For centuries, the history of leprosy in the Americas has been cloaked in the shadows of colonialism. The prevailing narrative traced the disease back to European ships and missionaries—just one among many afflictions, from smallpox to measles, carried across the Atlantic during the so-called Age of Discovery. It was, by all appearances, a disease imposed upon the Indigenous peoples of the New World, part of the biological conquest that decimated civilizations and reshaped continents.
But a groundbreaking study published in Science is turning that narrative on its head.
In a sweeping international collaboration involving the Institut Pasteur, the CNRS (France’s National Centre for Scientific Research), the University of Colorado, and over 40 institutions across North and South America, researchers have uncovered compelling evidence that leprosy, or at least a form of it, was infecting people on the American continents long before Columbus set sail.
The culprit? Not the familiar Mycobacterium leprae, the main bacterium traditionally linked to the disease, but a close relative: Mycobacterium lepromatosis, a lesser-known and recently identified species. Using ancient DNA, genome reconstruction, and insights from archaeology and anthropology, the researchers demonstrate that M. lepromatosis has been circulating in the Americas for at least a millennium—long before the first European ships ever appeared on the horizon.
The implications are profound, not just for the history of disease in the Western Hemisphere, but for our understanding of microbial evolution, zoonotic transmission, and the interplay between humans and pathogens over deep time.
A Curious Case in the Microbial Family Tree
First identified in a Mexican patient in 2008, Mycobacterium lepromatosis emerged quietly on the global stage, a shadow sibling to the better-known M. leprae. The clinical picture it painted was similar—nerve damage, disfiguring skin lesions, long incubation periods—but not identical. It was quickly recognized as a second causative agent of Hansen’s disease, the modern name for leprosy.
In 2016, another strange discovery sent ripples through the scientific community. Researchers in the British Isles found leprosy-causing bacteria in red squirrels—specifically, strains of both M. leprae and M. lepromatosis. How had a squirrel in the UK acquired a pathogen so rarely discussed even among tropical disease specialists? Where had this bacterium really come from? And how had it traveled?
These questions prompted a deeper investigation—one that required looking not forward into modern outbreaks, but backward, into history.
Led by Dr. María Lopopolo and Dr. Nicolás Rascovan at the Laboratory of Microbial Paleogenomics at the Institut Pasteur, the team decided to search for the microbial fingerprints of M. lepromatosis in ancient remains. What they found would rewrite the pre-Columbian medical landscape.
Digging into the Past: Leprosy in the Bones
To trace the hidden history of M. lepromatosis, the researchers analyzed nearly 800 biological samples collected from both recent clinical cases and ancient human remains. The archaeological material came from sites across the Americas—from Canada to Argentina—some dating back more than a thousand years. These bones, long buried in ancestral Indigenous cemeteries, were carefully studied with the full consent and participation of the descendant communities.
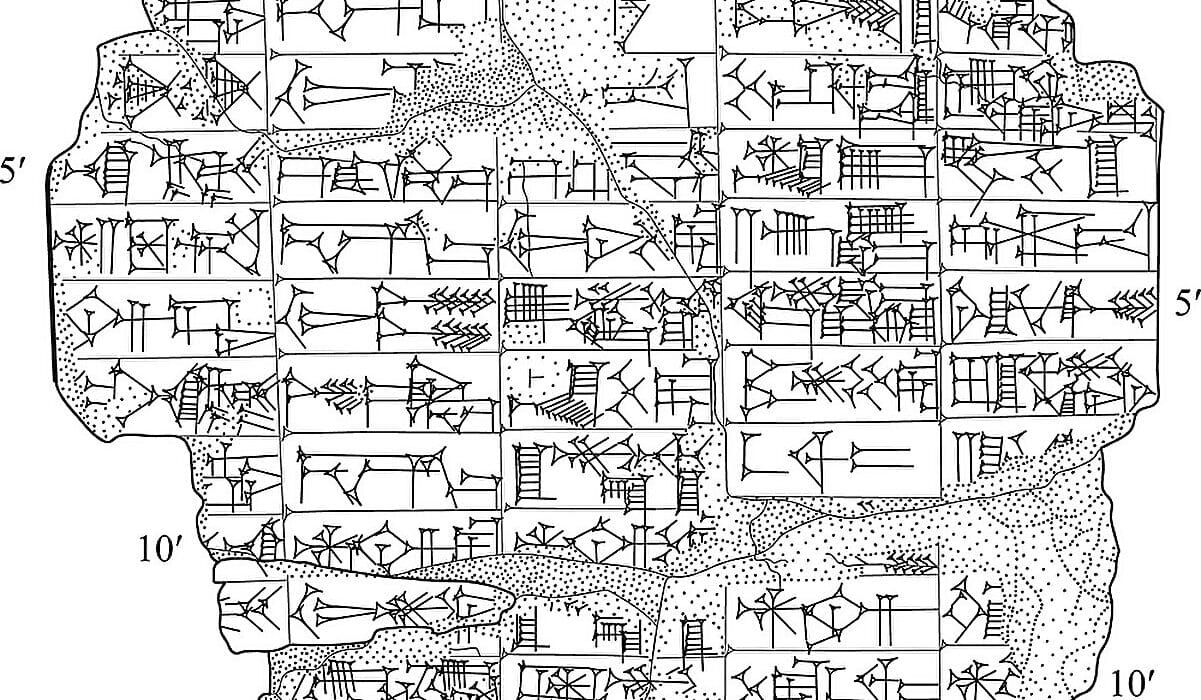
Using the powerful tools of paleogenomics, the team extracted and sequenced fragments of ancient DNA, teasing out degraded pieces of bacterial genomes from within the calcified lesions that had once marked the skeletal remains of leprosy patients. In this forensic dance between past and present, science and memory, they were able to piece together partial and even full genomes of M. lepromatosis that had been silently preserved for over a millennium.
What they found stunned even the most seasoned researchers.
These ancient strains, dating to roughly 1,000 years ago, were unmistakably M. lepromatosis. They were genetically distinct from M. leprae and, even more surprisingly, they were closely related to each other—despite being discovered thousands of kilometers apart. One genome was found in Canada. Another in Argentina. Yet the two bore such striking genetic resemblance that their last common ancestor likely lived within just a few centuries of their time of burial.
An American Original
This degree of genetic similarity, paired with the immense geographic distance between the samples, suggested a rapid and wide-ranging spread of M. lepromatosis across the Americas long before the arrival of Europeans. The data contradicted the long-held assumption that all forms of leprosy in the Western Hemisphere were post-contact imports. Instead, it pointed to a different story—one in which Indigenous populations were already coping with a uniquely American strain of the disease.
Dr. Lopopolo explains, “This discovery transforms our understanding of the history of leprosy in America. It shows that a form of the disease was already endemic among Indigenous populations well before the Europeans arrived.”
The team went further, identifying several novel lineages of M. lepromatosis, including one ancestral branch that appears to have diverged from all other known strains over 9,000 years ago. Even more intriguing, this ancient lineage has not vanished. It continues to infect modern patients in North America today, creating a living bridge between past and present.
A Pathogen on the Move
The presence of ancient leprosy in pre-Columbian populations raises another provocative question: how did M. lepromatosis arrive in the Americas in the first place?
The evolutionary divergence from M. leprae suggests a shared ancestor deep in time, likely on the Eurasian continent. But once established in the Americas, M. lepromatosis seems to have taken a separate path—evolving, adapting, and diversifying among Indigenous communities for thousands of years. Its relatively tight clustering in the evolutionary tree hints at a sudden expansion, potentially triggered by human migration patterns, trade routes, or ecological changes in the pre-Columbian era.
This microbial migration may also have included transcontinental leaps. The presence of American M. lepromatosis lineages in 19th-century red squirrels in the UK, for example, suggests a reverse journey across the Atlantic. The squirrels didn’t swim. More likely, the bacteria traveled with people—or with fur, or pets, or vermin—embedded in the increasingly global trade networks of the colonial world.
These revelations challenge the idea of pathogens as strictly national or continental in scope. They move with us, sometimes hitching rides across oceans, other times co-evolving in quiet parallel with our societies. M. lepromatosis may have made such journeys multiple times.
Animal Reservoirs and Hidden Hosts
One of the most startling discoveries of this study is the potential role of animal hosts in maintaining and spreading leprosy-causing bacteria. While M. leprae had previously been identified in armadillos and red squirrels, this study’s implications suggest that M. lepromatosis may also have unknown animal reservoirs—undiscovered carriers that have quietly preserved the bacteria in ecosystems where human cases have long disappeared.
The red squirrels in the British Isles remain the most curious case. Their infection with American strains raises questions about how wildlife diseases intersect with human history. Could fur traders have unknowingly spread leprosy across continents? Did animals act as microbial reservoirs that reintroduced the disease into human populations? These are questions the researchers are only beginning to explore.
Dr. Nicolás Rascovan, lead author of the study, notes, “We are just beginning to uncover the diversity and global movements of this recently identified pathogen. The study allows us to hypothesize that there might be unknown animal reservoirs.”
This opens new avenues for surveillance and study—not just in humans, but in wildlife populations, where these ancient pathogens may still linger.
An Ethical Collaboration Rooted in Respect
Integral to the success of the project was the deep collaboration with Indigenous communities. From the earliest stages, the research was conducted with transparent dialogue, shared decision-making, and respect for ancestral remains.
In many cases, ancient DNA studies have been criticized for their extractive approach to human remains, especially when working with Indigenous groups. But this project took a different path. Communities were involved in the design of the research, consented to the analysis of ancestral remains, and retained control over the interpretation and sharing of results.
When requested, ancient remains and samples were returned. All genetic data were stored and shared on platforms designed to meet the specific expectations of Indigenous partners. In some cases, local languages were used in final reports. It was a model for ethical genomics—where science advances not by extraction, but by relationship.
“This study clearly illustrates how ancient and modern DNA can rewrite the history of a human pathogen,” says Rascovan, “and how, when done with respect, science can also help restore historical agency to communities whose histories have been too often silenced.”
Redrawing the Map of Disease
The broader significance of this study lies not just in the history it reconstructs, but in the future it anticipates. By showing that M. lepromatosis has a much longer, richer, and more complex history in the Americas than previously believed, it forces scientists and public health officials to rethink how diseases are understood, classified, and controlled.
For one, it challenges the oversimplified binary of “Old World” vs. “New World” diseases. Microbes do not respect historical epochs or colonial boundaries. They travel, adapt, and evolve. The fact that leprosy—one of the most symbolically charged diseases in Western history—may have had an independent evolutionary path in the Americas is both astonishing and deeply humbling.
Secondly, it underscores the importance of studying ancient DNA. Many pathogens we consider “modern” may have been circulating in human populations for thousands of years, their histories buried not just in bones, but in genomes. By reviving these histories, scientists can better understand how pathogens behave today—how they mutate, where they hide, and how they might reemerge.
Finally, this study is a reminder that disease is not just biological—it is also cultural, political, and historical. The stigma of leprosy, which has caused untold suffering and isolation, rests in part on myths of origin and transmission. Correcting those myths with science is not just an academic exercise—it is an act of justice.
A New Chapter in an Old Story
In the end, the discovery of pre-Columbian leprosy in the Americas is more than a scientific breakthrough. It is a rewriting of one of the oldest chapters in the story of disease. It reminds us that humanity’s relationship with microbes is ancient, intimate, and complex—and that sometimes, what we think we know about history is only the tip of the biological iceberg.
The microbes that once haunted the lives of people buried a thousand years ago in Canada and Argentina are not gone. They live on—in red squirrels in the British Isles, in patients today in North America, and in the evolving story of science itself.
This new understanding of Mycobacterium lepromatosis marks a turning point—not just for the study of leprosy, but for how we see the deep intertwining of biology and human history. And it proves, once again, that sometimes the greatest revolutions begin not in laboratories or lecture halls, but in the silent archives of ancient bones.
Reference: Maria Lopopolo et al, Pre-European contact leprosy in the Americas and its current persistence, Science (2025). DOI: 10.1126/science.adu7144. www.science.org/doi/10.1126/science.adu7144