When the body is calm, the heartbeat slows and breathing settles into an easy rhythm. Under strain — a sprint, a deadline, an argument — both quicken in unison. This dance between breath and pulse is not accidental; it is orchestrated by the nervous system. Scientists have long known that heartbeats naturally shift in sync with the breathing cycle, a phenomenon called respiratory heart rate variability, or RespHRV. The greater the coordination, the healthier the heart and the stronger the body’s ability to regulate stress.
Diminished RespHRV is not just a statistic; it is a physical warning. People with chronic heart failure or hypertension often show a loss of this breath–heart synchrony, reflecting strain on the autonomic nervous system — the circuitry that quietly manages life support functions behind the scenes. But although doctors have linked RespHRV to health outcomes for years, the brain-level machinery that connects breathing and heartbeat remained largely mysterious.
That mystery has now begun to crack open.
Oxytocin — Better Known for Warmth — Enters the Picture
In a new study from Aix-Marseille University, neuroscientists working with mice have identified a neural circuit that mechanically links the rhythm of breathing to the timing of heartbeats — and the signal riding that circuit is the hormone oxytocin.
Oxytocin is most famous for its roles in bonding, touch, and emotional closeness. But the new work, published in Nature Neuroscience, shows that it also amplifies the heart–breath synchrony that characterizes states of safety and calm. The researchers tracked how oxytocin-producing neurons fire, how they wire into the brainstem rhythm generator for breathing, and how those signals reach the heart. The result is a biological explanation for why warm emotional states often produce physiologically calm hearts.
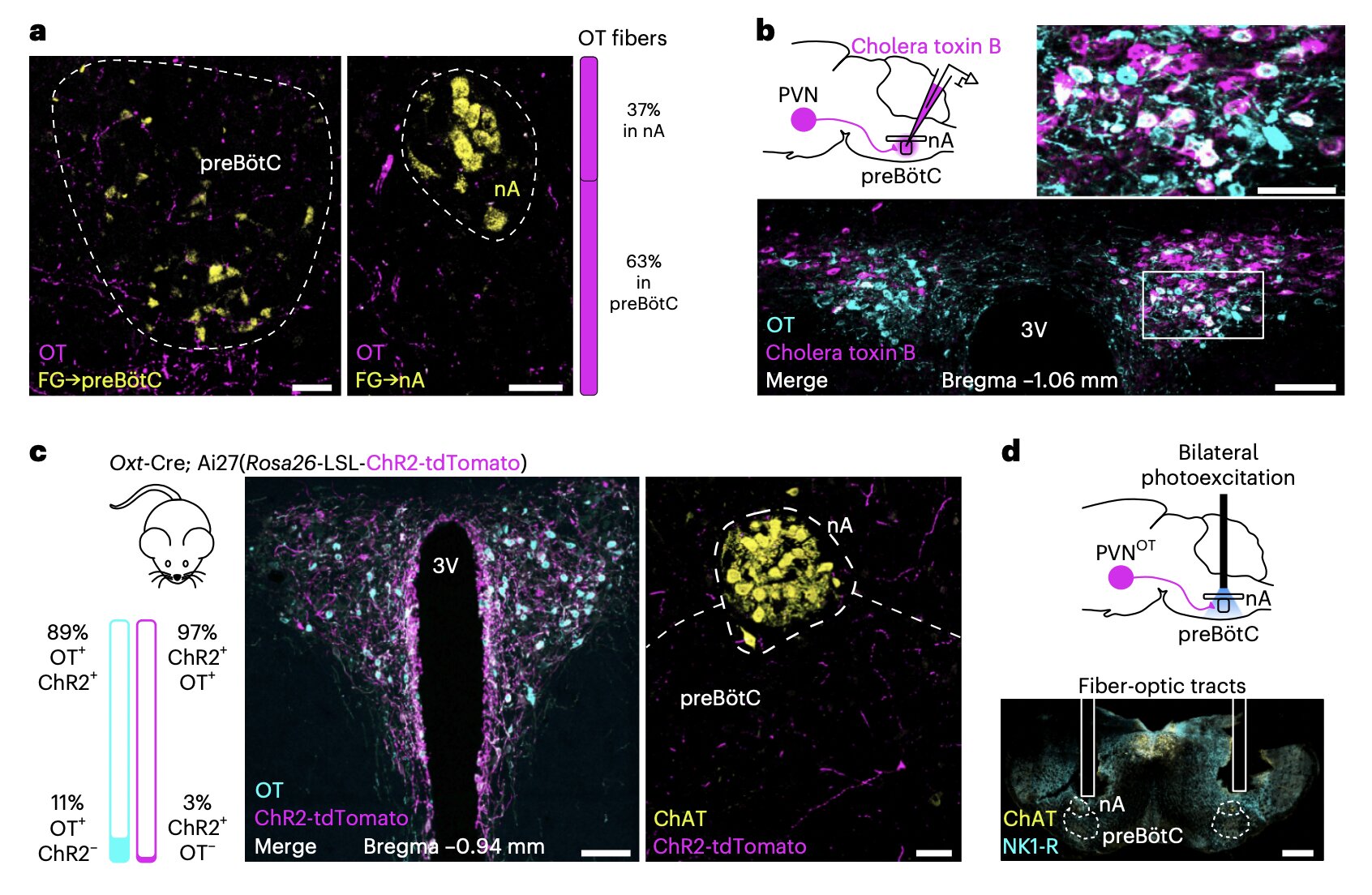
The team found that oxytocin neurons in a specific part of the hypothalamus communicate with inhibitory neurons in the pre-Bötzinger complex — the brainstem structure that generates the rhythm of inhalation. These brainstem neurons, in turn, influence parasympathetic neurons that directly slow the heart. When oxytocin flows through this pathway, the breathing cycle more strongly modulates heart activity, amplifying RespHRV.
The Brainstem as a Switchboard for Calm
To uncover this pathway, the researchers combined sophisticated imaging, physiological monitoring, and targeted manipulation of neural circuits in live mice. They observed how oxytocin-modulated signals sharpened the translation of breath rhythm into heart rhythm, strengthening the coherence between the two.
One key discovery is that oxytocin enhances glycinergic signaling — a form of biological inhibition — from brainstem neurons to the parasympathetic neurons that control the heart. This inhibition intensifies during each inspiration, making the heart more tightly track the respiratory cycle. In effect, oxytocin makes the heart listen more obediently to the breath.
Even more striking, the team found that after stress exposure, this oxytocin-driven pathway helped restore healthy RespHRV during recovery — suggesting that oxytocin is not merely a “feel-good” chemical, but a central regulator that helps shift the body from stress mode back toward physiological peace.
Toward Future Therapies for Stress and Anxiety
The discovery is more than a scientific curiosity. RespHRV is a strong predictor of resilience — people with higher respiratory heart synchronization recover more quickly from emotional shock and are less vulnerable to chronic anxiety. If oxytocin signaling helps resynchronize the heart after stress, then drugs or interventions that boost this pathway may become tools for treating stress-related disorders.
Such tools could range from pharmacological agents that enhance oxytocin signaling in select brain regions to behavioral therapies that naturally trigger oxytocin release — such as slow breathing, touch-based therapies, or pro-social interactions. But before humans can benefit, scientists must confirm that the same pathway exists in people and determine how to manipulate it safely.
Why This Matters
This work provides a mechanistic explanation for something humans have felt but could never anatomically prove: that emotional softness and physiological calm belong to the same network. It bridges sensation and physiology, revealing how safety signals in the brain can ripple down to the heart through a defined neural corridor. The discovery redefines oxytocin not only as a molecule of bonding, but as an internal architect of calm — sculpting our heartbeats into harmony with our breath whenever the body feels safe enough to rest.
The study does not close the story but opens a new front — a concrete path from emotion to organ, from brain to beat. If the findings are confirmed in humans, they could reshape the science of stress recovery and inspire therapies that do not simply blunt symptoms, but coax the body back into the synchrony that marks a state of deep physiological peace.
More information: Julie Buron et al, Oxytocin modulates respiratory heart rate variability through a hypothalamus–brainstem–heart neuronal pathway, Nature Neuroscience (2025). DOI: 10.1038/s41593-025-02074-2.