Lupus is a condition that sits at the crossroads of mystery and science, a disease that has puzzled doctors and researchers for decades. Known medically as systemic lupus erythematosus (SLE), lupus is an autoimmune disorder in which the immune system—the body’s own defense force—turns against itself. Instead of protecting against infections, viruses, and bacteria, the immune system mistakenly attacks healthy cells, tissues, and organs.
The result can be inflammation, pain, and damage that affect almost any part of the body, including the skin, joints, kidneys, heart, lungs, blood vessels, and brain. What makes lupus particularly complex is its unpredictability: it can flare up suddenly, calm down, and then strike again, often with different symptoms. No two people with lupus experience it in exactly the same way, which makes it a uniquely personal disease.
To understand lupus is to understand not only the science of autoimmunity but also the human stories behind it—stories of resilience, frustration, and hope. In this article, we will explore the causes, symptoms, diagnosis, and treatment of lupus, weaving together scientific accuracy with an emotionally engaging lens that reflects what living with lupus truly means.
What Causes Lupus?
The Immune System Gone Astray
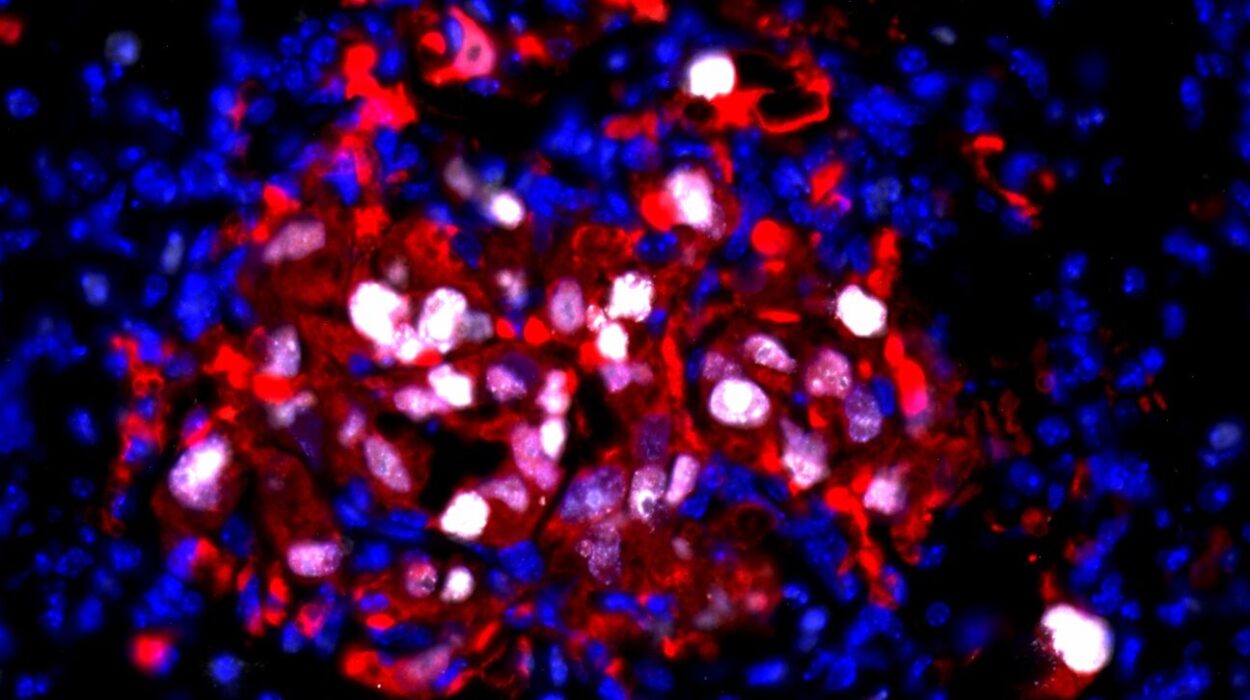
At the heart of lupus lies the immune system’s betrayal. Normally, the immune system identifies foreign invaders such as viruses and bacteria, producing antibodies to neutralize them. In lupus, the immune system mistakenly produces autoantibodies—proteins that attack the body’s own cells and tissues. This abnormal reaction triggers widespread inflammation and tissue damage.
But what causes the immune system to go astray? Scientists believe that lupus does not have a single cause but rather arises from a complex interplay of genetics, environment, and hormones.
The Role of Genetics
Genetics lays the foundation. While lupus is not directly inherited in the way eye color or blood type is, having certain genetic variations increases the risk. Researchers have identified dozens of genes linked to immune regulation, inflammation, and autoimmunity that contribute to lupus susceptibility.
If you have a family member with lupus or another autoimmune condition such as rheumatoid arthritis or multiple sclerosis, your risk may be higher. Still, most people with these genes never develop lupus, which suggests that genes alone are not enough to cause the disease.
Environmental Triggers
Environmental factors often act as the “spark” that ignites lupus in those who are genetically predisposed. Known triggers include:
- Sunlight (ultraviolet radiation): Many people with lupus are sensitive to sunlight, which can trigger skin rashes or systemic flares.
- Infections: Viral and bacterial infections may confuse the immune system, pushing it into an autoimmune response.
- Medications: Certain drugs, such as hydralazine or procainamide, can trigger drug-induced lupus, which mimics SLE but usually resolves after stopping the medication.
- Toxins and chemicals: Exposure to silica dust, cigarette smoke, or other environmental toxins may increase the risk of lupus.
Hormonal Influence
Lupus predominantly affects women—about 90% of lupus patients are female, particularly those of childbearing age. This strong gender bias points to a role of hormones, especially estrogen, in influencing immune function. While estrogen does not directly cause lupus, it may make the immune system more prone to overreaction in genetically susceptible individuals.
A Multifactorial Puzzle
Taken together, lupus is best understood as a multifactorial disease. Genes set the stage, environmental exposures act as triggers, and hormones influence the disease’s expression. The result is a highly variable, unpredictable condition that defies simple explanations.
The Symptoms of Lupus
The Challenge of Variability
One of the reasons lupus is so difficult to diagnose and manage is its incredible diversity of symptoms. Often referred to as “the great imitator,” lupus can mimic many other diseases, from arthritis to skin conditions to kidney disease. Symptoms can range from mild to life-threatening, vary over time, and differ widely between individuals.
Common Symptoms
Some of the most frequent symptoms include:
- Fatigue: An overwhelming tiredness that does not improve with rest is one of the most common and debilitating symptoms.
- Joint pain and stiffness: Often mistaken for arthritis, lupus can cause swelling and pain in multiple joints.
- Skin rashes: The classic “butterfly-shaped” rash across the cheeks and nose is iconic, but lupus can also cause lesions elsewhere on the body.
- Photosensitivity: Sunlight exposure often worsens rashes and can trigger systemic flares.
- Fever: Low-grade fevers are common during disease activity.
- Hair loss: Diffuse thinning or patchy hair loss may occur during flares.
Organ-Specific Symptoms
Because lupus can affect nearly any organ, symptoms may also include:
- Kidneys: Lupus nephritis can lead to swelling in the legs, high blood pressure, and abnormal urine tests.
- Heart and lungs: Inflammation may cause chest pain, shortness of breath, or fluid around the organs.
- Blood and vessels: Anemia, clotting problems, and increased risk of cardiovascular disease are common.
- Brain and nerves: Lupus can cause headaches, seizures, confusion, or memory problems.
The Flare-Remission Cycle
Lupus symptoms often follow a cycle of flares and remission. During flares, symptoms worsen as inflammation rises; during remission, symptoms improve or disappear. This unpredictable cycle adds to the emotional and physical burden of living with lupus.
Diagnosing Lupus
The Diagnostic Challenge
There is no single test that can definitively diagnose lupus. Because its symptoms overlap with many other conditions, diagnosis often requires a combination of clinical evaluation, laboratory tests, and careful medical history. On average, patients may wait years for a confirmed diagnosis, enduring uncertainty along the way.
Clinical Criteria
Doctors often rely on established classification criteria developed by organizations like the American College of Rheumatology (ACR) or the Systemic Lupus International Collaborating Clinics (SLICC). These criteria include symptoms, physical findings, and laboratory abnormalities. A patient typically must meet several criteria for a diagnosis of lupus.
Blood Tests
Laboratory tests are essential in supporting a diagnosis. Some key markers include:
- Antinuclear antibody (ANA): Present in nearly all people with lupus, though also found in other conditions.
- Anti-dsDNA and anti-Smith antibodies: More specific for lupus, indicating autoimmune activity.
- Complement levels (C3, C4): Often low during active disease, reflecting immune activation.
- Complete blood count (CBC): May reveal anemia, low white blood cells, or low platelets.
Imaging and Biopsies
If lupus affects major organs such as the kidneys, doctors may order imaging studies or perform a biopsy to assess tissue damage. A kidney biopsy, for example, helps determine the severity and type of lupus nephritis, guiding treatment decisions.
Treating Lupus
The Goal of Treatment
There is no cure for lupus, but treatment aims to control symptoms, prevent flares, and minimize organ damage. Because lupus varies so much between individuals, treatment must be highly personalized.
Medications
Several classes of drugs are commonly used:
- Nonsteroidal anti-inflammatory drugs (NSAIDs): Help relieve joint pain, muscle aches, and fever.
- Antimalarials (e.g., hydroxychloroquine): Reduce flares, protect organs, and improve skin and joint symptoms. They are considered foundational therapy for most lupus patients.
- Corticosteroids (e.g., prednisone): Powerful anti-inflammatory drugs used for moderate to severe disease, though long-term use can cause significant side effects.
- Immunosuppressants (e.g., azathioprine, mycophenolate, cyclophosphamide): Suppress the overactive immune system, especially for organ involvement.
- Biologic therapies (e.g., belimumab): Target specific immune pathways and represent newer advances in lupus treatment.
Lifestyle and Self-Care
Beyond medication, lifestyle choices play a vital role in managing lupus:
- Sun protection: Wearing sunscreen and protective clothing reduces the risk of rashes and flares.
- Balanced diet: Nutrient-rich foods help support immune balance and reduce inflammation.
- Regular exercise: Gentle activities like swimming or yoga maintain mobility and reduce fatigue.
- Stress management: Mindfulness, meditation, and adequate sleep help prevent flares.
Managing Flares
Patients learn to recognize early warning signs of flares—such as fatigue, joint pain, or skin changes—and adjust their care accordingly. Quick communication with healthcare providers often helps prevent severe flare-ups.
The Emotional and Social Impact of Lupus
Living with an Invisible Illness
For many patients, the hardest part of lupus is not the physical symptoms but the emotional and social challenges. Because lupus is often invisible—fatigue, pain, and internal organ damage are not obvious to others—patients may feel misunderstood or dismissed. Friends, family, or even healthcare providers may underestimate the seriousness of the disease.
Mental Health and Coping
Depression and anxiety are common among people with lupus, fueled by chronic pain, uncertainty, and the burden of ongoing treatment. Building resilience often requires support systems, counseling, and peer connections. Lupus support groups, both in-person and online, provide validation and community for those navigating this unpredictable condition.
The Future of Lupus Care
Advances in Research
Lupus research is advancing rapidly. Scientists are studying genetic markers to predict disease risk, exploring new biologic therapies that target specific immune pathways, and developing personalized medicine approaches. Clinical trials continue to test innovative drugs with the hope of reducing side effects and achieving longer remissions.
Toward a Cure
While a cure remains elusive, each step forward improves quality of life and reduces mortality. Survival rates for lupus have dramatically improved over the last few decades thanks to earlier diagnosis, better medications, and more comprehensive care.
Conclusion: Living with Lupus
Lupus is not just a disease—it is a journey. It demands strength, adaptability, and courage from those who live with it. While the immune system may betray them, patients with lupus show remarkable resilience, finding ways to live full and meaningful lives despite uncertainty.
Science continues to unravel the mysteries of lupus, bringing new hope to millions worldwide. Until a cure is found, treatment, support, and awareness remain powerful tools for improving outcomes. Understanding lupus—its causes, symptoms, diagnosis, and treatment—is not only a scientific necessity but also a human one. It bridges the gap between medical knowledge and the lived experiences of those who wake each day to face this unpredictable illness.