Scientists have uncovered a surprising connection between pancreatic cancer and dementia-like behavior inside cells. In groundbreaking new research, cells in the pancreas that are at risk of turning cancerous were found to develop clumps of faulty proteins—similar to those seen in Alzheimer’s and other neurodegenerative conditions.
The discovery, published in Developmental Cell, could help unlock new ways to diagnose and treat pancreatic cancer, one of the deadliest forms of cancer. Each year in the UK alone, around 10,500 people are diagnosed with the disease, and more than 6,900 lives are lost. Unlike some cancers where survival has improved in recent decades, pancreatic cancer remains notoriously difficult to detect early and even harder to treat.
How Cells Go Wrong
The pancreas, a small but vital organ sitting just behind the stomach, helps the body digest food and regulate blood sugar. Its cells are normally highly skilled at managing proteins—making, folding, and recycling them when no longer needed. This recycling process, known as autophagy, acts like a cellular housekeeping service, breaking down old or faulty molecules to keep cells healthy.
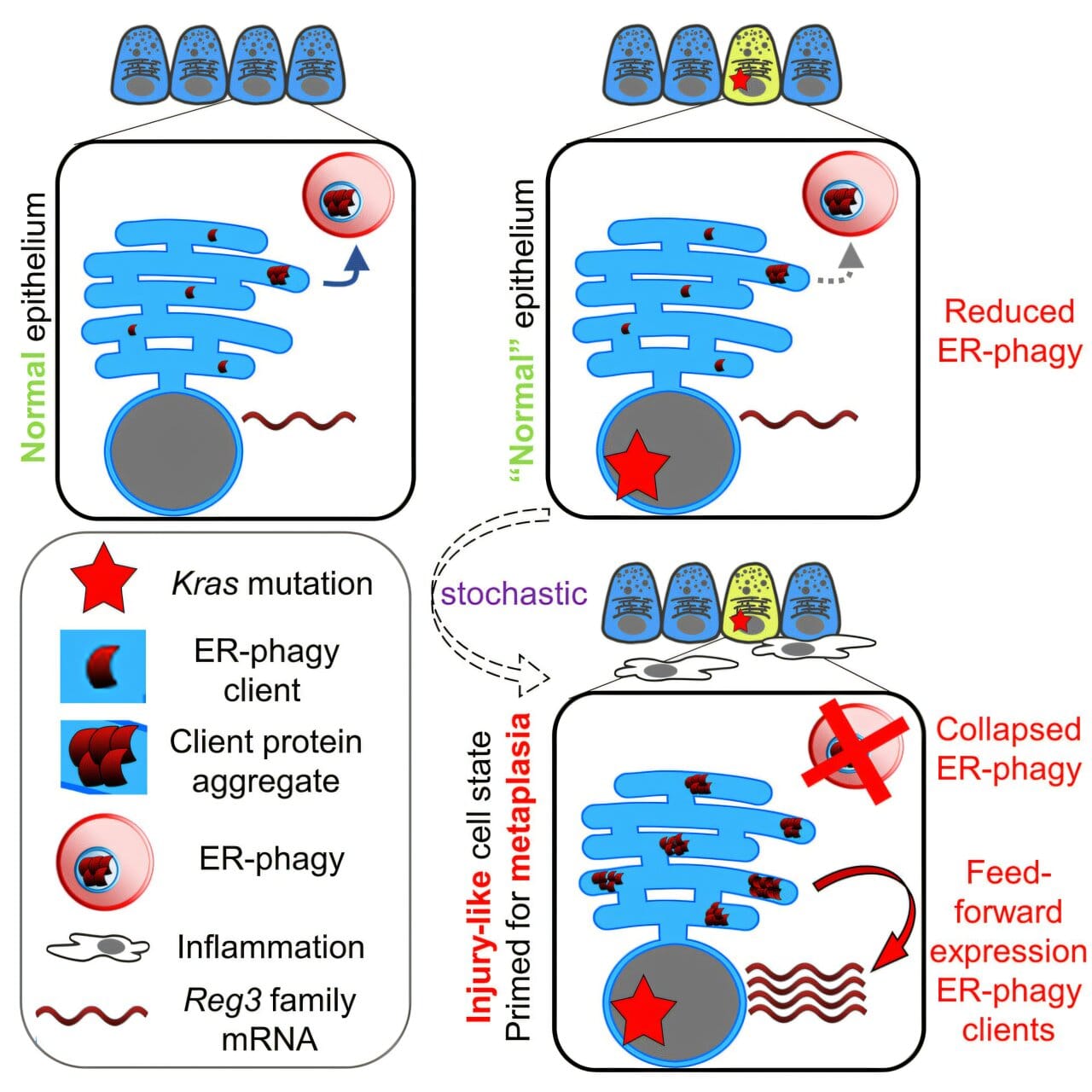
But researchers from the Cancer Research UK Scotland Centre and the University of Edinburgh discovered that in certain pancreas cells, this process breaks down. Specifically, in cells carrying a mutation in a gene called KRAS—a well-known driver of pancreatic cancer—autophagy begins to fail.
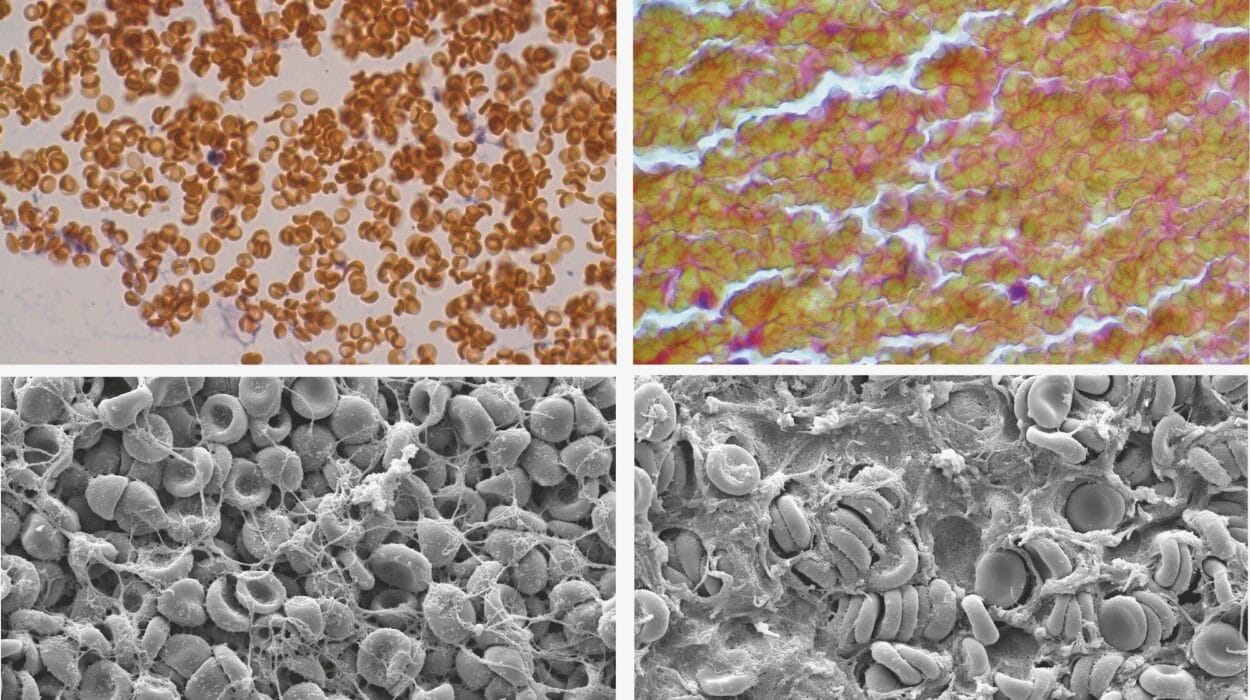
When that happens, proteins that should be recycled start to clump together. Instead of being cleared away, they gather inside the cell like piles of uncollected rubbish. The researchers likened this to the protein clumps seen in dementia, where malfunctioning proteins build up in brain cells and disrupt their function.
Dementia Inside the Pancreas
This unexpected overlap between two seemingly different diseases—cancer and dementia—has given scientists a fresh perspective.
Professor Simon Wilkinson, Cancer Research UK Senior Fellow at the Institute of Genetics and Cancer at the University of Edinburgh, explained:
“Our research shows the potential role autophagy disruption plays in the beginnings of pancreatic cancer. While early stage, we can potentially learn from research into other diseases where we see protein clumping, such as dementia, to better understand this aggressive type of cancer and how to prevent it.”
The finding suggests that before pancreatic cancer even takes hold, cells are already behaving in ways eerily similar to those observed in degenerative brain disorders.
Why Pancreatic Cancer Is So Difficult
One of the reasons pancreatic cancer is so deadly is that it usually develops silently. Symptoms often appear only once the disease has advanced and spread, leaving doctors with limited treatment options. By the time most patients are diagnosed, surgery—the only potential cure—is no longer possible.
This makes it vital to understand the very earliest steps of how healthy cells transform into cancer. By uncovering dementia-like changes inside pancreas cells, scientists may be able to identify early warning signs before tumors form.
Dr. Iain Foulkes, Executive Director of Research and Innovation at Cancer Research UK, said:
“Around 10,500 people are diagnosed with pancreatic cancer in the UK each year and, sadly, too many of those cases are found at a stage where treatment options are limited. While further work is needed, these findings could provide vital clues into how we can better understand how pancreatic cancer develops.”
When Recycling Turns Rogue
Autophagy has long been studied in cancer biology. In some cancers, tumor cells become “addicted” to autophagy, hijacking the recycling process to fuel their rapid growth. But this new research flips the idea on its head: rather than helping established cancers grow, disrupted autophagy may also play a role right at the very beginning of the disease.
The researchers believe that the double hit of a KRAS mutation and faulty autophagy could prime pancreas cells to tip into cancer. In other words, genetics alone may not be enough; when combined with problems in protein recycling, the path toward cancer becomes far more likely.
Learning From Other Diseases
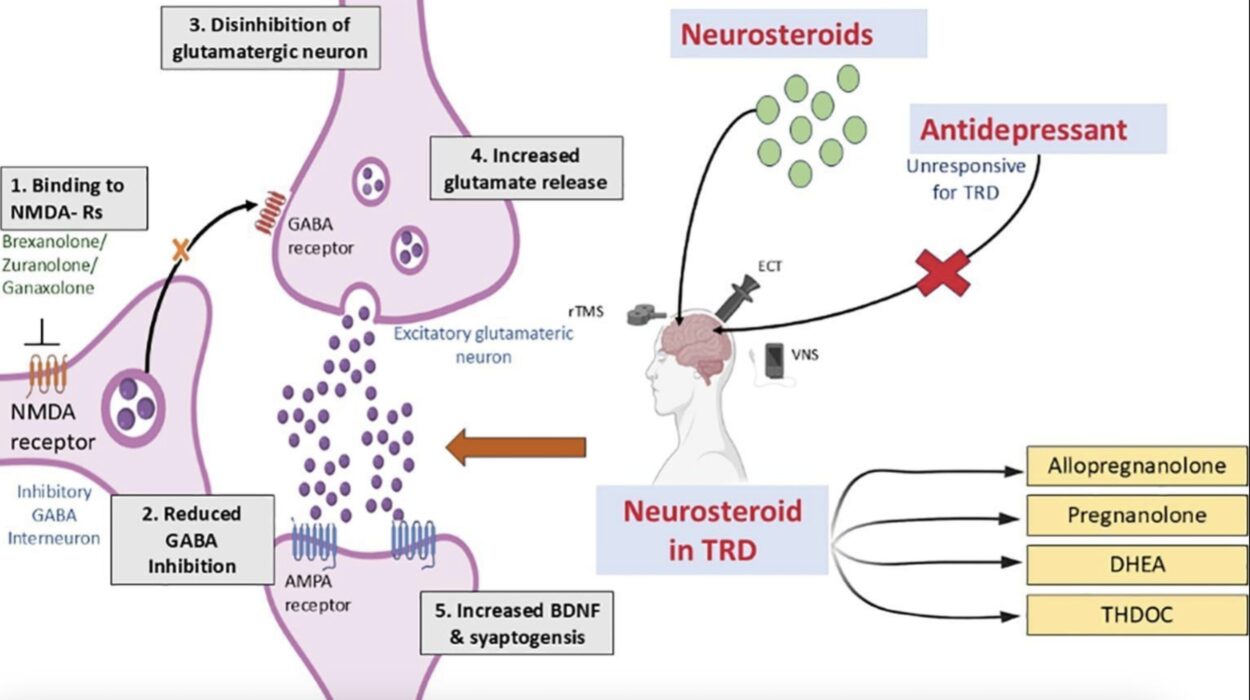
The comparison to dementia is more than a metaphor. Diseases like Alzheimer’s and Parkinson’s are heavily linked to the way cells handle proteins, and decades of research into those conditions has uncovered possible strategies for tackling protein clumping. If similar processes are at work in the pancreas, scientists could potentially repurpose knowledge—or even treatments—from the world of neurology.
The next step is to explore whether lifestyle factors such as age, sex, or diet influence how these cellular recycling problems develop. If so, it may be possible not only to predict who is at higher risk but even to find ways to reverse or slow the earliest stages of pancreatic cancer.
A Glimmer of Hope
Although pancreatic cancer remains one of the most devastating diagnoses, discoveries like this are slowly opening new doors. By peering into the microscopic machinery of the cell, scientists are beginning to see the first sparks of cancer long before tumors appear.
It is a sobering thought that the same clumping that robs people of their memories in dementia may also be pushing pancreas cells down the road to malignancy. Yet it is also a hopeful one: by drawing connections between diseases, researchers may uncover new strategies for some of the toughest medical challenges of our time.
More information: ER-phagy and proteostasis defects prime pancreatic epithelial state changes in KRAS-mediated oncogenesis, Developmental Cell (2025). DOI: 10.1016/j.devcel.2025.07.016. www.cell.com/developmental-cel … 1534-5807(25)00473-3