In the quiet moments when a woman begins to navigate the fog of hot flashes, sleep disturbances, or the profound hormonal shifts after surgery, hormone therapy often offers a much-needed light. It promises relief. But in the background, there’s always been a lingering question: What might it cost later?
Now, in a landmark study from the National Institutes of Health (NIH), scientists have uncovered new insights into how two common forms of hormone therapy may affect breast cancer risk in younger women—offering not only answers, but also more personalized direction for those facing life-altering health decisions.
Published in The Lancet Oncology, this large-scale investigation drew from data on more than 459,000 women under the age of 55 across North America, Europe, Asia, and Australia. The study’s scale is unprecedented—and so is its impact.
Two Hormones, Two Different Paths
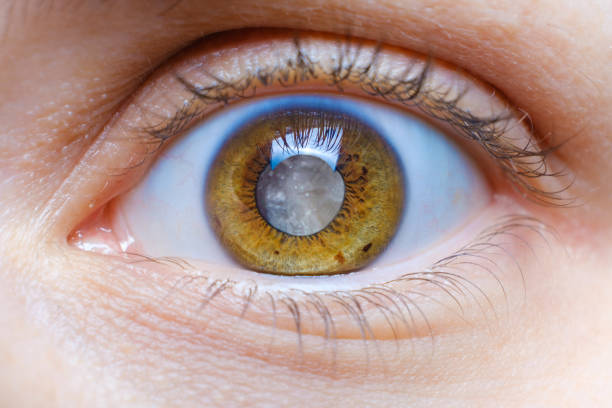
The research focused on two widely used forms of hormone therapy: unopposed estrogen hormone therapy (E-HT) and estrogen plus progestin hormone therapy (EP-HT). These therapies are most often used to relieve symptoms of menopause, or to balance hormones after surgeries like hysterectomy (removal of the uterus) or oophorectomy (removal of one or both ovaries).
The results? Striking.
Women who used E-HT were 14% less likely to develop breast cancer compared to those who had never used hormone therapy. That protective effect grew even stronger for women who started E-HT at younger ages or used it for longer periods.
But the picture shifted with EP-HT. Women who used this combined therapy had a 10% higher risk of developing breast cancer than non-users—and that number rose to 18% for those who had taken EP-HT for more than two years.
“This is not a minor difference,” said lead author Katie O’Brien, Ph.D., of the NIH’s National Institute of Environmental Health Sciences (NIEHS). “We’re talking about a noticeable shift in risk based on the type and duration of hormone therapy.”
The numbers tell a sobering story. For women using EP-HT, the estimated cumulative risk of developing breast cancer before age 55 was 4.5%. For those who never used hormone therapy, it was 4.1%. But for women using E-HT, it was only 3.6%.
Why Surgery Status Matters
One of the most compelling parts of the study centers on how surgical history—specifically, whether a woman has had a hysterectomy or oophorectomy—can dramatically influence how hormone therapy interacts with breast tissue.
Unopposed estrogen therapy (E-HT) is typically prescribed only to women who have had a hysterectomy, because taking estrogen alone with an intact uterus increases the risk of endometrial cancer. In these women, E-HT appears to offer not just symptom relief but also a modest protective effect against breast cancer.
But for women with an intact uterus and ovaries, who are instead prescribed EP-HT to reduce the risk of uterine cancer, the balance of benefits and risks becomes more complicated. According to the study, the breast cancer risk from EP-HT was significantly elevated in women without prior gynecological surgery.
“Women and their health care providers should weigh the benefits of symptom relief against the potential risks associated with hormone therapy, especially EP-HT,” said Dale Sandler, Ph.D., senior NIEHS scientist and co-author of the study. “This is not a one-size-fits-all decision. Personal medical history—including surgeries—must be factored into every conversation.”
A Milestone for Younger Women
Previous research on hormone therapy and breast cancer has largely focused on older, postmenopausal women. What makes this study so groundbreaking is its focus on younger women—those under 55, many of whom are dealing with early menopause or surgical menopause brought on by cancer treatments or other medical conditions.
This newer, younger demographic is often left with few clear answers and even fewer studies tailored to their age group. This study, by contrast, is a comprehensive, data-rich analysis that spans multiple continents, providing the kind of detailed, nuanced information that physicians and patients have long needed.
“Our study provides a greater understanding of the risks associated with different types of hormone therapy,” O’Brien said. “We hope this will help patients and their doctors develop more informed treatment plans that are tailored to individual needs and histories.”
A Story of Balance and Choice
Menopause is not a singular moment. For many women, it’s a long, challenging transition that affects the body, brain, and emotions. Hormone therapy can be life-changing. It can restore sleep. Improve mental clarity. Ease pain and discomfort. But it is not without risks.
What this study offers is not fear—but clarity. It draws a sharper line between therapies and outcomes, offering a clearer roadmap for physicians and patients to navigate.
For a woman in her late 40s, facing the sudden vacuum of hormones after surgery, knowing that E-HT might lower her breast cancer risk—if she’s had a hysterectomy—can be empowering. For another woman with an intact uterus and ovaries, learning that prolonged use of EP-HT may slightly increase her risk can guide her toward shorter courses of therapy or alternative treatments.
The Bigger Picture: A Shift Toward Personalized Care
This research aligns with a larger trend in medicine: the shift from broad recommendations to individualized care. Hormone therapy is no longer just about symptom relief—it’s about understanding each woman’s unique biological landscape and risks.
As researchers continue to unpack the complex relationship between hormones and cancer, studies like this offer a crucial foundation. They don’t provide absolute answers. But they illuminate the trade-offs, the risks, the possibilities—so that no woman has to walk this journey blind.
For now, the message is simple and powerful: Ask the questions. Understand the options. Make the choice that’s right for you.
And in those conversations—between patient and doctor, between woman and her future—this science may be the most empowering tool of all.