Chronic lung infections do not always announce themselves with drama. Sometimes they live quietly for years, weakening patients slowly, surviving in the shadows of the lungs despite aggressive treatment. One of the most difficult of these hidden pathogens is Mycobacterium avium, a microbe increasingly found in people with chronic lung disease across the world. Now, a team of scientists in Dublin has shown, with unprecedented clarity, how this bacterium evolves inside human lungs over years — learning to resist, adapt and persist.
Researchers from the Trinity Translational Medicine Institute and the Irish Mycobacterial Reference Laboratory at St James’s Hospital analyzed the genetic “diary” of the bacteria inside real patients, not in petri dishes. Their findings, published in Genome Medicine, offer a rare time-lapse view of microbial evolution unfolding inside the body. What they learned may explain why so many treatments fail and how doctors could finally outsmart an infection that keeps coming back.
When Cure Isn’t a Cure
Treating M. avium lung disease is a long, exhausting ordeal. It typically requires more than a year of multiple antibiotics taken together — yet nearly half of patients still do not clear the infection. Worse, many who do clear it become ill again. For years, doctors assumed such returns were relapses, meaning the original bacteria had survived. But the new genomic study paints a different picture.
By sequencing nearly 300 samples from patients across Ireland, the UK, and Germany — including two dozen from St James’s Hospital — the team discovered that patients were often not battling the same strain continuously. Instead, they were reinfected repeatedly with new strains from the environment. Some of these strains were nearly identical to ones circulating in other European countries, suggesting common environmental reservoirs such as water systems, soil, or air exposure.
This insight changes the narrative: the disease is not only stubborn inside the body — it may be waiting outside, ready to come back.
A Bacterium That Evolves in Real Time
By reading the DNA of the bacteria collected from the same patient over years, scientists could track how M. avium changes under pressure. They observed that the bacterium acquires roughly one new genetic mutation per year — slow, but steady enough to matter when an infection lasts five or ten years.
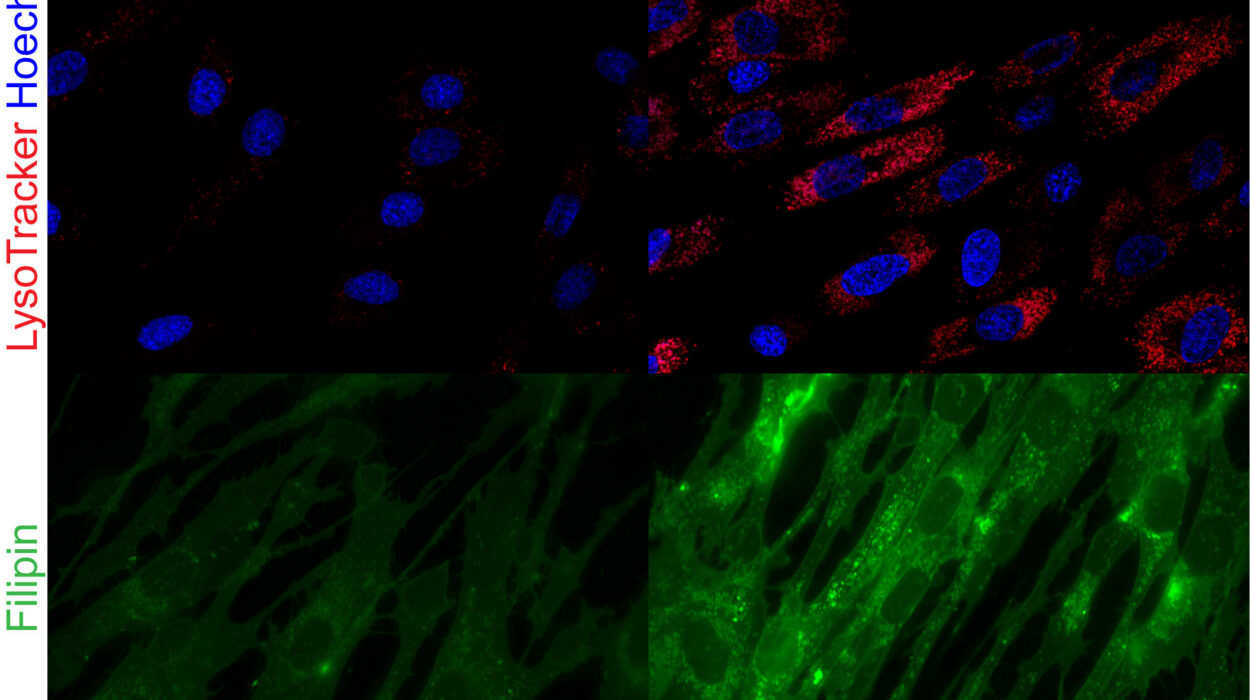
Most importantly, they identified 13 genes that showed clear signs of adaptive evolution under stress. These genetic changes made the bacteria better at withstanding antibiotics, surviving in low oxygen, resisting immune attack, and forming protective biofilms — glue-like communities that shield them from harm. Remarkably, some of these genes had never before been linked to survival inside human lungs.
Lead researcher Dr. Aaron Walsh explained that the study demonstrates the organism is not static. It is changing on the inside, responding to the battlefield of the lung and learning as it survives. Real-time evolution is not an abstract concept here; it is a biological strategy happening silently while treatment is underway.
A Global Infection Hiding in Plain Sight
One surprising discovery was that Irish bacterial strains were genetically nearly indistinguishable from those isolated in the UK and Germany — even though the patients had never met or traveled. This suggests shared external sources, perhaps tap water, medical equipment, or a widely distributed environmental niche. Rather than a private infection trapped inside one lung, M. avium appears to move through countries and populations like an invisible migrant, adapting as it goes.
Dr. Emma Roycroft, co-author of the study, noted that some of the newly identified genes are involved in oxidative stress responses and biofilm formation — two processes that likely give the bacterium its endurance inside hostile tissue. These pathways now represent targets for next-generation drugs designed not just to kill bacteria, but to interrupt their survival strategies.
A Path Toward Smarter Treatments
This research marks the first time whole-genome sequencing has been used to follow M. avium infections over many years within the human body. The team is now moving from decoding to intervention. Their next steps include testing in the laboratory how the 13 adaptive genes function, expanding sequencing to catch changes missed by current techniques, and collecting environmental samples to locate real-world sources of reinfection.
The long-term vision is not just new antibiotics, but new treatment logic: therapies shaped around how the bacterium actually evolves inside patients, not how it behaves in theory.
Why This Matters
Chronic infections like M. avium reshape lives. Patients lose lung function slowly. They undergo months of toxic therapies. They endure exhaustion, coughing, weight loss, and the emotional toll of recurrence. This study offers a moment of clarity — a shift from fighting an invisible enemy to understanding its tactics.
By exposing the genetic footsteps of a pathogen over time, the research gives doctors something they rarely have in chronic infectious disease: foresight. It shows that persistence is not mysterious luck, but a measurable, evolving strategy that can be countered once understood.
This work stands as a reminder that the longest battles in medicine are often fought not with force but with knowledge — and that even a microbe adapting one mutation at a time can be disarmed when its playbook is finally opened.
More information: Aaron M. Walsh et al, Genomic characterisation of recurrent Mycobacterium avium isolates from chronically infected patients reveals patterns of within-host evolution, Genome Medicine (2025). DOI: 10.1186/s13073-025-01549-y