There is something haunting about the way Multiple Sclerosis enters a person’s life. It rarely arrives with a loud bang or a definitive moment of recognition. Instead, it tiptoes in like a thief in the night—stealing coordination, vision, and control bit by bit, leaving its victims confused and frightened. For many, the early signs feel like fleeting inconveniences. A tingling in the fingers, a patch of numbness on the skin, or a bout of blurry vision might pass almost unnoticed. But these seemingly benign symptoms mark the start of a much deeper battle: one between the body and itself, waged along the fragile pathways of the central nervous system.
Multiple Sclerosis, or MS, is one of the most confounding autoimmune diseases in the medical world. It targets the brain and spinal cord—the very control center of the human body—and does so with chilling precision. Its effects can range from minor to life-altering, and its course is often unpredictable. For those diagnosed with MS, life becomes an uncharted road filled with uncertainty. But what makes this condition so fascinating is not just what it does—but how it does it. This is not a virus or a bacteria invading from the outside. MS is the body’s own defense system making a tragic mistake, turning its weaponry on the very structures it’s supposed to protect.
The Architecture of the Nervous System Under Siege
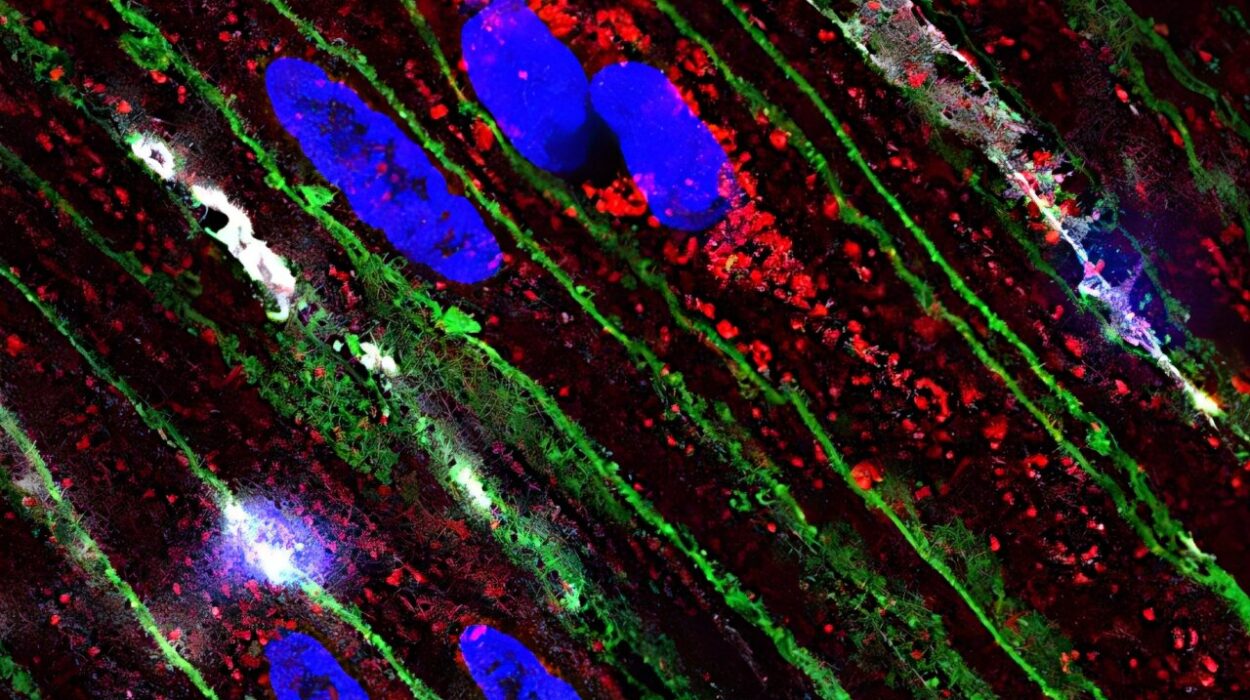
To understand the damage done by MS, we must first explore the marvel it corrupts. The human nervous system is a complex and elegant web of communication, connecting every thought, movement, and sensation. It operates with the efficiency of a high-speed superhighway, transmitting electrical impulses between the brain, spinal cord, and the rest of the body. At the heart of this system lie neurons—nerve cells wrapped in a protective, insulating sheath known as myelin. This myelin is not merely a buffer; it is essential to the speed and accuracy of nerve signal transmission.
In a healthy individual, this insulation allows messages to travel seamlessly, enabling a person to walk, speak, see, and think without effort. But in someone with MS, this delicate system becomes the battlefield. The immune system, in a grave act of misidentification, launches an attack on the myelin sheath. The resulting inflammation leads to the destruction or scarring of myelin, a process known as demyelination. The exposed nerves then become vulnerable, and over time, even the nerve fibers themselves may be damaged or severed.
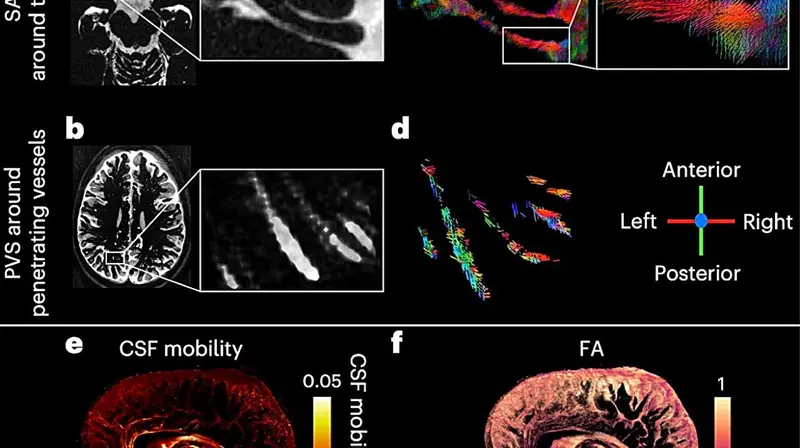
This demyelination interferes with the brain’s ability to send signals to the rest of the body. Messages are delayed, distorted, or blocked entirely. It is akin to frayed electrical wires trying to carry a current—they might still work intermittently, but they’re unreliable and unsafe. The areas where myelin has been damaged can be seen in MRI scans as lesions or plaques, stark white scars dotting the gray landscape of the brain and spinal cord.
The Immune System’s Fatal Miscalculation
The question that lies at the heart of MS is one that echoes through the study of all autoimmune diseases: Why does the immune system attack what it is supposed to protect? In MS, T-cells—normally the body’s foot soldiers against pathogens—begin crossing the blood-brain barrier, a shield meant to keep harmful substances out of the central nervous system. Once inside, they mistakenly identify myelin as a foreign invader and begin a destructive assault.
The reasons behind this betrayal are not fully known. Researchers believe there is a combination of genetic predisposition and environmental triggers at play. Certain genes may increase susceptibility, and factors like viral infections, vitamin D deficiency, and smoking may act as catalysts. But while science continues to piece together the causes, the reality for those living with MS is already in motion.
The immune attack is not a one-time event. It often comes in waves—periods of disease activity followed by times of remission, when the body temporarily repairs the damage. Over time, though, the nervous system’s ability to recover diminishes. The damage accumulates, and symptoms become more permanent.
The Faces and Forms of MS
Multiple Sclerosis does not wear a single face. Its manifestations are as varied as the individuals it affects, which makes it one of the most complex conditions to diagnose and manage. Some people may experience a single episode of neurological dysfunction and never have another. Others may encounter a steady, relentless decline in function from the outset. The medical community has categorized MS into several types based on its progression, though the lines between these categories are not always clearly defined.
Relapsing-remitting MS is the most common form at diagnosis. It is characterized by distinct episodes of symptoms (relapses), followed by periods of partial or complete recovery (remissions). During remissions, inflammation subsides, and the body often repairs some of the damage. For many, this cycle may continue for years.
Eventually, some patients transition to secondary progressive MS. In this form, the disease begins to advance more steadily, with or without relapses. The neurological damage becomes more permanent, and disability tends to increase over time. There is also primary progressive MS, in which individuals experience a gradual worsening of symptoms from the beginning without clear relapses or remissions.
Because no two cases are alike, MS presents a diagnostic and therapeutic challenge. Its symptoms can mimic those of other neurological conditions. Its pace can shift unpredictably. For the person living with MS, each day can feel like navigating a shifting landscape—never entirely sure which faculties will be intact and which will falter.
Symptomatology: A Symphony of Disruption
The symptoms of MS can be subtle or dramatic, fleeting or persistent. They vary depending on the location and extent of nerve damage. A person might wake up one morning with double vision or find that their limbs feel heavy and unresponsive. Fatigue, one of the most common and debilitating symptoms, often descends like a fog—unrelated to exertion and impervious to rest.
Motor symptoms can include muscle weakness, tremors, and difficulty with coordination and balance. These challenges can make walking a strenuous, sometimes impossible, task. Spasticity, or muscle stiffness, adds another layer of difficulty, transforming simple movements into painful struggles.
Sensory disturbances are equally common. Numbness, tingling, and a burning or electric-shock sensation may occur in various parts of the body. Visual problems—such as optic neuritis, where inflammation of the optic nerve causes pain and vision loss—can be an early sign. In some, MS even affects speech, swallowing, and bladder or bowel function.
Perhaps most frustrating of all are the cognitive effects. Many patients experience “brain fog,” difficulty concentrating, memory lapses, or slowed thinking. These symptoms can affect relationships, careers, and self-esteem. Depression and anxiety are also prevalent, both as direct effects of neurological disruption and as natural emotional responses to living with a chronic illness.
Diagnosis: The Search for Confirmation
Diagnosing MS is a process of elimination, pattern recognition, and technological assistance. There is no single definitive test. Instead, neurologists rely on a combination of clinical examination, medical history, MRI scans, spinal fluid analysis, and other assessments to make a diagnosis.
An MRI can reveal lesions in the brain and spinal cord that are characteristic of MS. These appear as bright spots, indicating areas where myelin has been damaged. A lumbar puncture can detect specific immune markers in the cerebrospinal fluid—evidence that the immune system is active within the central nervous system. Evoked potential tests, which measure the electrical activity in response to stimuli, can uncover delayed nerve conduction, even when a person has no visible symptoms.
Because symptoms can be so variable and intermittent, diagnosis can be delayed, especially when the signs are mild or attributed to other causes. For patients, the journey to diagnosis can be long and emotionally draining, marked by frustration, misdiagnoses, and anxiety. But receiving a definitive diagnosis, while terrifying, can also be a relief. It gives a name to the enemy and opens the door to treatment.
Treatment: Calming the Storm
There is currently no cure for MS, but the arsenal of treatments has grown significantly in recent decades. The goals are to reduce the frequency and severity of relapses, slow disease progression, and manage symptoms. Treatment often involves a combination of medication, rehabilitation, lifestyle modifications, and psychological support.
Disease-modifying therapies (DMTs) are the cornerstone of MS treatment. These medications work by altering the immune system’s activity to reduce inflammation and the frequency of relapses. Some are injectable, some are oral, and others are administered via infusion. While not without side effects, these drugs have dramatically improved long-term outcomes for many patients.
During an acute relapse, corticosteroids may be prescribed to reduce inflammation and speed recovery. These powerful anti-inflammatories can provide quick relief, though their long-term use is limited by significant side effects.
Symptom management is a critical part of living with MS. Physical therapy helps maintain strength and mobility. Occupational therapy assists with daily living skills. Speech therapy can improve communication and swallowing. Medications may be used to treat specific symptoms such as spasticity, fatigue, or bladder dysfunction.
More than ever, treatment plans are becoming personalized. Neurologists consider each patient’s disease course, lifestyle, and risk factors when crafting a strategy. This individualized approach is crucial in a condition as variable as MS.
The Human Side of MS
Behind every MRI image and clinical trial is a person navigating the emotional terrain of a life changed forever. Living with MS often means confronting an uncertain future while trying to maintain a sense of normalcy. It requires daily courage—to take medication, to attend therapy, to get out of bed despite pain and fatigue.
The emotional toll is profound. Many people with MS grieve the loss of abilities and independence. They may struggle with identity, relationships, and career changes. But amid these challenges, there is also resilience. Communities of MS patients have formed worldwide, offering support, resources, and hope. Stories of perseverance, adaptation, and even triumph are common among those living with the disease.
Family and friends play a critical role in supporting someone with MS. Understanding, patience, and practical assistance can make a world of difference. Education is key—both for those diagnosed and their loved ones. The more people know about the condition, the better they can respond to its demands.
Hope on the Horizon
Research into MS is more vibrant than ever. Scientists are uncovering new insights into the immune system, the genetic factors involved, and the potential role of environmental influences. Advanced imaging techniques are shedding light on how damage occurs and how it might be prevented or repaired.
Some of the most exciting work involves remyelination—stimulating the body’s ability to regenerate myelin. Stem cell therapies, while still experimental, offer hope for repairing damaged nerves. Investigational drugs are targeting new pathways in the immune system. Clinical trials are exploring everything from neuroprotective agents to gut microbiome interventions.
While a definitive cure remains elusive, the progress made over the last few decades is astounding. What was once a relentlessly debilitating condition can now be managed effectively in many cases. The future holds promise—not just for better treatments but for deeper understanding.
Conclusion: The Battle Within
Multiple Sclerosis is, at its heart, a war within—a betrayal by the very forces designed to protect. It is a disease that humbles science, frustrates medicine, and tests the spirit. But it is also a reminder of the body’s complexity, the mind’s resilience, and the incredible capacity of people to adapt and endure.
The road with MS is not easy, but it is not without light. Through research, support, and awareness, the landscape is shifting. The hope is no longer just to endure the disease—but to conquer it.