For millions around the world living under the heavy fog of major depressive disorder, the search for relief can feel endless. Traditional antidepressants often take weeks to work—if they work at all—and may bring troubling side effects or simply stop being effective over time. But a new study from the University of Auckland offers an unexpected glimmer of hope from an unconventional source: microdoses of LSD, one of the most iconic psychedelic substances of the 20th century.
In an eight-week trial, researchers found that small, precisely measured doses of LSD were safe, well-tolerated, and dramatically reduced symptoms of depression—and the effects lasted for months after the treatment ended. Their findings, published in the journal Neuropharmacology, are helping to rewrite the conversation about psychedelics and mental health.
Rethinking Psychedelics
For decades, LSD (lysergic acid diethylamide) was known mainly for its role in the counterculture movement of the 1960s. But in recent years, scientists have begun re-examining its potential therapeutic power. Unlike the high-dose “trips” associated with vivid hallucinations and altered consciousness, microdosing involves taking very small amounts—far below the threshold for intoxication—on a structured schedule.
Previous studies hinted that LSD microdosing might lift mood, increase energy, and enhance creativity in healthy volunteers. Yet, questions remained about safety, tolerability, and whether those subtle benefits could translate into meaningful relief for people struggling with clinical depression.
That’s what the University of Auckland team set out to test in their Phase 2A open-label trial—the first of its kind to systematically evaluate LSD microdosing for major depressive disorder under medical supervision.
The Study: Testing Feasibility and Safety
The study enrolled 19 adults diagnosed with moderate depression. Most were already taking antidepressants, yet still experienced persistent symptoms. Their average age was 41, and the group included 15 men and 4 women.
Over the course of eight weeks, participants received 16 sublingual doses of LSD, starting at a very low 8 micrograms in the clinic and continuing at home twice per week with doses between 6 and 20 micrograms. Each participant used a custom smartphone app to record effects, track dosing, and provide feedback to researchers.
The team’s primary goal was to determine whether this regimen was feasible, safe, and tolerable—crucial steps before conducting larger, placebo-controlled studies. Safety was monitored closely with blood tests, electrocardiograms (ECG), and echocardiography, which examines heart function.
Participants were advised to avoid risky activities for six hours after dosing and to take their microdoses before 2 p.m. to reduce the risk of sleep disruption.
What the Participants Experienced
Of the 19 participants, 16 completed the full eight weeks, and compliance was near perfect—every at-home dose was verified through the study’s video logs. Only one participant withdrew due to anxiety on dosing days, and two others discontinued for reasons unrelated to the study.
On average, participants settled at a mean dose of 14.6 micrograms, comfortably within the “micro” range. Side effects were minimal: a few reported mild headaches or transient anxiety, but no one experienced hallucinations or major physiological issues.
Crucially, no serious or clinically significant adverse events occurred, and the heart safety results were reassuring. Echocardiograms and ECGs revealed no signs of heart valve abnormalities or dangerous electrical changes, concerns sometimes raised with serotonergic drugs.
The Results: A 59.5% Drop in Depression
The results were nothing short of remarkable. By the end of the eight weeks, participants’ Montgomery–Åsberg Depression Rating Scale (MADRS) scores had dropped from an average of 23.7 (moderate depression) to 9.6, reflecting a 59.5% reduction in symptoms. Even more promising, nine participants met the criteria for full remission—essentially no longer showing signs of clinical depression.
And the benefits didn’t fade quickly. When researchers checked back six months later, participants continued to show substantial improvements.
The improvements extended beyond mood. Measures of anxiety, stress, and rumination (the tendency to dwell on negative thoughts) all declined significantly, while motivation, energy, and overall quality of life improved across the board.
- HAM-A anxiety scores dropped by 51.9%.
- DASS subscales showed stress reduced by 34.9%, anxiety by 59.1%, and depression by 40.6%.
- RRS rumination scores decreased by 14.7%.
- DARS scores—reflecting pleasure and motivation—rose by 14.8%.
- And participants reported measurable gains in physical, psychological, and social well-being on the WHOQOL-BREF scale.
The numbers paint a striking picture of broad, sustained improvement—without the typical side effects associated with standard antidepressants.
Understanding Why It Works
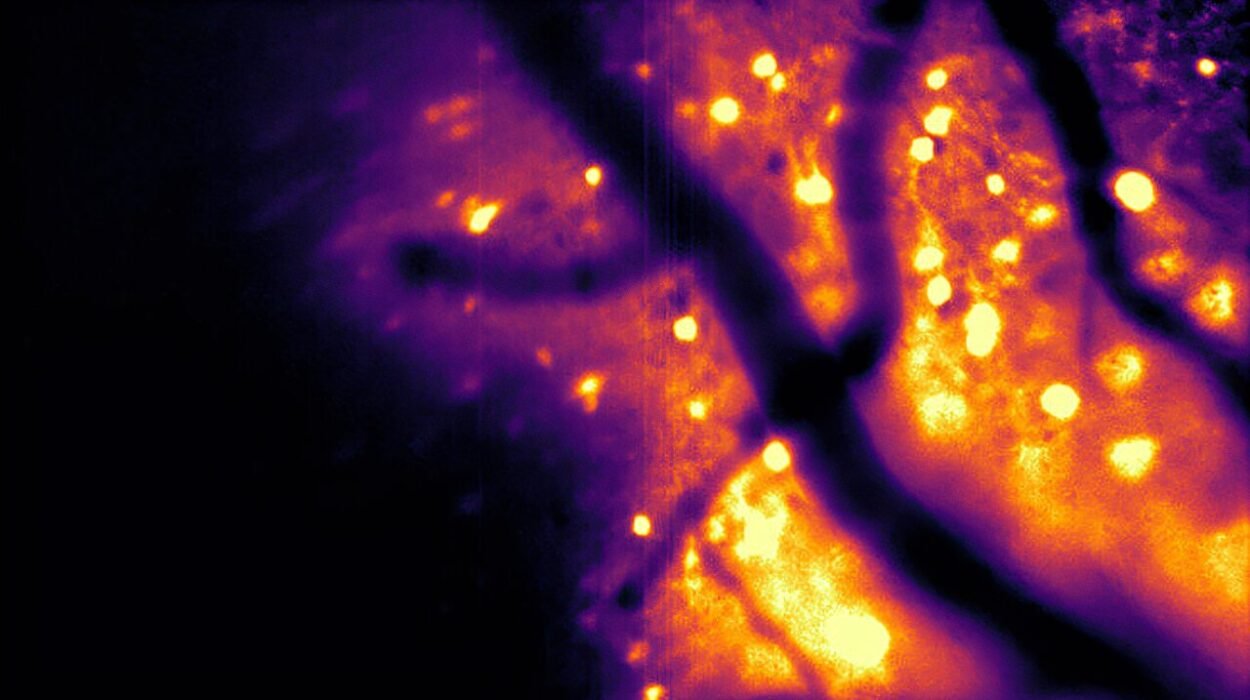
Why might microdoses of LSD help alleviate depression? While the exact mechanisms are still under study, scientists believe LSD acts on the brain’s serotonin 5-HT2A receptors, enhancing neural connectivity and promoting cognitive flexibility. This means it may help the brain “rewire” itself out of rigid patterns of negative thinking—a hallmark of depression.
Unlike traditional antidepressants, which often take weeks to build up in the system, psychedelic compounds can trigger rapid changes in mood and perspective, even at tiny doses. LSD microdosing may subtly increase openness, curiosity, and emotional resilience without producing full psychedelic effects.
The University of Auckland team was careful to stress that microdosing should not be attempted without medical oversight. Though promising, these effects were achieved under tightly controlled conditions, with comprehensive screening and monitoring for each participant.
Safety and Caution
The study’s findings are a major step forward for psychedelic medicine, but they are not an invitation to self-experimentation. Even microdoses of LSD can carry risks, particularly for people with anxiety, bipolar disorder, or certain heart conditions.
That’s why the researchers prioritized heart monitoring throughout the trial. LSD and related compounds interact with serotonin receptors that, in theory, could affect heart valve function. Fortunately, the study found no evidence of cardiac harm even after multiple months of dosing.
Still, as lead investigators note, larger randomized controlled trials are essential to confirm these early findings and ensure safety across diverse populations.
A Paradigm Shift in Mental Health Treatment
If future trials confirm these results, LSD microdosing could represent a paradigm shift in how we treat depression. It may offer a fast-acting, low-dose, and non-invasive alternative to conventional medications, potentially transforming the mental health landscape.
The implications extend beyond depression. Psychedelics are also being studied for anxiety, post-traumatic stress disorder, addiction, and even end-of-life distress. What was once dismissed as countercultural experimentation is now re-emerging as a serious frontier of neuroscience and psychiatry.
Looking Ahead
The University of Auckland team plans to launch a Phase 2B randomized controlled trial to directly compare LSD microdosing with placebo. This next stage will provide the rigorous evidence needed to move toward clinical approval and wider use.
For now, the message is one of cautious optimism. The study’s authors describe the results as “preliminary but powerful signals” of antidepressant potential. They emphasize that microdosing is not a magic cure, but it may open a door for those who have found none through traditional medicine.
The Human Side of Science
Behind the numbers lies a simple, deeply human story: people who had battled depression for years found their days a little lighter, their thoughts less heavy, their lives a bit more livable. Some spoke of renewed energy, others of finally feeling present again.
For them, and for millions still searching, this research carries a message of hope—that healing might not always come in large doses, but sometimes, in the smallest ones imaginable.
As science continues to rediscover the therapeutic potential of psychedelics, studies like this remind us that innovation often begins where curiosity meets compassion—and where the courage to look beyond stigma can illuminate entirely new paths to wellness.
More information: Dimitri Daldegan-Bueno et al, LSD microdosing in major depressive disorder: results from an open-label trial, Neuropharmacology (2026). DOI: 10.1016/j.neuropharm.2025.110762