High blood pressure, or hypertension, has been called the “silent killer.” It creeps up without warning, often without symptoms, yet it is one of the strongest predictors of heart attacks, strokes, kidney failure, and early death. Globally, about 1.3 billion people live with hypertension, and in nearly half of these cases, the condition is uncontrolled or resistant to standard treatments. In the UK alone, around 14 million people are affected.
For many, medications can help bring blood pressure under control. But for a substantial number of patients, even multiple drugs are not enough. Their blood pressure remains dangerously high, putting them at constant risk. For these individuals, every new advance in treatment brings not just scientific progress but real, tangible hope.
A Landmark Clinical Trial
That hope may have taken a giant step forward with the results of the international BaxHTN Phase III trial, led by Professor Bryan Williams of the UCL Institute of Cardiovascular Science. The study, involving nearly 800 patients across 214 clinics worldwide, tested a new drug called baxdrostat.
The results, presented at the prestigious European Society of Cardiology (ESC) Congress 2025 in Madrid and published simultaneously in the New England Journal of Medicine, were striking. Patients who took baxdrostat tablets (either 1 mg or 2 mg daily) saw their blood pressure fall by 9–10 mmHg more than those taking placebo after just 12 weeks.
This reduction may sound modest, but in cardiovascular medicine, it is profound. A drop of even 5 mmHg in systolic blood pressure can significantly reduce the risk of major cardiovascular events. Here, the effect was nearly double that. In fact, around four in ten patients reached healthy blood pressure levels with baxdrostat, compared with fewer than two in ten on placebo.
Professor Williams summed up the excitement: “Achieving a nearly 10 mmHg reduction in systolic blood pressure with baxdrostat in the BaxHTN Phase III trial is exciting, as this level of reduction is linked to substantially lower risk of heart attack, stroke, heart failure, and kidney disease.”
How Baxdrostat Works
To understand why baxdrostat is so promising, we must look at the hormone aldosterone.
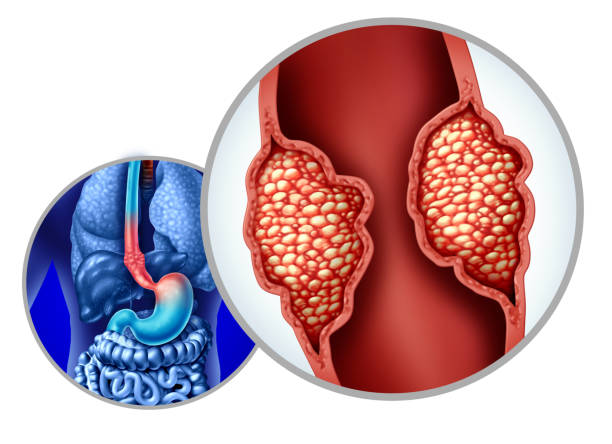
Aldosterone plays a vital role in regulating how the kidneys manage salt and water. But in some people, the body produces too much of it. This excess aldosterone traps salt and water in the body, pushing blood pressure upward. For decades, scientists have suspected that aldosterone dysregulation lies behind many cases of stubbornly high blood pressure.
The challenge has been finding a way to target it safely and effectively.
Baxdrostat represents a breakthrough because it works by directly blocking the production of aldosterone. Instead of treating the symptoms of hypertension, it addresses one of its underlying biological drivers. By cutting off the source of excess aldosterone, the drug reduces fluid retention and lowers blood pressure more effectively than many existing treatments.
Professor Williams explained: “These findings are an important advance in treatment and in our understanding of the cause of difficult-to-control blood pressure.”
Long-Term Benefits Without Safety Surprises
In addition to its effectiveness, baxdrostat also showed encouraging safety results. The benefits were not fleeting—the blood pressure reductions persisted for up to 32 weeks of treatment, with no unexpected adverse effects.
For patients and doctors alike, this is critical. A drug that lowers blood pressure dramatically but comes with serious risks would be difficult to justify. The fact that baxdrostat delivered significant, sustained benefits without new safety concerns makes it a strong candidate for widespread use in the near future.
The Wider Impact
The global implications of this breakthrough are enormous. While hypertension was once thought of as primarily a Western problem, that picture has shifted. Improved awareness and reduced salt consumption have helped bring down rates in some higher-income countries. But in lower-income nations—particularly across Asia—the burden of high blood pressure has surged.
Today, more than half of the world’s hypertensive population lives in Asia, including an estimated 226 million in China and 199 million in India.
For these populations, resistant hypertension is especially dangerous because access to advanced medical care is limited. A simple, once-daily tablet that effectively lowers blood pressure could transform public health outcomes on a massive scale.
Professor Williams emphasized this potential: “The results suggest that this drug could potentially help up to half a billion people globally—and as many as 10 million people in the UK alone, especially at the new target level for optimal blood pressure control.”
A Turning Point in the Fight Against Hypertension
Hypertension has often been described as a problem we can manage but never fully solve. Current treatments, while effective for many, leave millions vulnerable. Baxdrostat may mark a turning point.
By targeting the hormonal roots of resistant hypertension, it offers a new way forward—one that could save lives, reduce the burden on healthcare systems, and bring relief to patients who have long felt trapped by their condition.
For now, more follow-up and real-world testing will be needed to confirm its long-term effectiveness and safety. But for the millions of people who live with the constant shadow of uncontrolled blood pressure, baxdrostat is more than just a new drug. It is a symbol of hope, proof that science continues to push forward against the world’s most relentless killers.
Looking Ahead
The story of baxdrostat is not just about one medicine—it is about the power of medical research to transform lives. It shows how decades of curiosity, persistence, and innovation can lead to discoveries that change the world.
Hypertension may be silent, but the message from this trial is loud and clear: progress is possible, and for millions of people at risk, the future looks brighter than ever.
More information: Efficacy and Safety of Baxdrostat in Uncontrolled and Resistant Hypertension, New England Journal of Medicine (2025). DOI: 10.1056/NEJMoa2507109