In the quiet world of neuroscience, few conditions are as perplexing and misunderstood as Multiple Sclerosis (MS). It is a disease that seems to appear from nowhere, affecting millions of people around the world, yet its causes remain elusive. Often invisible to the outside world, the symptoms of MS can range from fatigue to paralysis, from brain fog to severe motor dysfunction, leading to a complex and multifaceted disorder that has baffled doctors for centuries.
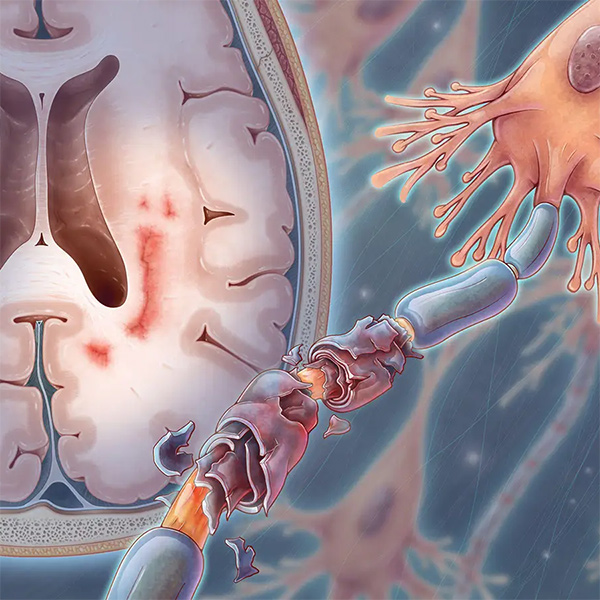
Multiple Sclerosis is a disease of the central nervous system (CNS), where the body’s immune system attacks its own tissues. Specifically, it targets the myelin sheath—the protective covering that encases nerve fibers in the brain and spinal cord. When myelin is damaged, the transmission of electrical impulses along the nerves is slowed or completely blocked, disrupting communication between the brain and the rest of the body. It is this disruption that leads to the varied symptoms that people with MS experience.
What is Multiple Sclerosis?
But MS is not just an affliction of the body; it’s a journey into the unknown. It represents a silent war within the body, one where the immune system, typically the body’s protector, turns against it. It is a constant battle that is fought on a cellular level, and for those who live with it, the struggle is often an emotional, psychological, and physical one.
Multiple Sclerosis is a chronic autoimmune disease that primarily affects the central nervous system, which includes the brain and spinal cord. It is characterized by the progressive damage to the myelin sheath, a fatty substance that insulates and protects nerve fibers. Myelin is essential for the smooth and rapid transmission of electrical signals between the brain and the body. Without it, nerve impulses are slowed or blocked, leading to a wide range of neurological symptoms.
The exact cause of MS remains uncertain. However, scientists believe it results from a combination of genetic and environmental factors. Certain genes appear to make individuals more susceptible to developing the disease, but these genetic markers alone do not fully explain the onset of MS. Environmental triggers, such as viral infections or vitamin D deficiency, are thought to play a role in initiating the autoimmune response.
Unlike many other diseases, where the body’s immune system is designed to protect against external threats, in MS, the immune system mistakenly attacks the body’s own cells. This leads to the inflammation and scarring (sclerosis) of nerve fibers, which disrupts their ability to function properly. This process is referred to as demyelination, and over time, it causes permanent damage to the affected nerves.
The Immune System Gone Rogue
The immune system is a remarkable network of cells and proteins that works tirelessly to defend the body from harmful invaders, such as viruses, bacteria, and other pathogens. Under normal circumstances, the immune system detects and eliminates these threats with precision. However, in individuals with Multiple Sclerosis, the immune system mistakenly identifies myelin as a foreign invader and begins to attack it.
The exact trigger for this malfunction is still debated, but researchers believe that a viral infection, such as the Epstein-Barr virus (which causes mononucleosis), may play a role in initiating the autoimmune response. The body, in an attempt to fight off the infection, begins to produce immune cells that target not only the virus but also the myelin sheath surrounding nerve fibers.
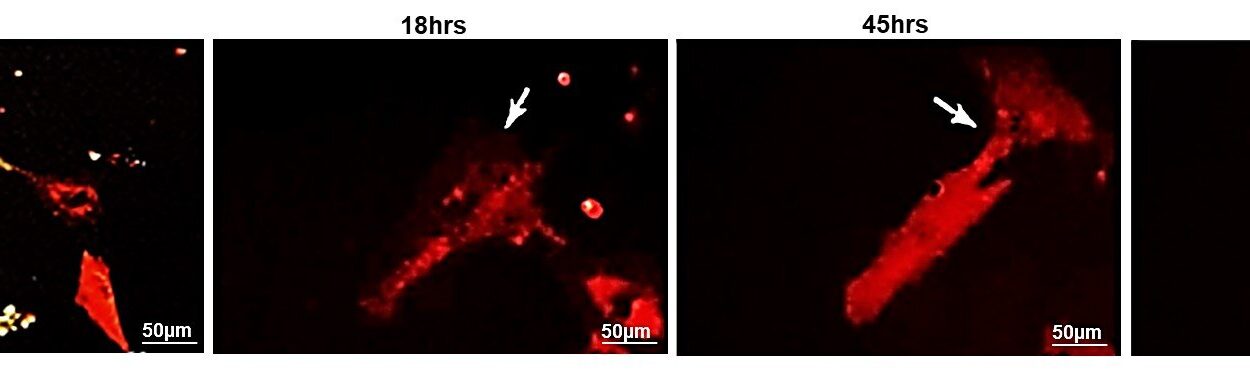
This misguided immune attack causes inflammation in the affected areas of the brain and spinal cord. The body’s repair mechanisms attempt to fix the damage, but over time, this process becomes less effective. As a result, the damaged areas of the nervous system become scarred and hardened, leading to the characteristic plaques or lesions seen in MS patients. These lesions can occur in any part of the CNS, and their location and size determine the symptoms a person experiences.
The immune attack in MS is often described as a “relapsing-remitting” pattern. This means that individuals experience periods of worsening symptoms (relapses) followed by periods of stability or partial recovery (remissions). However, over time, the disease may progress to a stage where remissions become less frequent, and the damage becomes more permanent. This phase is known as secondary progressive MS.
Symptoms: A Shifting Landscape
The symptoms of Multiple Sclerosis can be as diverse as the individuals who experience them. No two people with MS will have the same symptoms, and the severity of those symptoms can vary widely from one person to another. Some individuals may experience only mild discomfort, while others may face significant disability. The symptoms often come and go, sometimes suddenly and without warning, making MS a particularly unpredictable disease.
The most common symptoms of MS include:
- Fatigue: This is one of the most debilitating symptoms of MS, affecting up to 80% of people with the condition. MS-related fatigue is not simply the feeling of being tired after a long day; it is a profound and persistent exhaustion that does not improve with rest. This fatigue can interfere with daily activities, making even simple tasks feel overwhelming.
- Numbness and Tingling: Many people with MS report experiencing a sensation of numbness or tingling in their limbs, face, or other parts of the body. This occurs when the nerves responsible for transmitting sensory information are damaged.
- Muscle Weakness and Spasms: MS can cause muscle weakness, making it difficult for individuals to walk, climb stairs, or perform everyday tasks. Muscle spasms, also known as spasticity, can result in painful and involuntary muscle contractions, often in the legs.
- Vision Problems: Optic neuritis, an inflammation of the optic nerve, is a common symptom of MS. It can cause blurred vision, double vision, or even temporary blindness in one eye. Vision problems are often one of the first signs of MS.
- Balance and Coordination Issues: MS can affect the cerebellum, the part of the brain responsible for coordinating movement. This can lead to difficulty with balance, walking, and performing tasks that require fine motor skills.
- Cognitive Changes: MS can affect memory, attention, and the ability to process information. These cognitive changes, often referred to as “MS brain fog,” can make it difficult to concentrate, solve problems, or retain information.
- Bladder and Bowel Dysfunction: Many individuals with MS experience urinary urgency, incontinence, or difficulty emptying the bladder. Constipation and difficulty with bowel control are also common.
- Pain: Chronic pain, including headaches, neuropathic pain, and musculoskeletal pain, is common in people with MS. The pain can be sharp, stabbing, or aching and can significantly impact quality of life.
The severity and course of these symptoms depend on the extent and location of the damage to the nervous system. Some individuals may experience only mild symptoms that do not progress, while others may face more severe disability as the disease advances.
Diagnosing Multiple Sclerosis: A Puzzle of Symptoms
Diagnosing MS can be a complex and frustrating process. There is no single test that can definitively diagnose the disease, and many of its symptoms overlap with other conditions. Because MS is a disease of the central nervous system, it often requires a thorough examination by a neurologist, along with a series of diagnostic tests.
One of the most important tools for diagnosing MS is magnetic resonance imaging (MRI). An MRI uses strong magnets and radio waves to create detailed images of the brain and spinal cord, allowing doctors to identify lesions or plaques that are characteristic of MS. However, an MRI alone is not enough to make a diagnosis, as lesions can also be caused by other conditions.
To make a definitive diagnosis, doctors will also consider the patient’s medical history, symptoms, and neurological examination. In some cases, a lumbar puncture (spinal tap) may be performed to analyze cerebrospinal fluid for markers of inflammation and immune activity that are commonly seen in MS.
The diagnostic process can be frustrating, as it may take months or even years to confirm a diagnosis. In some cases, individuals may be initially misdiagnosed with other conditions, only to later receive a diagnosis of MS.
Treatment: Managing an Unpredictable Disease
While there is currently no cure for Multiple Sclerosis, there are treatments available that can help manage symptoms, reduce the frequency and severity of relapses, and slow the progression of the disease. The treatment approach for MS is highly individualized and depends on the specific form of the disease, the severity of symptoms, and the overall health of the patient.
There are three main types of treatment for MS:
- Disease-Modifying Therapies (DMTs): These medications aim to reduce the frequency of relapses and slow the progression of the disease. DMTs work by modifying the immune system’s response to prevent it from attacking the myelin sheath. Some DMTs are taken orally, while others are administered through injections or infusions. Common DMTs include interferon beta, glatiramer acetate, and more recently, monoclonal antibodies such as natalizumab and ocrelizumab.
- Steroids: During periods of relapse or flare-ups, high-dose corticosteroids may be prescribed to reduce inflammation and shorten the duration of the relapse. Steroids can help manage acute symptoms, but they do not alter the long-term course of the disease.
- Symptom Management: In addition to DMTs, individuals with MS may take medications to help manage specific symptoms, such as pain, muscle spasticity, and bladder dysfunction. Physical therapy, occupational therapy, and speech therapy can also help individuals maintain mobility, strength, and independence.
The goal of MS treatment is to help individuals maintain the best possible quality of life while managing the unpredictable nature
of the disease. Because MS affects each person differently, treatment plans are often adjusted over time to address changing symptoms and disease progression.
Living with Multiple Sclerosis: A Journey of Resilience
Living with Multiple Sclerosis is a journey of resilience, adaptation, and hope. It is a disease that can challenge both the body and the mind, forcing individuals to navigate a landscape that is constantly shifting. But despite the difficulties, many people with MS lead full and active lives, continuing to pursue their passions and contribute to their communities.
Support from family, friends, and healthcare professionals is essential in helping individuals cope with the emotional and physical challenges of MS. Psychosocial support, including counseling and support groups, can help individuals manage the emotional impact of the disease, while physical therapy and rehabilitation can provide strategies for maintaining independence.
Advances in research and treatment continue to offer hope for the future. New medications, therapies, and diagnostic tools are being developed, and scientists are learning more about the underlying causes of MS. With each discovery, the possibility of a cure or more effective treatments becomes more tangible.
Conclusion: The Road Ahead
Multiple Sclerosis is a disease that touches the lives of millions, yet its mysteries remain vast. The journey through MS is one of uncertainty and resilience, but it is also a journey of hope. As research advances and treatment options improve, there is reason to believe that the future holds better outcomes for those living with MS. It is a disease that challenges the body, the mind, and the spirit—but it is also one that sparks a fight for a better tomorrow.
The road ahead is still uncertain, but with greater awareness, understanding, and compassion, the world can continue to move toward a future where MS is no longer a life sentence, but a challenge that can be met and conquered.