Imagine this: a researcher in a lab, armed with curiosity and a pipette, peers into a microscope and sees something unusual—perhaps a protein behaving in a peculiar way or a compound that stops bacteria in its tracks. It’s a small discovery, seemingly insignificant. But this spark could ignite a multi-billion-dollar journey that spans over a decade and involves thousands of people. This is the beginning of drug development, a fascinating and grueling odyssey that transforms raw scientific insight into life-saving medications found on pharmacy shelves.
We often take for granted the capsules, tablets, and syrups handed to us by pharmacists. What few realize is the sheer complexity and staggering amount of work that lies behind each of them. Drug development is more than mixing chemicals; it’s a meticulous blend of science, strategy, ethics, money, and regulation. It’s a story of triumphs and failures, of perseverance and discovery. To understand how a simple idea becomes a globally distributed medicine, we must travel through the entire pipeline—from the lab bench to the pharmacy counter.
Discovery: The Hunt for Promising Compounds
The journey starts with drug discovery, a phase where researchers identify potential biological targets—proteins, genes, or pathways—that play a crucial role in diseases. Think of this as finding the “villains” in a disease narrative. These targets are typically uncovered through years of basic research, often in university labs funded by government grants.
Once a target is identified, the search begins for a compound—a “hero” molecule—that can interact with it. This search can go in many directions. Scientists might look into nature, screening thousands of plant and microbial extracts. They may turn to libraries of synthetic chemicals, using automated high-throughput screening machines that can test hundreds of thousands of compounds a day. Computational chemistry and artificial intelligence are also playing increasing roles, predicting how molecules will interact with targets without ever mixing chemicals in a test tube.
From millions of candidates, only a handful show promise. These are known as “hits.” Hits are further refined through medicinal chemistry, where scientists tweak their structure to improve potency, reduce side effects, or make them more stable. The goal is to craft the perfect key for the biological lock—the disease target.
At this stage, the compound becomes a “lead.” But before a lead becomes a drug, it must survive an unforgiving gauntlet of testing and validation.
Preclinical Testing: Into the Animal Kingdom
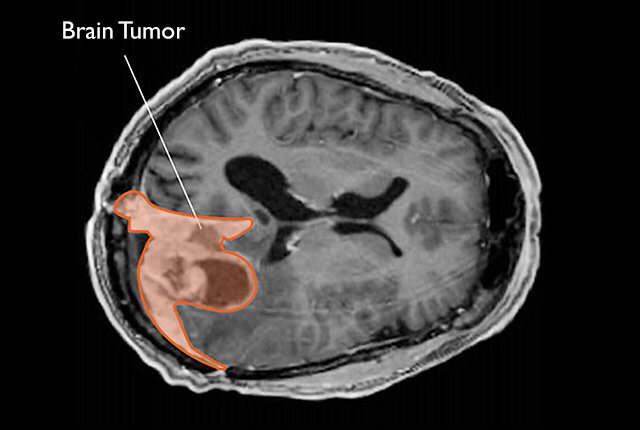
Now the compound must prove its worth in living systems. Enter the preclinical phase, where researchers test the lead compound in laboratory animals, typically mice, rats, and sometimes monkeys or dogs. These studies evaluate how the compound behaves in the body—its pharmacokinetics (what the body does to the drug) and pharmacodynamics (what the drug does to the body). Scientists look at how it is absorbed, distributed, metabolized, and excreted. They also study its mechanism of action: how it actually treats the disease.
Importantly, preclinical testing assesses toxicity. Does the compound cause cancer? Harm unborn fetuses? Damage the liver or kidneys? If even a hint of severe toxicity emerges, the project may be abandoned.
Ethics play a significant role here. Animal studies are conducted under strict regulatory oversight to minimize suffering, and researchers are obligated to use alternatives whenever possible. However, animal testing remains a necessary evil in drug development. It’s the last line of defense before a drug enters human trials.
A successful preclinical candidate is called a “clinical candidate.” But it can only move forward once regulatory agencies like the FDA (in the U.S.), EMA (in Europe), or PMDA (in Japan) grant approval through an Investigational New Drug (IND) application. The IND includes all data gathered so far—pharmacology, toxicology, manufacturing details—and outlines plans for human trials.
Clinical Trials: Testing in Humans
Clinical trials are where science meets the public. These are meticulously designed experiments conducted in human volunteers to test safety, efficacy, and optimal dosing. They are divided into four distinct phases.
Phase I: Safety First
Phase I trials are small, usually involving 20 to 100 healthy volunteers. The aim here is simple but critical: assess the drug’s safety in humans. Researchers look for side effects, monitor vital signs, and gather preliminary data on how the drug is processed by the human body.
Because this is the first time the drug enters human systems, it’s risky. Some compounds that looked safe in animals turn out to have dangerous side effects in people. A drug that fails here rarely gets a second chance.
Phase II: Testing for Effectiveness
If Phase I is successful, the drug moves to Phase II, which involves several hundred patients who actually have the condition the drug is meant to treat. This phase tests efficacy—does the drug actually work?—as well as safety. Researchers also experiment with different doses to find the right balance between effectiveness and tolerability.
Phase II is where many drugs stumble. Sometimes the drug doesn’t work as expected in humans. Sometimes side effects emerge that weren’t seen in animals or healthy volunteers. It’s an expensive, high-stakes filter that weeds out unfit candidates.
Phase III: Large-Scale Validation
Drugs that make it past Phase II move into the critical Phase III trials. These involve thousands of patients across multiple hospitals, sometimes in different countries. This phase provides definitive evidence about the drug’s safety and effectiveness and compares it against existing treatments or placebos.
Because Phase III is so large and expensive, it’s typically sponsored by pharmaceutical companies rather than academic researchers. The data gathered here will be used to apply for regulatory approval.
The stakes couldn’t be higher. Each Phase III trial can cost hundreds of millions of dollars. A failure here is devastating financially and emotionally. Yet it’s also the most critical phase—many of the drugs we rely on today exist because they survived this ultimate test.
Phase IV: After Approval
Even after a drug is approved and hits the market, the journey isn’t over. Phase IV trials, or post-marketing surveillance, continue to monitor the drug in real-world settings. Rare side effects, drug interactions, or long-term consequences often don’t appear until the drug is used by large, diverse populations.
Regulatory bodies can pull a drug off the market or require warning labels if serious problems emerge during this phase. Thalidomide, Vioxx, and several other infamous cases show why post-approval vigilance is vital.
Regulatory Approval: Passing the Gatekeepers
Once a drug passes Phase III, its developers submit a New Drug Application (NDA) to the relevant regulatory agency. The NDA includes all data from discovery, preclinical, and clinical phases, manufacturing processes, labeling plans, and proposed usage guidelines.
Regulators comb through this mountain of data with rigorous scrutiny. Their job is to protect public health, ensuring the drug is both safe and effective. They may convene advisory committees, hold public hearings, or request additional studies.
Approval can take months or even years. But if the data is solid and the benefits outweigh the risks, the drug receives the green light. It’s a moment of celebration for scientists, investors, and—most importantly—patients.
Manufacturing: Scaling Up for the World
Now comes a new challenge: manufacturing the drug at scale. Making a few grams in the lab is one thing; producing tons for global distribution is quite another. The compound must be synthesized, purified, and formulated into tablets, capsules, injections, or topical forms.
Manufacturing must follow Good Manufacturing Practices (GMP), a set of stringent guidelines that ensure consistency, quality, and safety. Every batch is tested for purity, potency, and contamination. A single error could lead to recalls, lawsuits, or worse—patient harm.
Supply chains must be robust, efficient, and resilient. Ingredients might come from one continent, be synthesized in another, and packaged in yet another. Cold storage, transportation, and inventory management all become critical.
Marketing and Market Access: Reaching the Right Patients
With manufacturing underway, pharmaceutical companies turn their attention to market access and education. They work with doctors, hospitals, insurance companies, and government agencies to ensure the drug reaches those who need it.
Pricing is a controversial and complex issue. Companies argue that high prices reflect the enormous cost and risk of drug development. Critics counter that prices are often unaffordable, especially in countries without universal healthcare. Balancing profit and accessibility remains a central ethical debate in modern medicine.
Marketing efforts must follow strict regulations. Companies can’t make unsubstantiated claims or promote off-label uses. Educational campaigns, physician training, and patient advocacy all play a role in ensuring the drug is used correctly and ethically.
The Role of Innovation and Technology
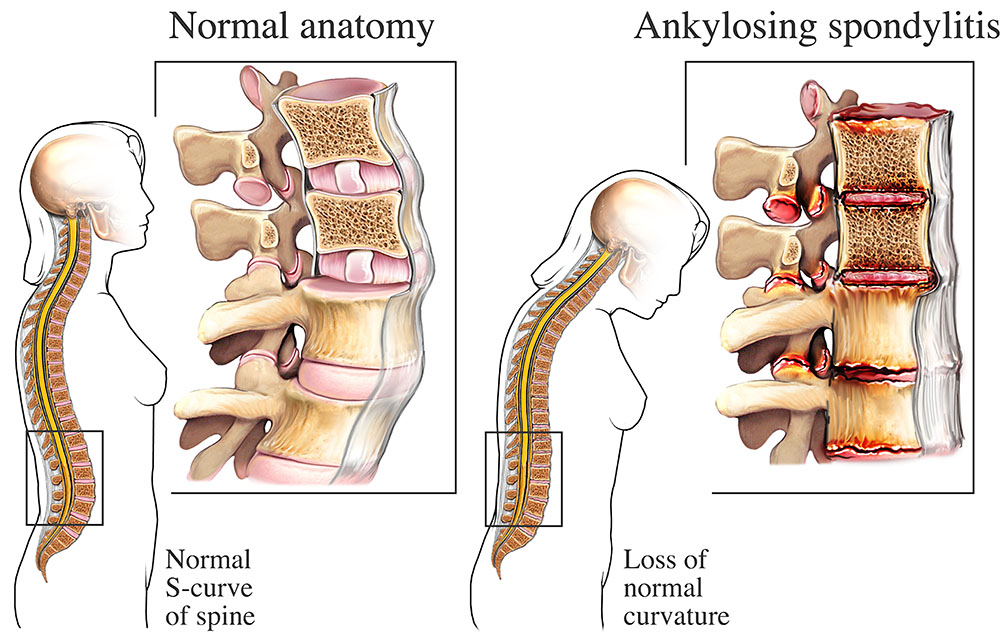
The world of drug development is changing rapidly. Artificial intelligence is being used to predict molecular behavior and design better compounds. Genomics is helping create personalized medicine tailored to a person’s genetic profile. mRNA technology, as seen in COVID-19 vaccines, is opening new frontiers in infectious disease and cancer treatment.
3D printing may soon allow customized pills with multiple drugs and time-release mechanisms. CRISPR and gene editing are leading to therapies that treat the root cause of genetic diseases. The integration of data science, bioengineering, and machine learning is transforming what’s possible.
These innovations promise to make drug development faster, cheaper, and more targeted. But they also bring new challenges: regulatory uncertainty, ethical dilemmas, and questions about long-term safety.
The Human Cost: Failures, Setbacks, and Sacrifice
For every drug that succeeds, thousands fail. Many fail in preclinical stages, never making it to humans. Others crash during clinical trials. Some show promise but are shelved due to strategic or financial reasons.
Each failure represents years of effort, lost money, and disappointed hopes. Yet failure is an essential part of the process. Every dead end teaches scientists more about biology and chemistry, informing future efforts.
The emotional toll is real. Researchers invest their lives in these compounds. Patients enroll in trials hoping for miracles. Families hold their breath. The stakes are always deeply human.
Conclusion: From Molecule to Miracle
The journey from lab to pharmacy is long, complex, and fraught with challenges. But it is also one of the most extraordinary achievements of modern science. Each pill on the shelf represents a triumph of human ingenuity, collaboration, and resilience.
Drug development isn’t just about chemistry—it’s about saving lives, alleviating suffering, and advancing the boundaries of what’s possible. It’s about the fusion of science, ethics, and humanity in pursuit of a better world.
The next time you swallow a pill or apply a cream, take a moment to reflect on the incredible odyssey it has traveled. From a flash of insight in a lab to a regulated, mass-produced medicine in your hands, it embodies decades of knowledge, billions of dollars, and countless hours of work.
This is drug development—not just a scientific process, but a profoundly human one.