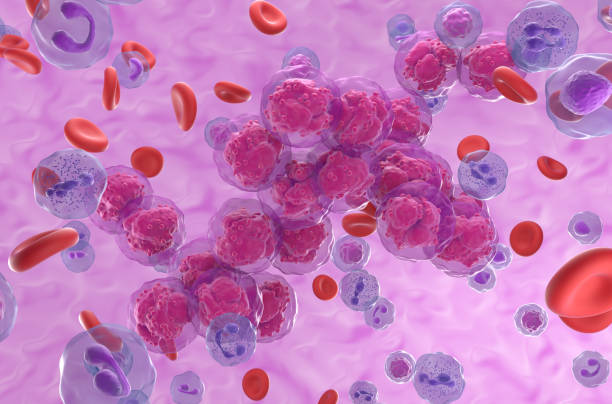
In the intricate battle between cancer and the human immune system, few cancers have been as elusive and devastating as acute myeloid leukemia (AML). Known for its aggressiveness and stubborn resistance to therapy, AML remains one of the most difficult blood cancers to treat. But now, researchers at Lund University in Sweden have uncovered a hidden mechanism that allows AML cells to cloak themselves from the immune system. By developing an antibody to disrupt this mechanism, the team has found a way to reactivate the immune system’s natural ability to recognize and kill leukemia cells.
The findings, published in Nature Cancer, represent a major step forward in the long fight against AML—a disease that takes thousands of lives each year and offers patients limited treatment options.
Why AML is So Difficult to Treat
Acute myeloid leukemia arises from the bone marrow, where blood cells are formed. Unlike some cancers that create isolated tumors, AML floods the bloodstream with malignant cells, making it harder for the immune system and conventional treatments to target them effectively.
Current therapies are notoriously harsh. Patients often endure rounds of intensive chemotherapy or undergo stem cell transplants, both of which carry serious risks and are not always effective. Even with these treatments, the five-year survival rate for AML hovers just above 30%. For decades, researchers have searched for ways to harness the immune system—an approach called immunotherapy—that has revolutionized treatment for other cancers, like melanoma and certain lung cancers. Yet, progress in AML has been frustratingly slow.
This is what makes the discovery from Lund University so compelling. It shines a light on a specific mechanism that AML uses to stay hidden, and, crucially, offers a way to dismantle it.
The Search for a Vulnerability
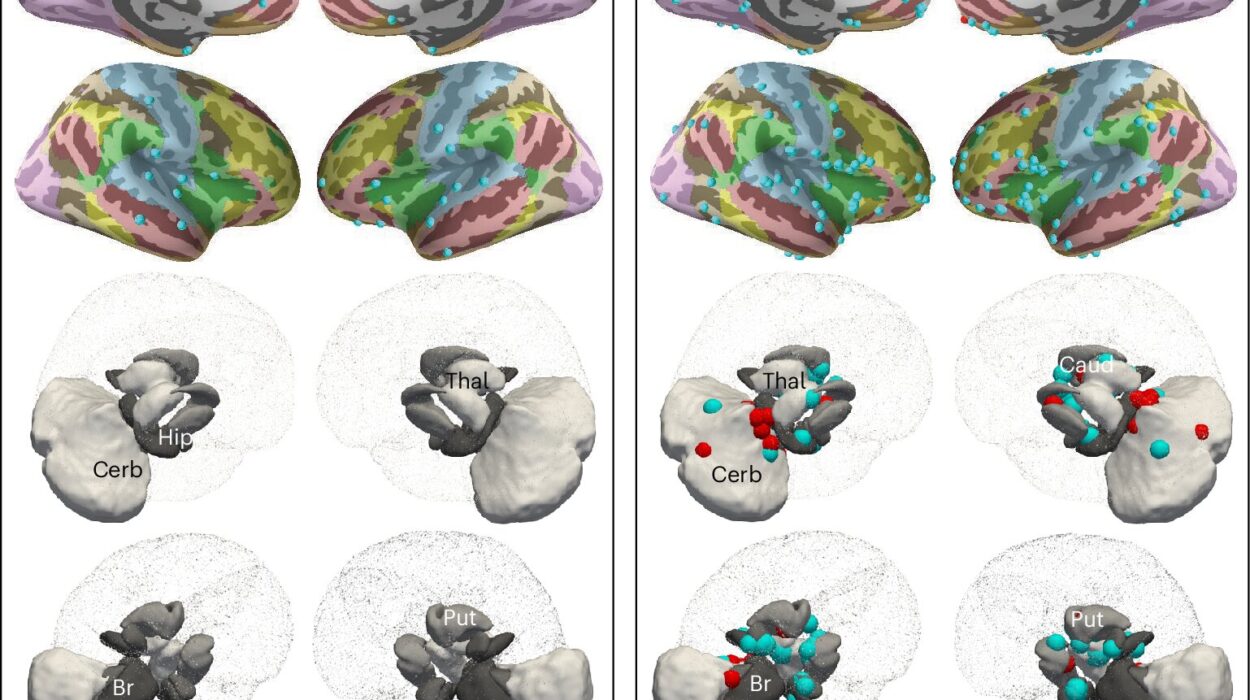
The Swedish research team, led by Professor Thoas Fioretos, began with a simple but ambitious question: could there be proteins on the surface of leukemia stem cells that are absent from healthy blood stem cells? If so, such proteins could serve as precise targets for new therapies, allowing doctors to attack the cancer while sparing the healthy blood system.
To answer this, the researchers undertook an intensive mapping of proteins in bone marrow samples from three patients with particularly treatment-resistant AML. They then compared these profiles with the proteins found on the blood stem cells of healthy individuals.
What they discovered was striking. A previously unknown protein, SLAMF6, appeared consistently on the leukemia cells but not on the healthy stem cells. To confirm this finding, the team analyzed samples from 50 additional AML patients, and the result was the same: SLAMF6 was present only in diseased cells.
Uncovering the Cancer’s Defense Strategy
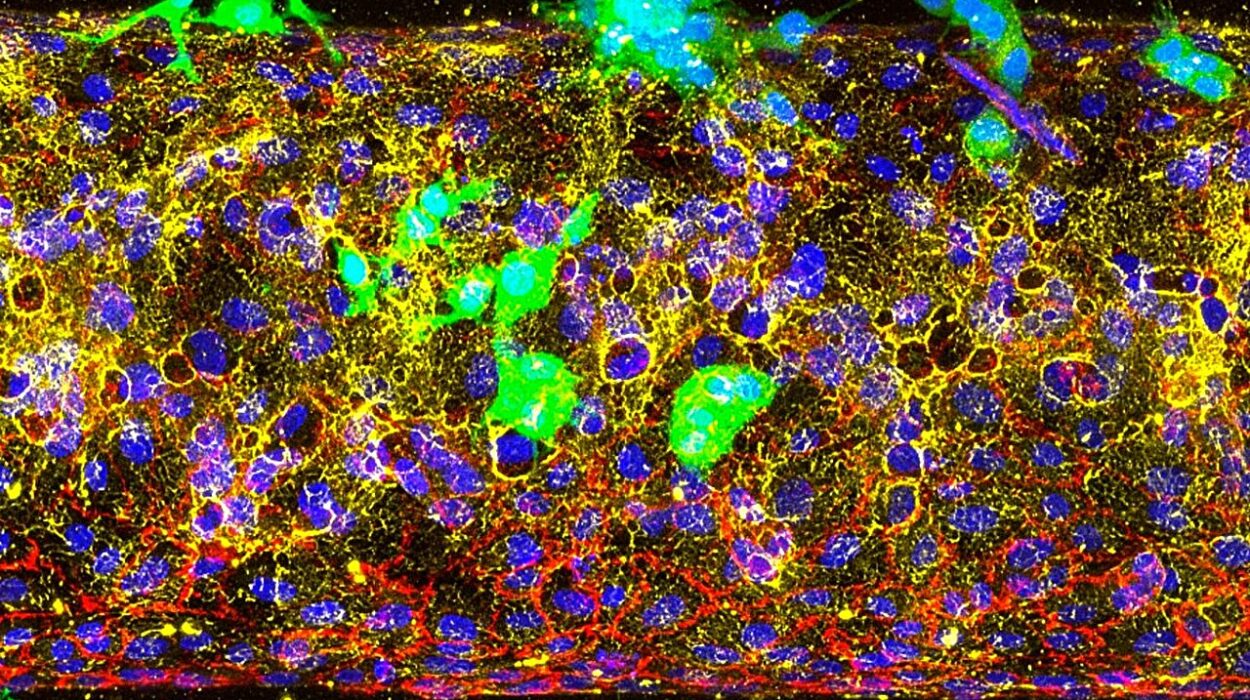
Identifying SLAMF6 was only the first step. The team then needed to understand what role it played in the disease. Using CRISPR/Cas9 gene-editing tools, they studied how altering SLAMF6 affected the leukemia cells. What they found was revelatory: SLAMF6 acted as a shield, preventing the immune system’s T cells from recognizing and attacking the cancer cells.
In other words, the protein was not just a marker of disease—it was an active player in the cancer’s ability to survive. Without intervention, the T cells remained blind, unable to distinguish the malignant invaders from healthy cells.
Turning the Immune System Back On
The real breakthrough came when the researchers developed a specific antibody to block SLAMF6. Once the antibody attached itself to the protein, the shield fell away. Suddenly, the immune system’s T cells could see the leukemia cells clearly—and they attacked.
“It was like turning the switch to the immune system back on,” said Carl Sandén, one of the study’s lead researchers. In laboratory experiments and in trials with mice, the antibody restored the T cells’ ability to destroy AML cells effectively.
The results were dramatic. What had once been an untouchable disease became vulnerable. For the first time, researchers could watch as the immune system, when freed from the cancer’s disguise, fought back with its natural ferocity.
Why This Discovery Matters
This finding helps explain why previous immunotherapies have had limited success against AML. Many therapies that unleash the immune system, such as checkpoint inhibitors, rely on T cells being able to recognize cancer in the first place. If AML uses proteins like SLAMF6 to hide, then these therapies are essentially fighting with blindfolded soldiers. By removing that blindfold, the Lund team has opened a new front in the war against leukemia.
It also marks a shift toward precision medicine in leukemia care. Rather than relying solely on broad, destructive treatments like chemotherapy, scientists are now moving toward therapies tailored to the unique features of each patient’s cancer. If a protein like SLAMF6 is expressed only in diseased cells, then therapies targeting it could strike at the root of the cancer while leaving healthy cells unharmed.
From Lab to Patients
Of course, a discovery in the laboratory does not immediately translate into a treatment available in hospitals. There are years of development, safety testing, and clinical trials ahead. But the researchers are already taking steps in that direction. They have launched a spin-off company, Lead Biologics, to drive the commercial development of the SLAMF6 antibody. The hope is that in the future, this treatment could be offered to patients who desperately need new options.
For now, the discovery offers hope—a rare and precious thing for those facing AML. It suggests that even the most cunning diseases can be outwitted, and that the immune system, when given the right tools, is capable of extraordinary feats.
A Glimpse of the Future
The fight against cancer is never straightforward. Every time scientists make progress, cancer seems to find another way to resist. Yet discoveries like this remind us that science is not static. It evolves, adapts, and pushes forward.
The identification of SLAMF6 is not just a technical achievement—it is a glimpse into the future of medicine. A future where treatments are not blunt instruments but precise keys that unlock the body’s own defenses. A future where patients no longer have to choose between enduring brutal treatments and watching their disease progress.
Acute myeloid leukemia remains a formidable adversary, but the discovery from Lund University shows that its defenses are not impenetrable. With persistence, creativity, and collaboration, the cloak of invisibility that protects cancer cells can be stripped away.
And when that happens, the body’s own immune system—our oldest, most powerful ally—will be ready to finish the fight.
More information: Aberrant expression of SLAMF6 constitutes a targetable immune escape mechanism in acute myeloid leukemia, Nature Cancer (2025). DOI: 10.1038/s43018-025-01054-6