In a remarkable twist that’s reshaping how we think about some of today’s most popular diabetes drugs, medications like Ozempic and Wegovy—known scientifically as GLP-1 receptor agonists—are now stepping into an unexpected spotlight: brain health.
These drugs, originally engineered to treat type 2 diabetes and support weight loss, are now being explored for a more profound role—potentially slowing the progression of, or even preventing, dementia. This isn’t just medical speculation. Two new studies, paired with a compelling editorial in JAMA Neurology, are painting an increasingly hopeful picture of how these metabolic medications might double as cognitive protectors.
As Alzheimer’s disease and related dementias tighten their grip on aging populations worldwide—affecting nearly 7 million Americans today and projected to reach nearly 14 million by 2060—this new wave of research couldn’t come at a more critical time.
A New Chapter for Familiar Medications
GLP-1 receptor agonists like semaglutide (marketed as Ozempic for diabetes and Wegovy for obesity) were originally developed to stimulate insulin production, lower blood glucose levels, and help manage weight. But in recent years, scientists began noticing something curious: patients on these drugs seemed to be doing better in ways that went beyond blood sugar and body weight.
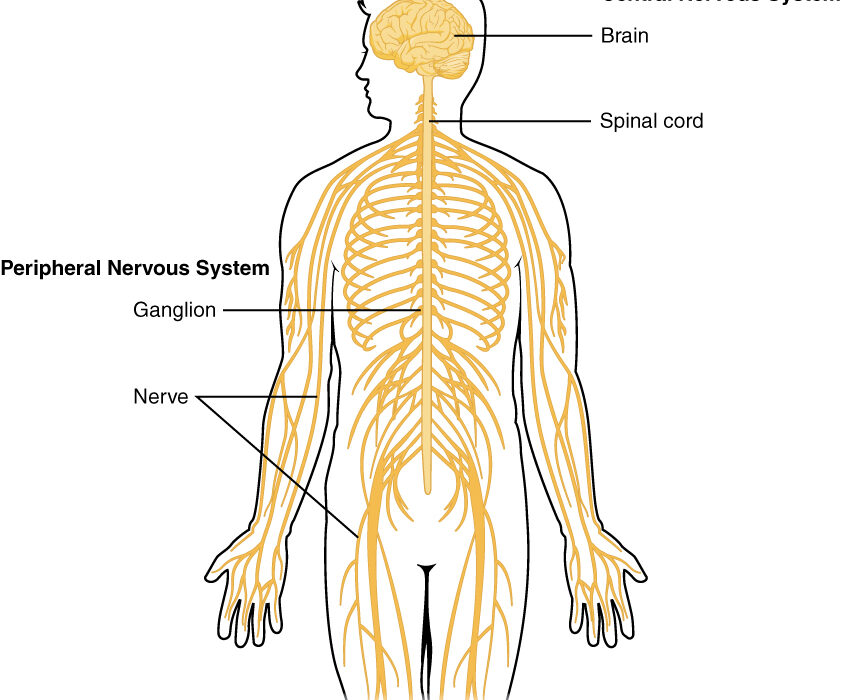
What started as clinical anecdotes soon gave way to structured investigation. Researchers discovered that GLP-1 receptors aren’t just hanging out in the pancreas and gut—they’re also located in the brain, particularly in areas tied to memory, cognition, and neuroinflammation. That raised an intriguing question: could these drugs actually be influencing brain function?
The Florida Study: A Big Data Revelation
To investigate further, scientists from the University of Florida embarked on a large-scale study that dove into the health records of over 90,000 patients with type 2 diabetes. What they found was striking.
Patients who were treated with GLP-1 receptor agonists had a 33% lower risk of developing Alzheimer’s disease and related dementias (ADRD) compared to those on other glucose-lowering medications. Another class of diabetes drugs—SGLT2 inhibitors—also showed promise, with a 43% reduction in ADRD risk. Although SGLT2 inhibitors appeared slightly more effective on paper, statistically, the differences between the two groups weren’t significant, meaning both drug classes may offer a similar level of cognitive protection.
This study was observational, which means it can’t prove causation, but the sheer size of the cohort and consistency of results across multiple patient populations give it real scientific weight.
Galway Meta-Analysis: Narrowing the Focus
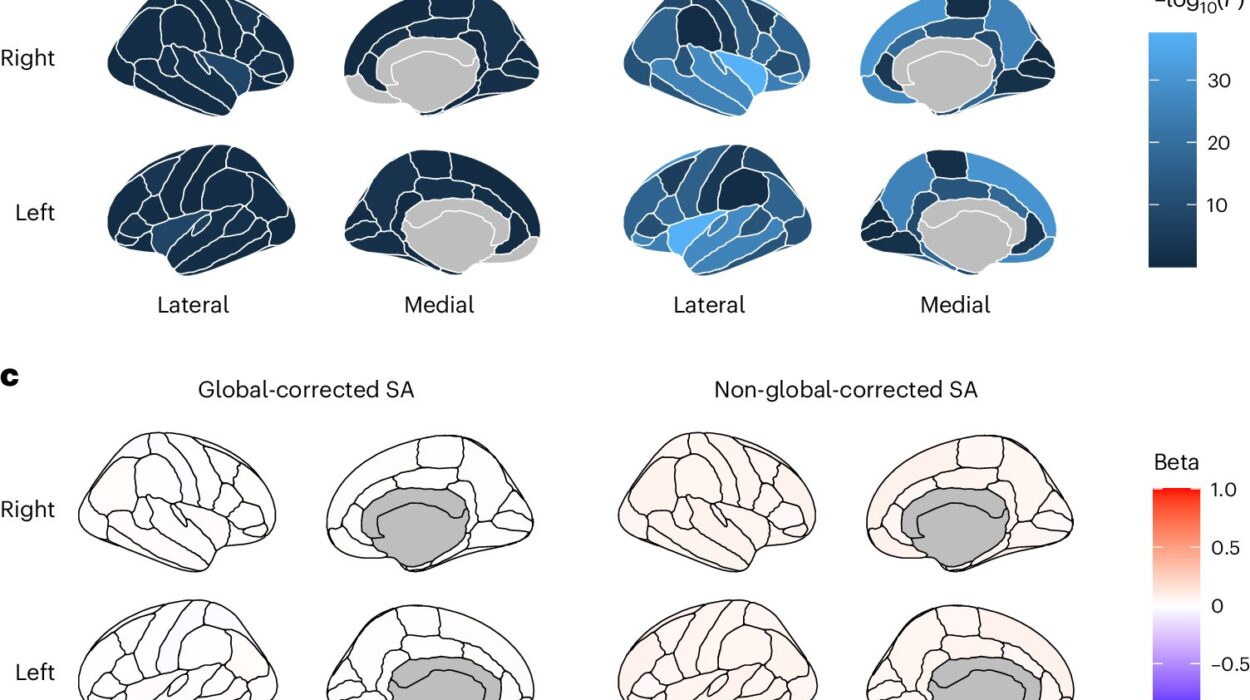
While the Florida research cast a wide net, a second study from the University of Galway in Ireland zoomed in with a fine-tooth comb. The team conducted a rigorous meta-analysis of 26 randomized clinical trials involving more than 164,000 participants, specifically focusing on whether GLP-1 receptor agonists, SGLT2 inhibitors, or pioglitazone (another older diabetes drug) were linked to changes in dementia risk.
The result? Only GLP-1 receptor agonists showed a statistically significant reduction in dementia incidence. Neither SGLT2 inhibitors nor pioglitazone appeared to have the same protective effect.
This suggests that while SGLT2 inhibitors might still be helpful in some contexts, GLP-1 agonists are emerging as uniquely potent neuroprotective agents, potentially capable of influencing the trajectory of cognitive decline in ways we hadn’t previously imagined.
How Exactly Could GLP-1 Drugs Protect the Brain?
So what’s the mechanism here? Why would a drug that helps control blood sugar also safeguard the brain?
It turns out GLP-1 receptor agonists are more than metabolic multitaskers. In preclinical studies with animals, these medications have demonstrated several brain-specific effects:
- Reduced neuroinflammation – a key driver of cognitive decline.
- Improved synaptic plasticity – essentially making brain cells more adaptable and efficient.
- Decreased accumulation of amyloid-β and tau proteins – the biological villains behind Alzheimer’s disease.
- Enhanced blood flow and vascular health – critical for maintaining oxygen and nutrient supply to brain tissue.
These actions create a neurological environment that is more resilient, less toxic, and better able to maintain cognitive function over time.
“We Are Only at the Precipice”: The Road Ahead
Dr. Diana Thiara, a neurologist at the University of California, San Francisco, authored a recent JAMA Neurology editorial responding to this growing body of evidence. Her tone is optimistic—but measured.
She describes the brain effects of GLP-1 drugs as “highly promising,” especially with newer formulations like semaglutide, which have stronger and longer-lasting receptor activity. But she also emphasizes that we are still in the early stages of understanding their full potential.
“We are only at the precipice,” Thiara writes, pointing to emerging research on dual and triple hormone agonists—next-gen drugs that may pack even more powerful benefits for the brain and body alike.
Several major clinical trials are already in motion. The EVOKE and EVOKE Plus trials are currently investigating whether semaglutide can directly slow cognitive decline in patients with early-stage Alzheimer’s. Results from these trials, expected over the next few years, could fundamentally reshape how we treat both diabetes and dementia.
Not Without Risks: The Side Effects Puzzle
Of course, no drug is without downsides. GLP-1 receptor agonists are generally well-tolerated, but common side effects include:
- Nausea
- Vomiting
- Diarrhea
- Reduced appetite (sometimes leading to loss of lean muscle mass)
The latter is particularly concerning in older adults, who are already vulnerable to sarcopenia, the age-related loss of muscle. Muscle mass isn’t just about strength—it’s also crucial for metabolic health and mobility. That’s why some experts urge caution when prescribing these drugs to elderly patients, especially those already frail.
Rare but serious side effects include:
- Pancreatitis
- Potential concerns about thyroid tumors (seen in animal studies but not yet in humans)
Because of these risks, it’s crucial for patients and providers to weigh the pros and cons carefully, especially when considering off-label uses like dementia prevention.
A Paradigm Shift in the Making?
The idea that a widely prescribed diabetes drug might also shield us from one of the most devastating neurodegenerative diseases of our time is more than just medically intriguing—it’s potentially transformative.
If future studies confirm the neuroprotective benefits of GLP-1 receptor agonists, we could be looking at a new paradigm in dementia prevention and treatment. It would mean that doctors, in managing a patient’s metabolic health, may also be offering a layer of defense against cognitive decline—a true win-win in an aging population.
This shift would also underscore a larger lesson in medicine: sometimes, the most powerful new treatments are hiding in plain sight, waiting for us to see them through a different lens.
References: Huilin Tang et al, GLP-1RA and SGLT2i Medications for Type 2 Diabetes and Alzheimer Disease and Related Dementias, JAMA Neurology (2025). DOI: 10.1001/jamaneurol.2025.0353
Allie Seminer et al, Cardioprotective Glucose-Lowering Agents and Dementia Risk, JAMA Neurology (2025). DOI: 10.1001/jamaneurol.2025.0360
Diana Thiara, GLP-1 Receptor Agonists—From Breakthroughs in Cardiometabolic Treatment to Emerging Neuroprotective Potential, JAMA Neurology (2025). DOI: 10.1001/jamaneurol.2025.0237