Beneath the surface of our skin, in the flowing rivers of blood coursing through our veins, an unseen army stands watch. These are not warriors in armor or soldiers with weapons, but cells—tiny, invisible sentinels with a sacred duty: to protect the body from invaders. They are our white blood cells, and they carry out this mission without rest, often without thanks, and usually without our awareness. Yet without them, even the simplest scratch or common cold could become fatal.
White blood cells—or leukocytes—are the vanguard of the human immune system. They operate silently, tirelessly, and with breathtaking coordination, forming a living shield against bacteria, viruses, parasites, and even our own damaged cells that turn against us. Their story is one of ceaseless vigilance, of life-and-death battles fought in microscopic landscapes. To understand how they fight infection is to glimpse the profound intelligence of nature and the exquisite complexity of the human body.
Born in the Bone: The Origins of White Blood Cells
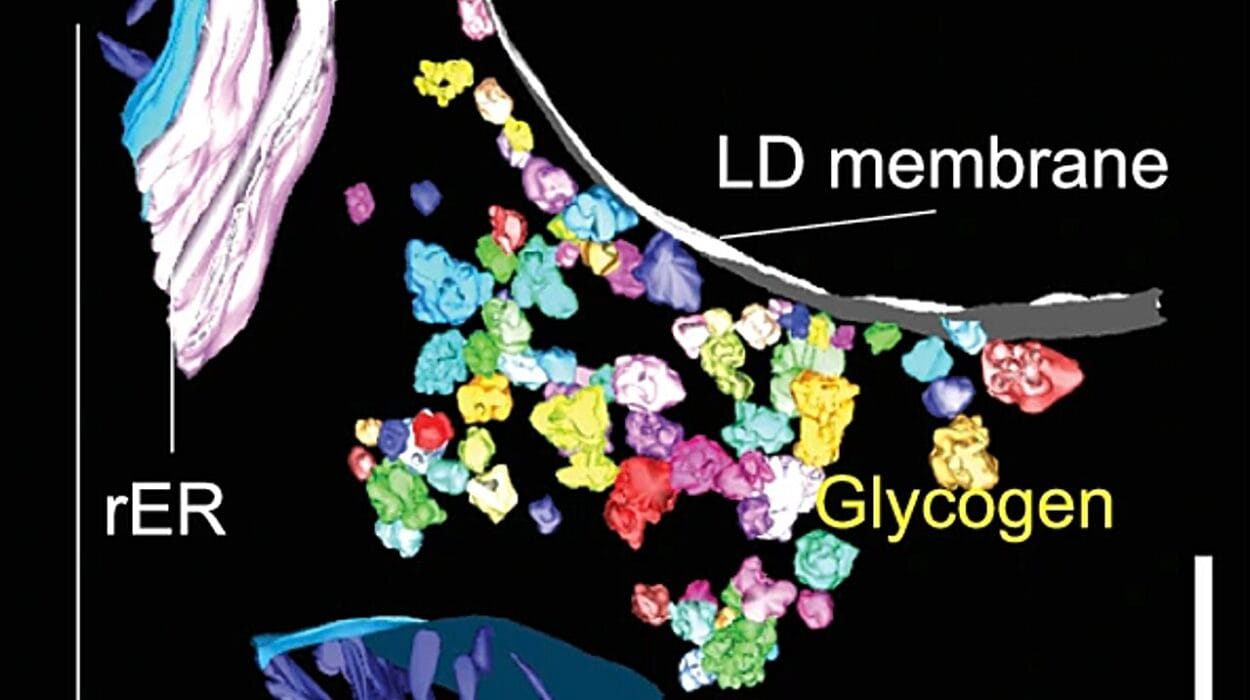
All white blood cells begin their lives deep within the marrow of our bones. This may seem an unlikely place for heroism to begin, but the bone marrow is not a lifeless structure. It is, in fact, a vibrant, soft tissue teeming with potential. Within this crucible, hematopoietic stem cells divide and differentiate into the many types of blood cells—including the red cells that carry oxygen, the platelets that help blood clot, and the versatile white cells that fight infection.
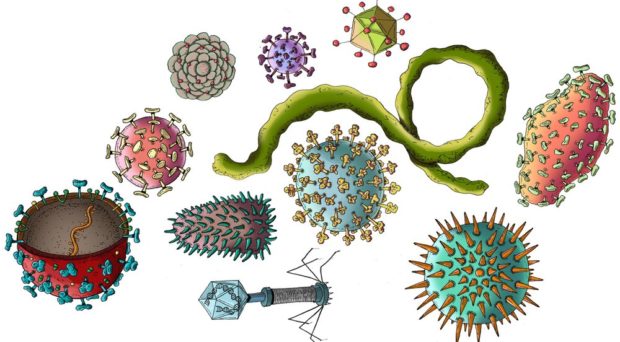
From these stem cells arise five major families of white blood cells: neutrophils, lymphocytes, monocytes, eosinophils, and basophils. Each has its own specializations, tactics, and role in the immune orchestra. Though vastly different in shape, function, and behavior, all are bound by a shared purpose: to defend the integrity of the human body.
Their journey from marrow to battlefield is rapid and purposeful. Once matured, many white blood cells enter the bloodstream, patrolling continuously. Others remain stationed in tissues, acting as sentries. They move with intention, flowing with the blood or migrating toward signals of danger. And when that signal is raised—when an infection begins—these cells spring into action with remarkable speed and precision.
The First Responders: Neutrophils and the Innate Immune Response
When a pathogen—say, a bacterium—breaches the body’s barriers, perhaps through a cut in the skin or a droplet inhaled into the lungs, it encounters the body’s first line of immune defense. This is the innate immune system: fast, nonspecific, and brutal. And at the heart of this system are the neutrophils.
Neutrophils are the most numerous of all white blood cells and among the most aggressive. They are the shock troops, the first to arrive at the site of infection. They don’t ask questions. They don’t wait for confirmation. When a chemical distress signal—called a chemokine—is released from an injured or infected site, neutrophils rush toward it, navigating by gradients of scent like bloodhounds.
Upon arrival, neutrophils unleash their arsenal. They engulf bacteria through phagocytosis, surrounding and digesting them with enzymes housed in lysosomes. They release reactive oxygen species—chemical weapons that damage or kill microbes. They even sacrifice themselves by exploding in a burst of DNA and proteins, forming “neutrophil extracellular traps” that ensnare invaders in a sticky web of destruction.
But neutrophils are not surgical in their attacks. They often damage nearby tissues, leading to inflammation, pain, and redness. This is the price of urgency: the body is willing to endure some collateral damage if it means stopping the infection before it spreads. Once their mission is complete, neutrophils die in droves and are cleared away by scavenger cells. Their sacrifice is the first act in a larger immune drama.
Calling in the Specialists: Monocytes and Macrophages
Where neutrophils strike fast, monocytes arrive more slowly but with greater versatility. Born in the marrow, monocytes circulate in the blood but transform into macrophages when they enter tissues. The word “macrophage” means “big eater,” and it is apt: these cells are voracious. They engulf not just bacteria, but dead cells, debris, and anything else that doesn’t belong.
Macrophages are more than cleaners, though. They are information brokers. As they digest pathogens, they break them into fragments—antigens—and present these fragments on their surface using special proteins called MHCs (major histocompatibility complexes). In doing so, they serve as living bulletin boards, displaying “wanted posters” for other immune cells to examine.
This antigen presentation is what initiates the adaptive immune response, a more specific and powerful system of defense. While neutrophils and macrophages are capable of defeating many minor infections on their own, the adaptive response is called upon for more serious threats—ones that require memory, strategy, and precision.
The Generals and Assassins: Lymphocytes and the Adaptive Immune Response
If neutrophils are the foot soldiers and macrophages the scouts, then lymphocytes are the strategists and elite operatives of the immune system. The lymphocytes come in two primary types: B cells and T cells. They are not only capable of identifying specific invaders but also of remembering them, ensuring a faster and stronger response in future encounters.
B cells are the architects of antibodies—proteins that bind to antigens with exquisite specificity. Once activated by an antigen (usually with the help of a T cell), a B cell becomes a plasma cell, churning out thousands of antibodies every second. These antibodies flood the bloodstream, coating pathogens and marking them for destruction. Some antibodies neutralize viruses directly, blocking their entry into cells. Others act as beacons, guiding phagocytes to their targets.
T cells, on the other hand, operate through direct contact. Helper T cells (CD4+ T cells) act as conductors, coordinating the entire immune response. They activate B cells, summon macrophages, and enhance the killing power of other cells. Cytotoxic T cells (CD8+ T cells) are more solitary and lethal. When they detect a virus-infected cell or a cancerous cell displaying abnormal antigens, they kill it without hesitation, using enzymes to trigger apoptosis, or programmed cell death.
Together, B and T cells create a personalized immune response tailored to the exact nature of the threat. And once the danger has passed, some of these cells remain behind as memory cells—ready to leap into action if the same pathogen ever returns.
The Rare and the Powerful: Eosinophils, Basophils, and Mast Cells
Not all white blood cells are generalists. Some are specialists, designed for very specific threats. Eosinophils, for example, are crucial in fighting parasitic infections—particularly worms that are too large to engulf. These cells release toxic granules directly onto the invader’s surface, damaging it from the outside.
Basophils and their close cousins, mast cells, play key roles in allergic responses and inflammation. They release histamine and other chemicals that increase blood vessel permeability, allowing more immune cells to reach the site of infection. While this is beneficial in fighting some pathogens, it can become problematic when the immune system overreacts to harmless substances—such as pollen or food—resulting in allergic reactions.
Though these cells are few in number, their impact can be profound. In some cases, like asthma or anaphylaxis, their overactivity can even become life-threatening. Yet in the right circumstances, they contribute powerfully to the body’s defense.
Balancing Attack and Restraint: The Regulation of Immunity
The immune system must strike a delicate balance. Too weak, and the body succumbs to infection. Too strong, and it risks attacking its own tissues. White blood cells, therefore, operate within a finely tuned regulatory system that modulates their activity based on need.
Regulatory T cells help maintain this balance. They suppress the immune response once an infection has been cleared, preventing excessive inflammation and autoimmune reactions. When this regulation fails, the consequences can be dire. Conditions like lupus, rheumatoid arthritis, and multiple sclerosis occur when the immune system turns on the body it is meant to protect.
Additionally, some pathogens have evolved clever ways to evade detection. HIV, for instance, specifically targets CD4+ T cells, gradually dismantling the immune system. Other viruses lie dormant in cells, invisible to patrolling white cells. The arms race between pathogens and white blood cells is ongoing and relentless.
Infection and the Orchestration of Defense
When infection begins, it is not a random flurry of activity—it is an orchestration. White blood cells work in synchrony, passing signals like musical notes in a symphony. Chemical messengers called cytokines and interleukins coordinate the timing, location, and intensity of the response.
This orchestration begins with danger signals, either from injured cells or microbial molecules recognized by pattern recognition receptors. These alerts trigger a cascade of events: the release of inflammatory chemicals, the dilation of blood vessels, and the migration of white blood cells from blood to tissue.
In the midst of battle, cells constantly communicate. They assess the threat, adapt their strategy, and adjust their tactics. They die and are replaced. They remember and learn. And they never rest.
Vaccines and the Training of White Blood Cells
One of humanity’s greatest achievements has been the ability to train white blood cells in advance of an infection. This is the principle behind vaccination. By introducing harmless components of a pathogen—often inactivated viruses, bacterial proteins, or genetic material—vaccines stimulate the adaptive immune system to generate memory B and T cells without causing illness.
These memory cells remain on patrol for years, even decades, primed to respond instantly if the real pathogen appears. The result is immunity: a prepared and rapid defense that can prevent disease before it takes hold.
Vaccination is, in essence, education for white blood cells. It teaches them what to look for, what to attack, and how to respond. It is a triumph of science and a testament to the adaptability of the immune system.
When the System Fails: Immunodeficiency and Leukemia
Sometimes, white blood cells fail not from neglect, but from internal failure. Immunodeficiency diseases, such as Severe Combined Immunodeficiency (SCID), leave individuals defenseless, often from birth. Even a mild infection can become deadly without functional white cells.
Leukemia is another tragic manifestation. It is a cancer of white blood cells, where immature or abnormal cells multiply uncontrollably. These rogue cells do not fight infection; they overwhelm the bloodstream and crowd out healthy cells. Though treatments have improved dramatically, leukemia remains a powerful reminder of what happens when the immune system turns against itself.
White Blood Cells and the Future of Medicine
In the 21st century, white blood cells are not only guardians of health—they are becoming tools of healing. Scientists have learned to harness their power through immunotherapy, reprogramming T cells to fight cancer with extraordinary precision. CAR-T cell therapy, for example, engineers a patient’s own T cells to recognize and destroy cancerous cells.
Other therapies involve stimulating white blood cells with synthetic molecules, or using monoclonal antibodies—lab-made versions of natural antibodies—to target infections and tumors. The age of precision medicine is deeply tied to the abilities of white blood cells.
In infectious disease, autoimmunity, allergy, and cancer, white blood cells are no longer just responders. They are becoming therapeutic agents, tailored by human hands and guided by natural intelligence.
The Inward Miracle: A Final Reflection
To contemplate the role of white blood cells is to recognize that our very survival depends on processes we never see. Every moment of every day, millions of cells are born, migrate, fight, and die for us. They respond to threats before we ever feel sick. They heal us before we know we were in danger.
And yet they do not act blindly. These cells, each only a few micrometers across, navigate chemical messages, recognize patterns, and make decisions. They are, in a sense, intelligent—not in the way we think of consciousness, but in their ability to sense, respond, and learn.
Their story is not only biological—it is poetic. In their unseen labor, white blood cells embody the principles of vigilance, sacrifice, coordination, and memory. They do not boast, and they do not rest. They are always watching, always ready.
So the next time you recover from a cold, or avoid an infection that never quite took hold, remember them—the silent protectors in your blood. The white blood cells. The tireless guardians of life.