In just three decades, obesity rates have more than doubled, now affecting over a billion people worldwide. This is not merely a matter of extra pounds — it’s a public health crisis tied to a tangle of serious conditions, from type 2 diabetes and cardiovascular disease to chronic kidney disease and several cancers.
Doctors and patients have long relied on a familiar trio of solutions: lifestyle changes, bariatric surgery, and powerful new drugs like Ozempic or Wegovy. But while these treatments can be effective, they are not perfect. Many people face high costs, limited access, unpleasant side effects, or the frustrating reality of regaining lost weight over time.
Now, researchers at the Salk Institute for Biological Studies believe a new class of treatments could be hiding in plain sight — or more precisely, hiding deep within the so-called “junk” DNA that makes up much of our genome. Their target: microproteins.
The Tiny Molecules with Big Potential
Microproteins are incredibly small proteins — so small, in fact, that they were overlooked for decades. Once dismissed as genetic noise, they are now emerging as powerful regulators of many biological processes. Some influence muscle function, others control cell growth, and still others may directly impact metabolism and fat storage.
The Salk team suspected that some of these microproteins might be key players in obesity. But finding them in the vast expanse of our genome is no small feat. That’s where CRISPR gene-editing technology comes in.
CRISPR: Turning the Lights On in Genomic Dark Matter
Think of the genome as a vast library — except most of its shelves are unmarked and unlit. CRISPR works like a high-tech flashlight and scalpel combined: it can both illuminate and cut out specific genes to see what happens when they are gone.
In their new study, published in Proceedings of the National Academy of Sciences, the Salk researchers used CRISPR to screen thousands of fat cell genes. They weren’t looking for the usual suspects like PPAR gamma or GLP-1, but for entirely new genes that might code for microproteins regulating fat cell growth (proliferation) or fat storage (lipid accumulation).
“CRISPR screening is extremely effective at finding important factors in obesity and metabolism that could become therapeutic targets,” explains Alan Saghatelian, senior author of the study. “The more we screen, the more disease-associated microproteins we find — and the more possibilities we have for new drugs.”
Why Current Drugs Aren’t the End of the Story
Two major obesity drug targets have dominated the last few decades:
- PPAR gamma — a master regulator of fat cell development, once the darling of diabetes drug research. But PPAR gamma drugs often caused unwelcome side effects like bone loss and weight gain.
- GLP-1 — a natural hormone that curbs appetite and regulates blood sugar. Drugs like Ozempic and Wegovy have transformed obesity treatment, but they, too, come with drawbacks: nausea, digestive discomfort, and muscle loss among them.
Both PPAR gamma and GLP-1 share something in common — they are relatively small molecules or peptides, fitting into the category of microproteins. That track record suggests there may be many more therapeutic gems hidden in the genomic shadows.
Discovering Adipocyte-smORF-1183
After screening their massive gene library, the Salk team narrowed the field to 38 potential microproteins that seemed to influence lipid droplet formation — a hallmark of fat storage. Then came the painstaking process of verification.
In the end, one candidate emerged with clear evidence of function: a newly confirmed microprotein the researchers named Adipocyte-smORF-1183. Laboratory tests suggest it plays a role in controlling lipid droplet formation in fat cells, meaning it could be directly involved in how the body stores fat.
While it’s far too early to say whether Adipocyte-smORF-1183 will become a drug target, its discovery proves the CRISPR screening approach works — and can find molecules that might otherwise remain invisible.
From Mice to Humans
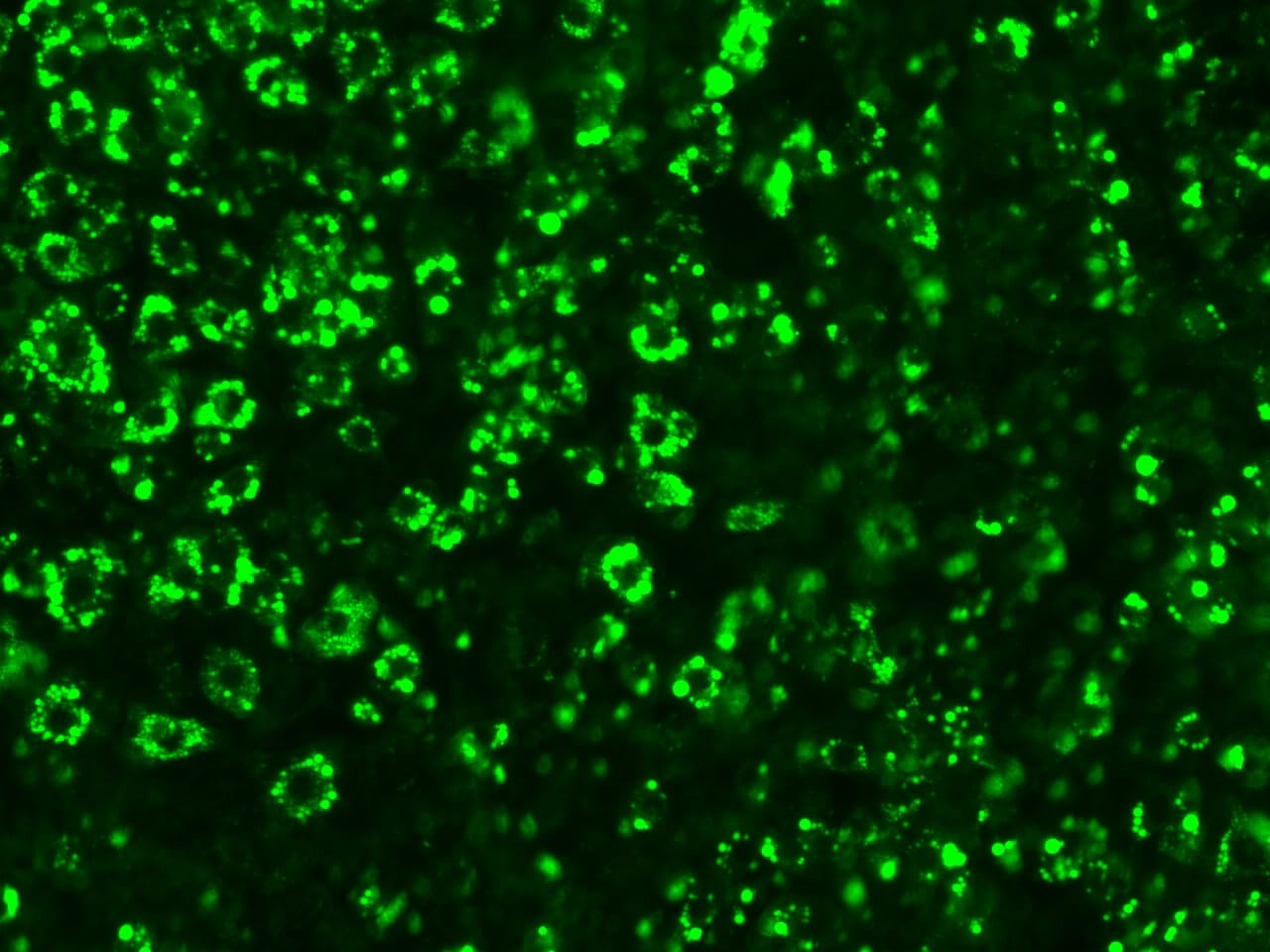
The current study was performed using mouse fat cell models, including pre-fat cells that can be observed as they mature into fully functional fat cells. This allowed researchers to track the genetic influence on every stage of fat development.
The next step is to repeat the process in human fat cells to see whether the same microproteins — including Adipocyte-smORF-1183 — behave similarly. If they do, the door opens to designing entirely new classes of obesity and metabolic disorder drugs.
A Future Beyond “Junk” DNA
For decades, vast regions of our genome were written off as useless. But as technology catches up with biology, these stretches of DNA are being reinterpreted as a treasure trove of hidden proteins and regulatory elements.
Saghatelian hopes that the success of this study will encourage others to explore this “dark genome” with the latest tools. “That’s the goal of research,” he says. “You keep going. It’s a constant process of improvement — better technology, better workflows, and eventually, better treatments.”
If that vision becomes reality, the next breakthrough in obesity treatment may not come from a flashy new diet drug or a surgical innovation — but from a microscopic protein once buried in what we thought was genetic trash.
More information: Victor J. Pai et al, CRISPR–Cas9 screening reveals microproteins regulating adipocyte proliferation and lipid metabolism, Proceedings of the National Academy of Sciences (2025). DOI: 10.1073/pnas.2506534122