Multiple sclerosis (MS) has long baffled scientists and doctors. It is a disease where the body’s own immune system turns against the brain and spinal cord, stripping away the protective coating around nerve fibers — a process that disrupts communication between the brain and the body. For many people, MS begins with relapses and remissions, moments of decline followed by temporary recovery. But over time, the disease can shift into a more relentless form known as progressive MS — a phase marked by steady, irreversible neurological decline and very few treatment options.
Now, in a groundbreaking discovery, scientists have uncovered a previously unknown type of brain cell that appears to play a major role in driving the progression of this devastating condition. The finding, published in Neuron, offers not only a new perspective on what fuels MS but also a promising target for future therapies.
Modeling the Disease in a Dish
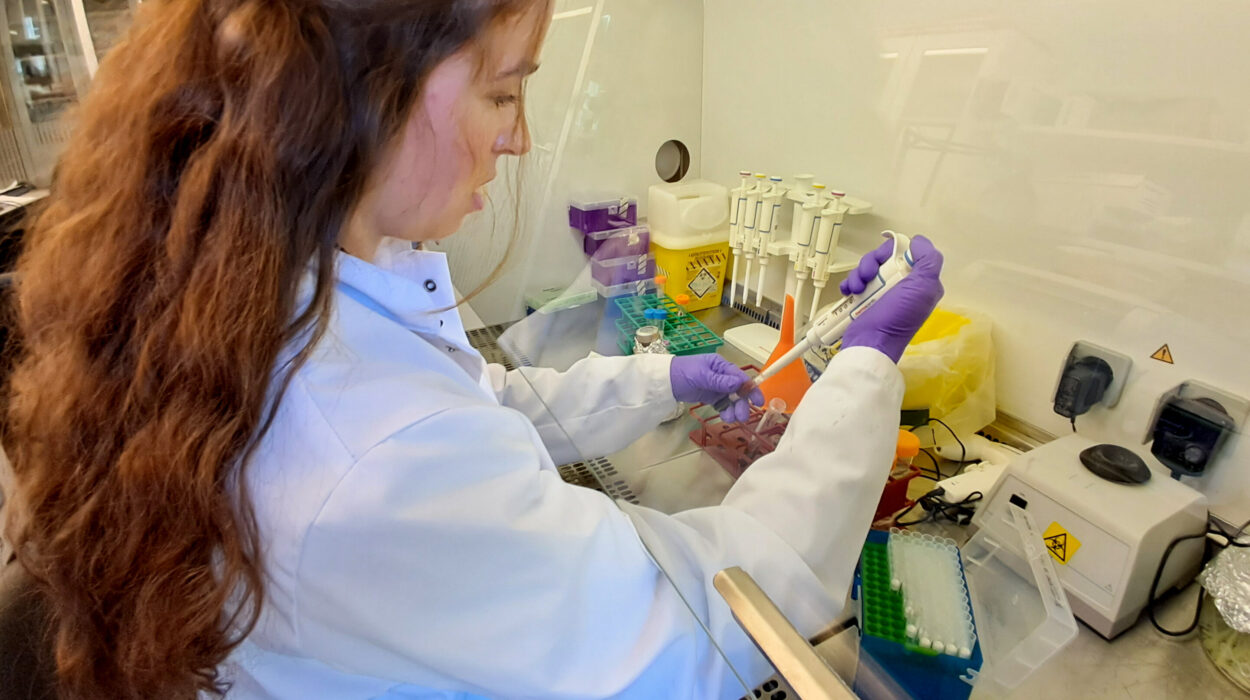
To investigate what happens deep inside the brains of people with progressive MS, researchers from the University of Cambridge in the UK and the National Institute on Aging in the US turned to an innovative “disease-in-a-dish” model. They began by taking skin cells from patients with progressive MS and reprogramming them into induced neural stem cells — immature cells capable of dividing and transforming into different types of brain cells.
This process allowed scientists to recreate aspects of the disease outside the human body, in a controlled environment where every step could be observed. What they found was astonishing: among these cells, a subset began reverting to a much earlier stage of development, transforming into an unusual kind of cell known as radial glia-like (RG-like) cells.
These cells weren’t random anomalies. They appeared about six times more often in samples taken from people with progressive MS than in healthy controls. Because of their unique features and association with disease, researchers named them disease-associated radial glia-like cells — or DARGs.
The Return of the Radial Glia
Radial glia are essential during early brain development. They serve as scaffolding that guides young neurons to their proper locations and can transform into other types of brain cells. In a developing brain, these cells are the architects — designing, supporting, and building the neural network.
But in adults, radial glia are almost entirely gone. Their sudden reappearance in MS patients, therefore, raises profound questions. Why would mature brain cells regress to a more primitive state? And what impact would that have on brain function?
The researchers found that these DARGs were not just harmless remnants of early development. Instead, they seemed to behave abnormally, showing a troubling combination of traits: they were both “young” and “old” at the same time. While they reverted to an immature developmental stage, they also displayed hallmarks of cellular aging, or senescence — a state in which cells stop dividing but remain metabolically active, often releasing inflammatory molecules that damage surrounding tissues.
This paradoxical state made DARGs particularly dangerous. They acted like rogue players in the brain’s ecosystem — instead of supporting neurons, they secreted toxic signals that accelerated aging and inflammation in neighboring cells.
The Inflammatory Signal of Damage
One of the most striking features of DARGs is their heightened sensitivity to interferons — molecules that serve as “alarm signals” for the immune system. In healthy brains, interferons help coordinate defense responses. But in DARGs, this signaling system goes into overdrive.
Their genetic and epigenetic profiles — the patterns of chemical marks that regulate which genes are turned on or off — revealed that these cells are primed to respond excessively to immune activation. That overreaction may be one of the driving forces behind the chronic inflammation seen in progressive MS.
Professor Stefano Pluchino from the University of Cambridge, one of the senior authors of the study, described it vividly: “Progressive MS is a truly devastating condition, and effective treatments remain elusive. What we’ve discovered are glial cells that don’t just malfunction — they actively spread damage. They release inflammatory signals that push nearby brain cells to age prematurely, fueling a toxic environment that accelerates neurodegeneration.”
In other words, DARGs might not simply be bystanders caught in the chaos of MS — they could be its key instigators.
Confirming the Culprits
To ensure that these findings weren’t just a laboratory artifact, the researchers compared their results with human brain tissue from people who had died with progressive MS. Using advanced single-cell RNA sequencing and spatial mapping — techniques that reveal how genes are expressed within individual cells and where those cells are located in the brain — they found that DARGs were not evenly distributed.
Instead, they clustered within chronically active lesions — regions of the brain that show persistent inflammation and tissue damage. These are precisely the areas that worsen over time and contribute to progressive disability.
Even more telling, DARGs were found near immune cells known for promoting inflammation, suggesting that they actively interact with and possibly amplify the body’s immune assault on the nervous system.
A New Target for Treatment
This discovery opens a new frontier in MS research. For decades, scientists have focused on the immune system as the primary culprit behind MS. While that remains true, the identification of DARGs shifts part of the attention back to the brain itself — to the cells that live there and may perpetuate inflammation long after the immune system’s initial attack.
By isolating and studying DARGs in the lab, scientists can now explore how these cells communicate with neurons, microglia, and other cell types in the brain. Understanding that cellular “conversation” could reveal the molecular triggers that push DARGs into their harmful state — and, crucially, how to silence them.
Dr. Alexandra Nicaise, co-lead author of the study, explained, “We’re now working to explore the molecular machinery behind DARGs, and test potential treatments. Our goal is to develop therapies that either correct DARG dysfunction or eliminate them entirely. If we’re successful, this could lead to the first truly disease-modifying therapies for progressive MS, offering hope to thousands living with this debilitating condition.”
The Broader Implications
Intriguingly, this isn’t the first time radial glia-like cells have been spotted in human disease. Similar cells have been detected in glioblastoma — one of the most aggressive forms of brain cancer — and in cerebral cavernomas, clusters of abnormal blood vessels in the brain. Until now, these sightings were rare, partly because scientists lacked the technology to detect them with precision.
Now, with advanced stem cell models and single-cell sequencing techniques, researchers can look more closely than ever before. Professor Pluchino and his colleagues believe that DARGs might turn out to be key players not just in MS, but in many forms of neurodegeneration — from Alzheimer’s to Parkinson’s disease.
If that’s true, these cells could represent a unifying thread in our understanding of how the brain breaks down over time — and a powerful new target for treatments across multiple conditions.
Hope on the Horizon
Progressive multiple sclerosis has long been one of medicine’s most daunting challenges. While there are several treatments for the relapsing-remitting form of MS, few options exist once the disease enters its progressive stage. For patients, this often means watching their mobility, independence, and cognitive function gradually decline, with little that medicine can do to stop it.
The discovery of DARGs does not yet offer an immediate cure — but it provides something equally important: a direction. It gives scientists a new way to think about the disease, a tangible set of cells to study, and a potential biological target to aim at.
In the complex landscape of the human brain, progress often comes from small, hidden clues — a rare cell type, a faint genetic signal, a forgotten pathway that reveals itself under the microscope. DARGs may be one of those clues: small in number but enormous in significance.
For patients and researchers alike, this discovery rekindles a vital spark of optimism — the belief that even in the most stubborn diseases, there is always more to learn, and always another door to open.
More information: Integrated Omics Reveals Disease-Associated Radial Glia-like Cells with Epigenetically Dysregulated Interferon Response in Multiple Sclerosis, Neuron (2025). DOI: 10.1016/j.neuron.2025.09.022. www.cell.com/neuron/fulltext/S0896-6273(25)00710-X