It happens to roughly half of the world’s population, every month, from adolescence to middle age. Yet for centuries, menstruation has lived in the shadows—talked about in whispers, shrouded in shame, and treated as if it were something unclean or inconvenient rather than what it truly is: a biological marvel. Menstruation is more than just a monthly bleed; it’s a vital sign, a barometer of hormonal health, and a messenger that speaks volumes about what’s going on inside the female body.
So what, exactly, is “normal” when it comes to menstrual health? That question might seem simple, but the answer is as varied and personal as the people who menstruate. From the duration of your cycle to the color of your blood, from cramps that knock you off your feet to the barely noticeable twinges of ovulation—understanding menstrual health requires us to break free from stigma and listen closely to what our bodies are trying to say.
The Menstrual Cycle: A Symphony of Hormones
To understand what’s normal and what’s not, we first have to understand the menstrual cycle itself—not just the bleeding part, but the whole hormonal symphony that takes place each month. It’s not simply a countdown to the next period; it’s an orchestrated cycle of events that prepares the body for a potential pregnancy, even if pregnancy never happens.
The average menstrual cycle is about 28 days, but anything from 21 to 35 days can still be considered within the normal range. Day 1 is the first day of menstruation. This is when the uterine lining, or endometrium, is shed because pregnancy did not occur. Estrogen is low, and you may feel tired, crampy, or emotionally raw.
After the period, the follicular phase begins. This is when your body starts gearing up again. Estrogen levels rise, a dominant follicle matures in the ovaries, and your energy levels may increase. Around the midpoint—usually Day 14 in a 28-day cycle—ovulation occurs. A mature egg is released, triggered by a surge in luteinizing hormone (LH). This is the time of peak fertility.
Following ovulation, the luteal phase kicks in. Progesterone rises, preparing the uterine lining to support a fertilized egg. If no pregnancy occurs, hormone levels crash, and the cycle starts anew with your next period.
Every hormone shift during this process can affect your mood, energy, skin, libido, digestion, and sleep. That’s why it’s not “just a period”—it’s a full-body experience, every month.
What a “Normal” Period Looks Like
It’s tempting to wish there were a universal standard for periods—a neat definition of “normal” that everyone could follow. But the truth is, periods are as individual as fingerprints. Still, medical science does give us some general parameters.
A normal period typically lasts between 3 and 7 days, with bleeding ranging from light to moderately heavy. Blood color can vary from bright red to dark brown. Small clots may appear, especially on heavier days, and mild to moderate cramps are common due to the uterus contracting to shed its lining.
It’s also normal for your cycle to vary a bit from month to month, especially if you’re under stress, traveling, sick, or have recently changed your diet or sleep routine. Hormonal fluctuations are sensitive to all these factors, and the menstrual cycle often acts like a canary in the coal mine, warning you when something is off.
The First Period and What to Expect
Menarche—the first menstrual period—usually happens between the ages of 10 and 15, although some girls may start earlier or later. In the months leading up to it, there might be signs: breast development, pubic hair, and white or clear vaginal discharge. The first period is often light and irregular, and it may take a few years for cycles to stabilize.
It’s essential to normalize this phase for young menstruators. Open conversations about what to expect, how to manage bleeding, and how to recognize signs of pain or irregularity can turn a potentially confusing experience into one of empowerment.
Cramps, Clots, and Crankiness: When Is It Too Much?
Cramps—technically called dysmenorrhea—are so common that many people just accept them as a painful part of life. But while some cramping is normal, pain that interferes with daily functioning is not. If you find yourself doubled over, missing school or work, or relying on strong painkillers every month, that’s a red flag.
Heavy bleeding—clinically termed menorrhagia—is another warning sign. If you’re soaking through pads or tampons in less than two hours, passing large clots, or bleeding longer than seven days, it’s time to see a healthcare provider. These symptoms could indicate fibroids, polyps, endometriosis, adenomyosis, or a bleeding disorder.
Emotional symptoms can also signal an imbalance. While many experience mood swings or irritability in the days leading up to their period (thanks to fluctuating progesterone and estrogen), severe depression, anxiety, or rage may indicate premenstrual dysphoric disorder (PMDD), a more intense form of PMS that affects about 5-10% of menstruators.
Irregular Cycles: What’s Causing the Chaos?
A few irregular periods here and there aren’t usually cause for concern. However, consistently irregular cycles—especially cycles that are shorter than 21 days or longer than 35—may suggest an underlying issue. Polycystic Ovary Syndrome (PCOS) is one of the most common culprits. It’s a hormonal disorder characterized by irregular ovulation, excess androgen (male hormone) levels, and sometimes cysts on the ovaries.
Other causes of irregularity include thyroid disorders, excessive exercise, eating disorders, chronic stress, and perimenopause. Skipped periods—especially in people who are not pregnant or using hormonal birth control—shouldn’t be ignored.
Spotting and Mid-Cycle Bleeding: Whisper or Warning?
Light spotting between periods can occur for benign reasons—like ovulation, starting a new birth control method, or hormonal fluctuations. However, persistent or heavy mid-cycle bleeding can be a sign of cervical polyps, endometrial hyperplasia, or even cancer. It can also signal an infection or injury.
If you notice bleeding after sex or random spotting that doesn’t follow a pattern, it’s best to get it checked out. Bleeding should follow a rhythm, and anything outside that rhythm deserves a closer look.
Birth Control, Periods, and the Myth of “Regulation”
Hormonal birth control is often prescribed to “regulate” periods, but what it actually does is suppress ovulation and induce a withdrawal bleed—not a true period. This can be a helpful tool for managing painful or heavy cycles, acne, or endometriosis, but it’s important to understand that the bleed on the pill isn’t a natural menstrual cycle. That doesn’t mean it’s bad—just different.
Some methods, like the hormonal IUD or the implant, may stop bleeding altogether. This is medically safe for most people, but it can be unsettling if you’ve been taught that monthly bleeding is essential for health. In reality, having a period isn’t necessary when ovulation is being suppressed, unless you’re using the cycle to track fertility or diagnose underlying issues.
Endometriosis: The Hidden Disease
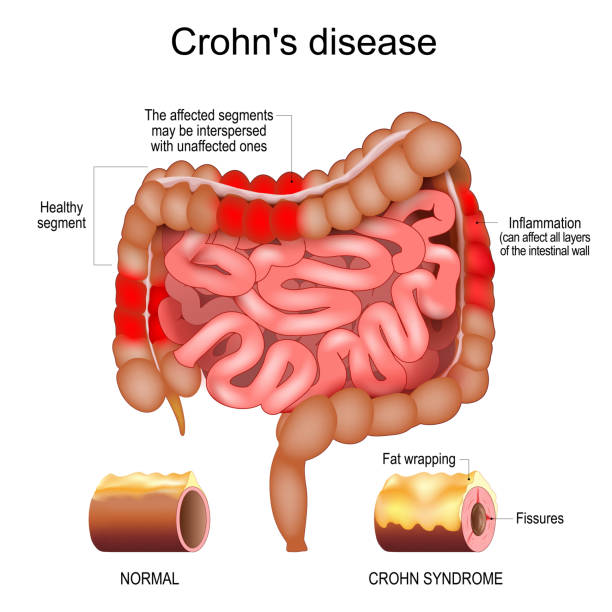
For too long, people with endometriosis have suffered in silence, often dismissed as having “bad cramps” or being overly sensitive. But endometriosis is a serious, often debilitating condition in which tissue similar to the uterine lining grows outside the uterus—on ovaries, fallopian tubes, the bladder, or even the intestines.
This rogue tissue behaves like endometrial tissue: it thickens, breaks down, and bleeds each cycle. But because it has no way to exit the body, it causes inflammation, scarring, and intense pain. Many endure years of misdiagnosis before receiving appropriate care. There is no cure, but surgery, hormonal treatments, and pain management can improve quality of life.
PCOS: More Than Missed Periods
Polycystic Ovary Syndrome is not just about cysts—it’s a complex endocrine disorder with far-reaching effects. PCOS affects up to 1 in 10 people with ovaries and is a leading cause of infertility. It’s characterized by irregular periods, high androgen levels (which can cause acne, facial hair, and hair thinning), insulin resistance, and metabolic complications.
Diagnosis typically requires two of the following: irregular ovulation, excess androgens, and polycystic ovaries on ultrasound. But treatment is highly individualized. Managing PCOS often involves lifestyle changes, hormonal therapies, and sometimes medications to address insulin sensitivity.
Menstrual Hygiene: Access, Equity, and Education
Menstrual health isn’t just a medical issue—it’s a social justice issue. Across the globe, millions of people lack access to safe, affordable menstrual products. Some miss school or work due to period poverty. In some cultures, menstruators are isolated, shamed, or denied basic participation in daily life.
Education is also critical. Many grow up without adequate knowledge about their own bodies. Shame and misinformation breed silence, and silence keeps menstrual health in the dark. Promoting menstrual literacy is not only empowering—it’s essential for global health and gender equality.
Perimenopause and the Slow Fade to Silence
Menstrual cycles don’t stop all at once. Perimenopause—the transition to menopause—can last anywhere from 2 to 10 years, often beginning in the early 40s. During this time, periods become unpredictable. They may be heavier, lighter, closer together, or farther apart. You may experience hot flashes, night sweats, mood swings, vaginal dryness, and sleep disturbances.
Eventually, menopause is reached when 12 consecutive months have passed without a period. After that, menstruation becomes a memory, but the hormonal echoes may linger. Bone density, heart health, and sexual wellness all become key concerns in the post-menopausal years.
Tracking Your Cycle: A Practice in Self-Knowledge
One of the most powerful tools in menstrual health is cycle tracking. Whether you use a paper journal or a smartphone app, charting your cycle helps you understand your unique rhythm and detect any changes early.
Track not just bleeding, but also symptoms like cramps, mood, discharge, libido, sleep, and energy levels. Over time, you’ll start to see patterns—and when something falls out of that pattern, you’ll notice it. That’s the foundation of body literacy, and it’s an act of radical self-care.
When to See a Doctor
If your period is painful, irregular, unusually heavy, or missing, it’s time to seek medical guidance. You don’t need to suffer in silence. Modern medicine offers a wide range of diagnostic tools—blood tests, pelvic ultrasounds, hormone panels—and treatments tailored to your unique needs.
Listen to your body. Pain is not a virtue. Bleeding is not an inconvenience. Your menstrual cycle is a message. Learn its language.