetic profile, environment, and lifestyle. But even as the science evolves, the basics remain: healthy living, protection from toxins, and early medical attention when problems arise.
Fertility as a Reflection of Whole-Body Health
Ultimately, male fertility is more than the ability to conceive a child. It is a reflection of whole-body health, influenced by nutrition, exercise, mental well-being, and environment. A man with healthy fertility is often one whose body and mind are in balance.
In this sense, fertility becomes a mirror—showing us not just whether sperm can meet egg, but whether we are caring for our bodies, minds, and environments in ways that support life.
Closing Reflections: Protecting the Seeds of Life
The science of male fertility reveals a delicate, wondrous process—millions of sperm produced each day, each carrying the potential to spark new life. But it also reveals vulnerability. Fertility can be damaged by toxins, stress, illness, and neglect.
Improving fertility, then, is not only about fatherhood—it is about honoring the body, cultivating health, and preparing to pass life forward with strength and integrity. In the end, the science of male fertility is not only about biology; it is about continuity, responsibility, and the timeless human desire to nurture the future.