The human heart beats around 100,000 times a day, sending life-sustaining blood through every corner of the body. Yet, for millions of women, this quiet rhythm is under silent attack. Heart disease has long been considered a “man’s problem,” a condition of older males with chest pain and obvious warning signs. But the reality is far more complex—and alarming. Cardiovascular disease is the number one killer of women worldwide, taking more lives each year than all forms of cancer combined.
What makes this crisis even more heartbreaking is that so much of it is preventable. Women’s heart health often suffers from underrecognition, misdiagnosis, and misconceptions. Too many women believe that cancer is their greatest health risk, while ignoring the subtle, sometimes invisible, signs that their hearts are struggling. Understanding the unique risks women face, and the steps they can take to protect themselves, is not just a matter of medicine—it’s a matter of saving lives, families, and futures.
The Gender Gap in Heart Health
For decades, research and medical practice centered on men’s experiences with heart disease. Clinical trials were male-dominated, diagnostic guidelines were based on men’s symptoms, and treatment strategies often failed to consider women’s biology. This gender gap in research has left women vulnerable, as their symptoms, risk factors, and disease progression can differ significantly.
Women are more likely than men to experience “silent” or atypical symptoms of a heart attack—such as fatigue, shortness of breath, nausea, or pain in the jaw or back—rather than the classic crushing chest pain that men often report. As a result, women may dismiss their symptoms as stress, indigestion, or fatigue, and doctors may misinterpret them, delaying diagnosis and treatment.
Moreover, certain conditions—like autoimmune diseases, pregnancy-related complications, and hormonal changes—play unique roles in women’s cardiovascular health. This means that women’s heart health cannot simply be seen through the same lens as men’s; it requires its own focus, research, and care strategies.
The Science of the Female Heart
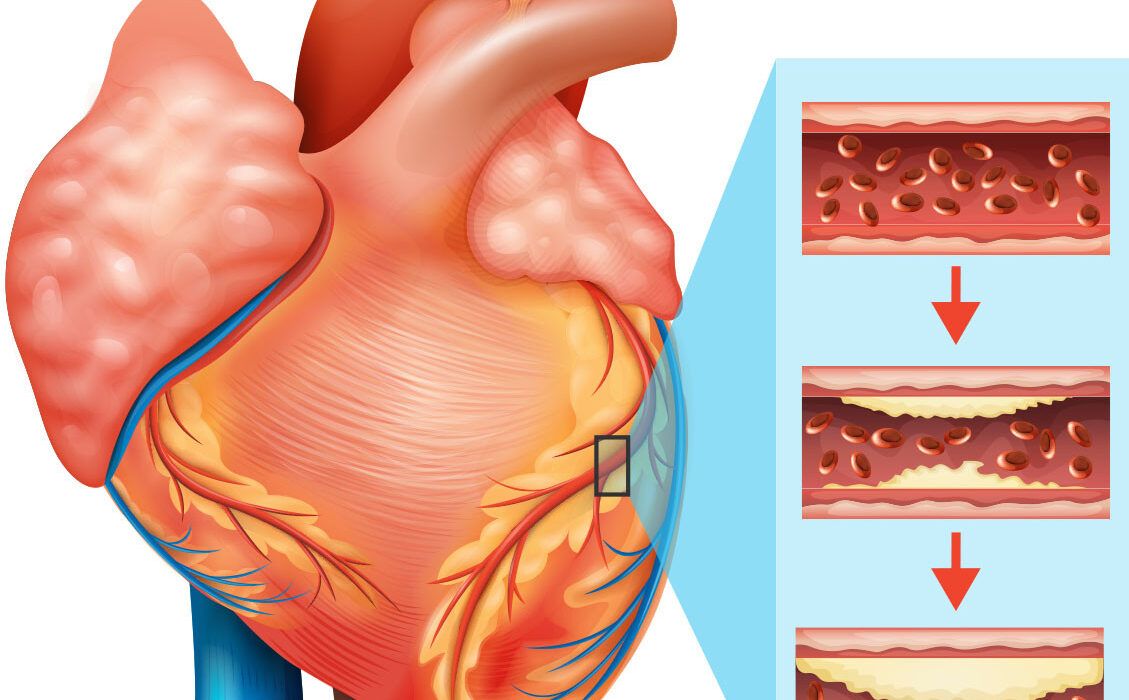
At the biological level, women’s hearts are not identical to men’s. The average woman’s heart is smaller, with finer coronary arteries. This structural difference can make blockages harder to detect on standard imaging tests. Furthermore, women are more likely to experience microvascular disease—where tiny blood vessels are damaged, reducing blood flow—rather than large artery blockages.
Hormones, particularly estrogen, also play a powerful role. During the reproductive years, estrogen offers protective effects by maintaining healthy blood vessel walls, promoting good cholesterol (HDL), and keeping blood pressure in check. But after menopause, when estrogen levels drop, the risk of heart disease rises dramatically. This hormonal shift is one reason why cardiovascular disease becomes the leading cause of death in older women.
Understanding the Risks
Women face many of the same risk factors as men—high blood pressure, high cholesterol, obesity, smoking, diabetes, and inactivity—but their impact can be stronger, more insidious, and sometimes more dangerous in women.
High blood pressure, for instance, is more strongly associated with stroke and heart failure in women than in men. Diabetes also carries a heavier burden, doubling or even tripling women’s risk of heart disease compared to men with the same condition. Smoking is another deadly factor: women who smoke are 25% more likely than men to develop heart disease.
In addition to these shared risks, women encounter unique challenges:
- Pregnancy-related complications such as preeclampsia, gestational diabetes, and preterm birth increase long-term risk of cardiovascular disease. A woman who experiences preeclampsia, for example, has a doubled risk of developing heart disease later in life.
- Autoimmune diseases, including lupus and rheumatoid arthritis, disproportionately affect women and raise inflammation levels, damaging blood vessels.
- Polycystic ovary syndrome (PCOS), a hormonal disorder, is linked with obesity, insulin resistance, and metabolic syndrome—all of which threaten heart health.
- Depression and chronic stress, more prevalent in women, can directly and indirectly harm cardiovascular health by raising stress hormones, disrupting sleep, and influencing lifestyle habits.
These layered risks mean that a woman’s cardiovascular profile is often more complex than a man’s, requiring a nuanced understanding to detect problems early and intervene effectively.
The Hidden Symptoms
One of the greatest dangers in women’s heart health lies in how heart disease manifests. The stereotypical image of a heart attack—a man clutching his chest in agony—does not reflect the reality for many women. Their symptoms are often subtler, easier to dismiss, and sometimes mistaken for anxiety, indigestion, or exhaustion.
Women may experience:
- Shortness of breath
- Nausea or vomiting
- Dizziness or lightheadedness
- Pain or discomfort in the jaw, neck, back, or arms
- Extreme fatigue, sometimes lasting days before an event
These atypical signs mean that women often delay seeking help or are misdiagnosed by healthcare providers. Unfortunately, every minute of delay in recognizing and treating a heart attack can mean the difference between recovery and fatality. Raising awareness of these hidden symptoms is essential not only for women themselves but also for healthcare systems and providers.
The Role of Lifestyle: Choices That Shape the Heart
The heart is both resilient and vulnerable. While genetics and age play roles in cardiovascular health, lifestyle choices are among the most powerful determinants. For women, cultivating heart-healthy habits is an act of empowerment, offering protection not just for the heart but for overall well-being.
Nutrition as Medicine
A diet rich in vegetables, fruits, whole grains, lean proteins, and healthy fats provides the fuel a woman’s heart needs. The Mediterranean diet, which emphasizes olive oil, fish, nuts, legumes, and leafy greens, has been consistently linked with lower risks of heart disease. Reducing processed foods, trans fats, and added sugars helps combat inflammation and obesity, key contributors to heart problems.
Movement for Longevity
Physical activity strengthens the heart muscle, improves circulation, lowers blood pressure, and regulates blood sugar. For women, regular exercise is not just about fitness—it’s a shield against chronic illness. Even moderate activities, such as brisk walking, dancing, or gardening, provide profound benefits when practiced consistently.
Sleep and Stress
Sleep is often overlooked, yet it is a cornerstone of heart health. Women juggling careers, families, and caregiving often sacrifice sleep, which can disrupt hormones, raise blood pressure, and fuel weight gain. Stress, particularly chronic stress, is another hidden enemy. Women under constant pressure may see their bodies flooded with cortisol, a hormone that strains the cardiovascular system. Mindfulness practices, yoga, or even simple breathing exercises can help restore balance.
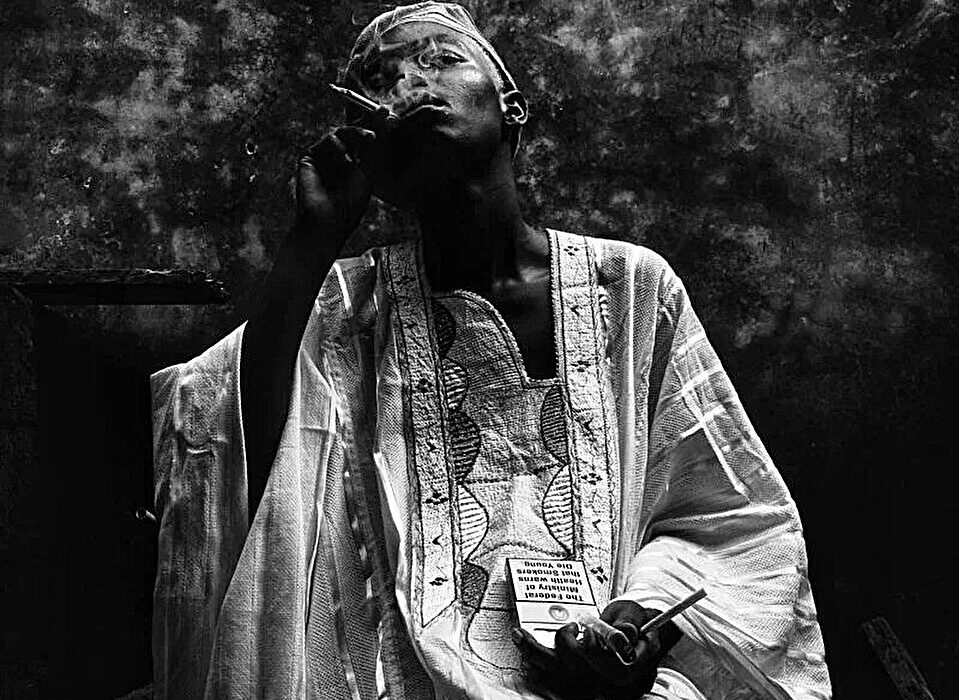
Saying No to Smoking and Excess Alcohol
Smoking is one of the deadliest threats to women’s heart health. Even light smoking dramatically raises risks, and secondhand smoke is harmful too. Alcohol, while sometimes linked with modest protective effects in small amounts, can easily tip into harm when consumed excessively, raising blood pressure and weakening the heart muscle.
Prevention: Building a Shield Around the Heart
Preventing heart disease in women requires both personal commitment and systemic change. On the individual level, prevention means regular check-ups, understanding personal risk factors, and adopting healthy lifestyle habits. Blood pressure, cholesterol, and blood sugar should be monitored regularly, especially after age 40 or during high-risk periods such as post-pregnancy or menopause.
At the community and societal level, prevention requires education, awareness campaigns, and healthcare policies that prioritize women’s heart health. Access to affordable healthcare, maternal care, and preventive screenings must be expanded. Equally important is research dedicated to understanding women-specific cardiovascular patterns, ensuring that treatments and interventions are tailored accordingly.
The Intersection of Mind and Heart
Science is increasingly showing that the heart and mind are inseparable. Mental health profoundly influences cardiovascular health, and vice versa. Depression, anxiety, and trauma are not just emotional struggles—they can alter the nervous system, increase inflammation, and disrupt heart rhythms.
Women, who experience higher rates of depression and anxiety than men, are particularly vulnerable. After a heart attack, women are more likely to develop depression, which can hinder recovery. Conversely, women with untreated depression are more likely to develop cardiovascular disease. Addressing women’s heart health, therefore, demands a holistic approach that includes psychological support alongside medical treatment.
Special Focus: Pregnancy and the Heart
Pregnancy is often described as a stress test for the heart. During pregnancy, blood volume increases by nearly 50%, and the heart must work harder to pump oxygen and nutrients to both mother and child. For most women, the body adapts beautifully. But for some, complications reveal underlying vulnerabilities.
Conditions like gestational diabetes, preeclampsia (dangerously high blood pressure), and preterm birth are not just pregnancy complications—they are red flags for future cardiovascular disease. A woman who has experienced preeclampsia, for example, is at higher risk of developing hypertension, heart disease, and stroke later in life. These risks persist long after childbirth, making postpartum follow-up and long-term monitoring essential.
Menopause and Beyond
The transition to menopause is another pivotal chapter in women’s heart health. As estrogen levels decline, women lose a powerful layer of cardiovascular protection. Cholesterol levels often rise, blood pressure creeps upward, and fat distribution shifts toward the abdomen—all factors that heighten heart disease risk.
This does not mean that heart decline is inevitable. With proactive care—through exercise, diet, stress management, and medical check-ups—women can maintain cardiovascular strength well into older age. Hormone replacement therapy (HRT) has been studied as a potential protective factor, but its role remains complex and should be considered individually with a doctor’s guidance.
The Power of Awareness and Advocacy
Perhaps the most urgent challenge in women’s heart health is awareness. Too few women recognize their risks, and too many dismiss early symptoms. Campaigns such as “Go Red for Women” have made strides in bringing attention to the issue, but stigma and misconceptions persist.
Every woman needs to know: heart disease is not just a man’s disease, and prevention begins early. Talking openly about heart health, encouraging loved ones to seek screenings, and advocating for more inclusive research are powerful ways women can take charge of their cardiovascular destiny.
A Future of Stronger Hearts
The future of women’s heart health lies in the convergence of science, education, and empowerment. Precision medicine, which tailors treatments based on genetics and individual profiles, holds promise for better, more personalized care. Advances in imaging, wearable technology, and AI-driven diagnostics will allow earlier detection and intervention.
But perhaps the most powerful future tool is knowledge itself. When women understand their risks, when healthcare providers listen more closely to their symptoms, and when society invests in prevention, the tide of cardiovascular disease can turn.
Living with Heart: A Final Reflection
At the center of all of this is not just a muscle pumping blood, but the very symbol of life, love, and resilience—the heart. Protecting women’s hearts means protecting their ability to live fully, to nurture families, to lead communities, to create, to love, and to dream.
Heart health is not about fear but about empowerment. It is about recognizing that while risks exist, so does incredible power to prevent, heal, and thrive. Every choice—a nourishing meal, a walk in the fresh air, a good night’s sleep, a moment of calm—becomes a vote for the heart, a promise to keep its rhythm strong.
In the end, women’s heart health is not just a medical issue; it is a human issue. It is about safeguarding the heartbeat of mothers, daughters, sisters, and friends. It is about giving women the chance not only to live longer but to live well, with hearts that are strong enough to carry the weight of life’s challenges and open enough to embrace its joys.