For years, immunotherapy has promised a revolution in cancer treatment. By harnessing a patient’s own immune system, it has delivered stunning successes—helping some patients achieve long-term remission where traditional therapies failed. But for others, especially those with aggressive cancers like triple-negative breast cancer (TNBC), the promise has often fallen short. Tumors find ways to hide, silencing immune alarms and evading destruction.
Now, a new study published in Science Signaling shines light on one of the secret weapons tumors use to escape. At the center of this discovery is a little-known genetic player: a long noncoding RNA (lncRNA) called EPIC1. Researchers have uncovered how this molecule helps cancer cells shield themselves from immune attack—and how switching it off could transform the effectiveness of immunotherapy.
The Hidden Language of Cancer: What Are lncRNAs?
Our DNA is filled with stretches that do not produce proteins, long dismissed as “junk.” But far from useless, many of these regions produce lncRNAs, RNA molecules that fine-tune cellular behavior. In cancer, they can act as powerful regulators, flipping switches that help tumors grow, spread, and resist treatment.
EPIC1 is one such lncRNA. Until recently, it was a shadowy figure in cancer biology, known only for its role in promoting tumor growth. The new study reveals something more troubling: EPIC1 can manipulate the immune system itself. By partnering with a protein called EZH2, a histone methyltransferase, it creates a molecular shield that hides tumors from detection.
How Tumors Evade Immune Detection
Normally, cancer cells produce abnormal signals—like double-stranded RNA (dsRNA) from so-called retroelements (REs), ancient pieces of viral-like DNA embedded in our genomes. These dsRNAs act as danger flags, alerting the immune system to unleash antiviral defenses, including the type I interferon (IFN) response, which recruits T cells and macrophages to attack.
But in cancer cells with high EPIC1 activity, this alarm system is silenced. EPIC1 and EZH2 repress the expression of retroelements, suppressing dsRNA buildup. With the warning signals muted, the immune system remains blind, and immunotherapy drugs like pembrolizumab (a PD-1 checkpoint inhibitor) struggle to work.
As the study authors put it, “Collectively, these results suggest that EPIC1 suppression promotes an antiviral-like type I IFN response with potential antitumor effects.”
Putting the Discovery to the Test
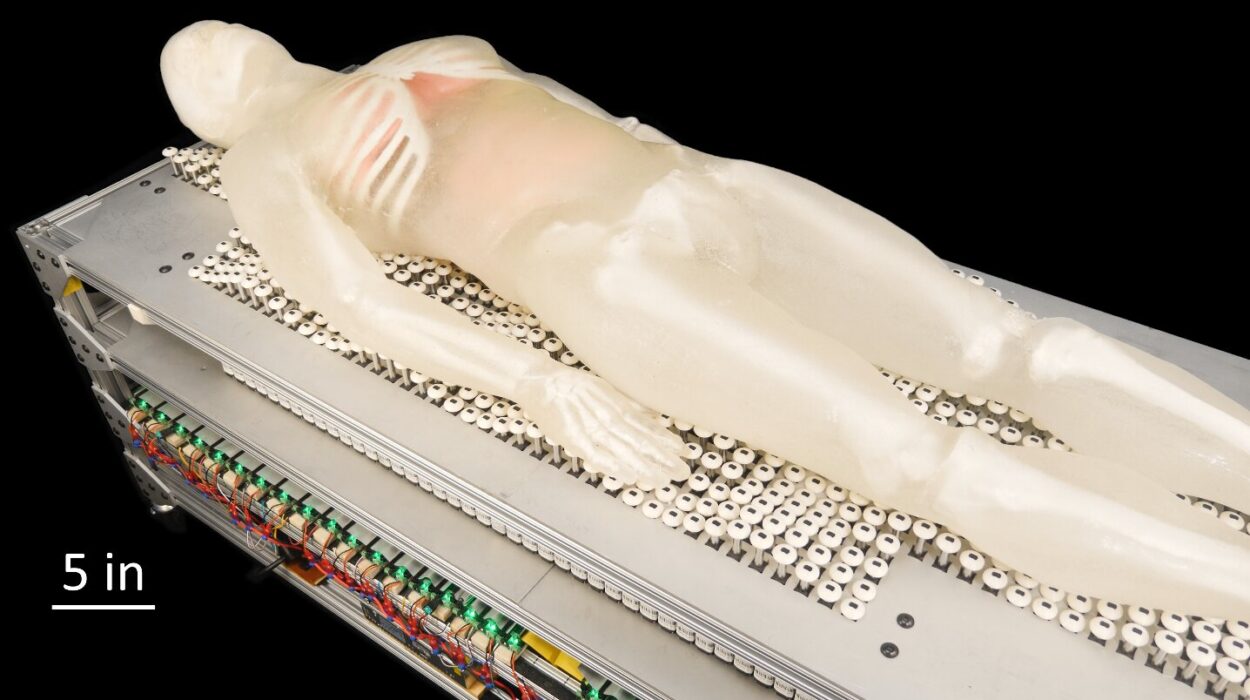
To test what happens when EPIC1 is shut down, the researchers turned to an ingenious model: humanized mice—mice carrying human immune systems. Using RNA interference to “knock down” EPIC1 in cancer cell lines, they implanted these cells into the mice and treated them with pembrolizumab.
The results were striking. Tumors shrank. T cells and inflammatory macrophages flooded the cancer environment. The once-resistant cancers began to respond to immunotherapy. In triple-negative breast cancer, one of the most stubborn forms of the disease, the combination of EPIC1 knockdown and pembrolizumab significantly slowed tumor growth.
Coculture experiments reinforced the finding: when cancer cells lacking EPIC1 were exposed to T cells or monocytes in the lab, immune attack was far more effective.
“EPIC1 can be a potential therapeutic target in combination with immunotherapy,” the researchers write.
Hope for Patients with Few Options
For patients with triple-negative breast cancer, this research is especially meaningful. TNBC accounts for about 10–15% of breast cancers and disproportionately affects younger women. It is notoriously aggressive and lacks the hormone receptors that make other breast cancers easier to target with drugs. Current treatment options are limited, and survival rates remain lower than for other breast cancer types.
The discovery of EPIC1’s role in immune evasion suggests a new strategy: combining immunotherapy with targeted RNA interventions to unmask hidden tumors. If successful in humans, it could turn previously resistant cancers into treatable ones.
Cautious Optimism: The Road Ahead
Despite the excitement, scientists urge caution. The work so far has been conducted in cell cultures and mouse models. Human cancers are more complex, and clinical trials will be needed to determine whether targeting EPIC1 is safe and effective. Furthermore, lncRNAs form a vast and intricate regulatory network. Turning off one may have ripple effects that need to be carefully studied.
Still, the promise is real. By revealing the molecular tricks cancers use to escape, researchers are building a roadmap to outsmart them. If EPIC1 can be safely silenced, it may one day transform immunotherapy for not only TNBC but also prostate, pancreatic, and other cancers where immune resistance remains a barrier.
A Future Where the Immune System Always Wins
At its heart, this research is about giving the immune system back its voice. Cancer thrives on silence—silencing alarm signals, silencing immune responses, silencing hope. By uncovering how EPIC1 and EZH2 suppress those alarms, scientists have found a way to restore the immune system’s ability to fight back.
For patients and families living with the uncertainty of aggressive cancers, this work offers more than a scientific advance. It offers a glimpse of a future where no tumor can hide, where the immune system is empowered, and where the promise of immunotherapy can finally be fulfilled for all.
More information: Dhamotharan Pattarayan et al, The lncRNA EPIC1 suppresses dsRNA-induced type I IFN signaling and is a therapeutic target to enhance TNBC response to PD-1 inhibition, Science Signaling (2025). DOI: 10.1126/scisignal.adr9131