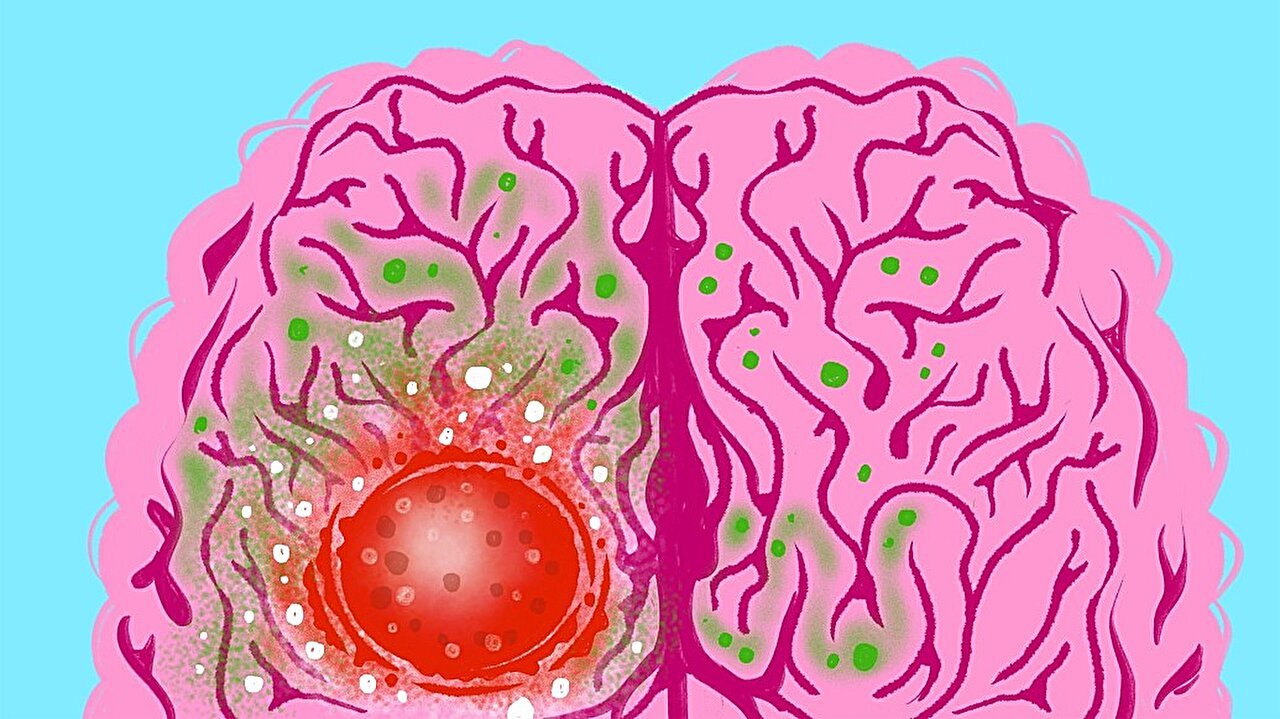
Glioblastoma is often described as the most aggressive and unforgiving of brain cancers. For the patients who receive this diagnosis, the news is devastating: the average life expectancy is only one to two years, even with the best available treatments. Surgeons can remove as much of the tumor as possible, radiation and chemotherapy can strike at what remains, but almost inevitably, the cancer returns—stronger, more resistant, more determined.
What makes glioblastoma so deadly is not just its rapid growth but its ability to invade the brain’s delicate tissue with ruthless precision. Normal brain cells that once functioned harmoniously begin to change, becoming predators within their own home. These cancerous cells are not only structurally different from their healthy neighbors—they are metabolically different, too. They consume nutrients in unique ways, fueling their unchecked growth. Understanding this hidden metabolic shift has become one of the greatest challenges in modern cancer research.
Following the Sugar Trail
A recent study published in Nature by researchers at the University of Michigan has illuminated this dark territory. The team, combining expertise from the Rogel Cancer Center, the Department of Neurosurgery, and the Department of Biomedical Engineering, asked a deceptively simple question: how do glioblastoma cells use sugar compared to healthy brain cells?
To answer this, they used a powerful technique—injecting small amounts of labeled sugar into both mice and patients with glioblastoma. By tracing the sugar’s path, the researchers could follow the invisible highways of metabolism, watching in real time as the molecules were processed within the brain.
The results were striking. Both healthy brain tissue and tumor cells consumed sugar hungrily, but they used it for entirely different ends. The normal brain converted sugar into energy and neurotransmitters—molecules essential for thought, memory, and survival. Tumors, however, made a different choice at this metabolic fork in the road. Instead of fueling brain function, glioblastomas redirected sugar into building blocks of growth: nucleotides for DNA and RNA, the very materials needed to divide and spread.
As Andrew Scott, Ph.D., a scholar in the lab, explained, “It’s a metabolic fork in the road.” And glioblastomas, it seems, always take the path that leads to more cancer.
Metabolism as a Weapon
Metabolism is life’s engine. Every breath we take, every bite of food we eat, is broken down into molecular fuel that powers cells. But in cancer, this universal process is hijacked. Tumor cells, like cunning thieves, rewire their metabolic systems to prioritize survival and expansion over cooperation with the body.
In glioblastoma, this theft becomes especially sinister. While the healthy brain uses sugar to create amino acids—the raw materials for proteins—the tumors abandon this route. Instead, they scavenge amino acids from the blood, sucking them in from the body’s resources to sustain their growth. This discovery gave the researchers a daring idea: what if the supply of these amino acids could be cut off?
Starving the Enemy
The team focused on two amino acids in particular: serine and glycine. These molecules, usually produced and recycled in the healthy brain, were being hoarded by glioblastoma cells. By removing them from the diet of mice with brain tumors, the researchers tested whether the cancer’s hunger could be turned against it.
The results were remarkable. Mice fed an amino acid–restricted diet responded better to radiation and chemotherapy. Their tumors grew more slowly, and in some cases, the cancers shrank compared to those in mice that had normal diets.
“It was like dropping a roadblock on a busy freeway,” said Costas Lyssiotis, Ph.D., one of the study’s senior authors. In healthy brain cells, amino acid uptake is like a quiet country road, with little traffic. But in cancer cells, it is a highway filled with speeding cars. Blocking the road where traffic is heaviest causes maximum disruption with minimal harm to normal tissue.
From Laboratory to Clinic
This discovery is more than a scientific curiosity—it is a glimpse of a new treatment strategy. Current therapies for glioblastoma almost always fail because the tumors adapt. They learn to resist radiation and chemotherapy by rewiring their metabolism. But if diet itself could become part of the treatment—limiting the nutrients tumors need most—patients might finally have an advantage.
The University of Michigan team is now preparing clinical trials to test whether specialized diets that restrict amino acids like serine can benefit human patients. It is a bold approach, one that requires collaboration across disciplines. Neurosurgeons, oncologists, biomedical engineers, and physiologists all contributed to the study, working together with a shared urgency to outsmart one of medicine’s deadliest foes.
Dr. Daniel Wahl, co-senior author of the study, reflected on the team’s efforts: “This is a multidisciplinary effort from across the university. It is a study that no individual investigator could do on their own, and I’m grateful to be part of a team that works together to make important discoveries that can improve treatments for our patients.”
Hope Amid the Hardship
Glioblastoma remains a formidable adversary. Its biology is complex, its resistance to treatment legendary. But this study offers something rare in the landscape of brain cancer research: hope. By revealing how tumors use sugar and amino acids differently from the healthy brain, scientists have identified new vulnerabilities—cracks in the armor of glioblastoma.
For patients and families facing this diagnosis, even the possibility of a new strategy can feel like light breaking through storm clouds. The path from discovery to treatment is long, but every step forward matters.
At its core, this research is more than science. It is a reminder that even in the darkest battles, curiosity and collaboration can carve out new possibilities. Glioblastoma may be the deadliest brain tumor, but it is not invincible. With each new insight, researchers move closer to a future where patients are given not just more time, but more life.
More information: Andrew J. Scott et al, Rewiring of cortical glucose metabolism fuels human brain cancer growth, Nature (2025). DOI: 10.1038/s41586-025-09460-7