When we think about cancer treatment, our attention often turns to the tumor itself. Cutting it out, shrinking it with chemotherapy, or attacking it with radiation has long been the frontline approach. Yet, new research suggests that the real key to defeating cancer may lie not just in confronting tumors directly, but in understanding—and protecting—the body’s own immune hubs: the lymph nodes.
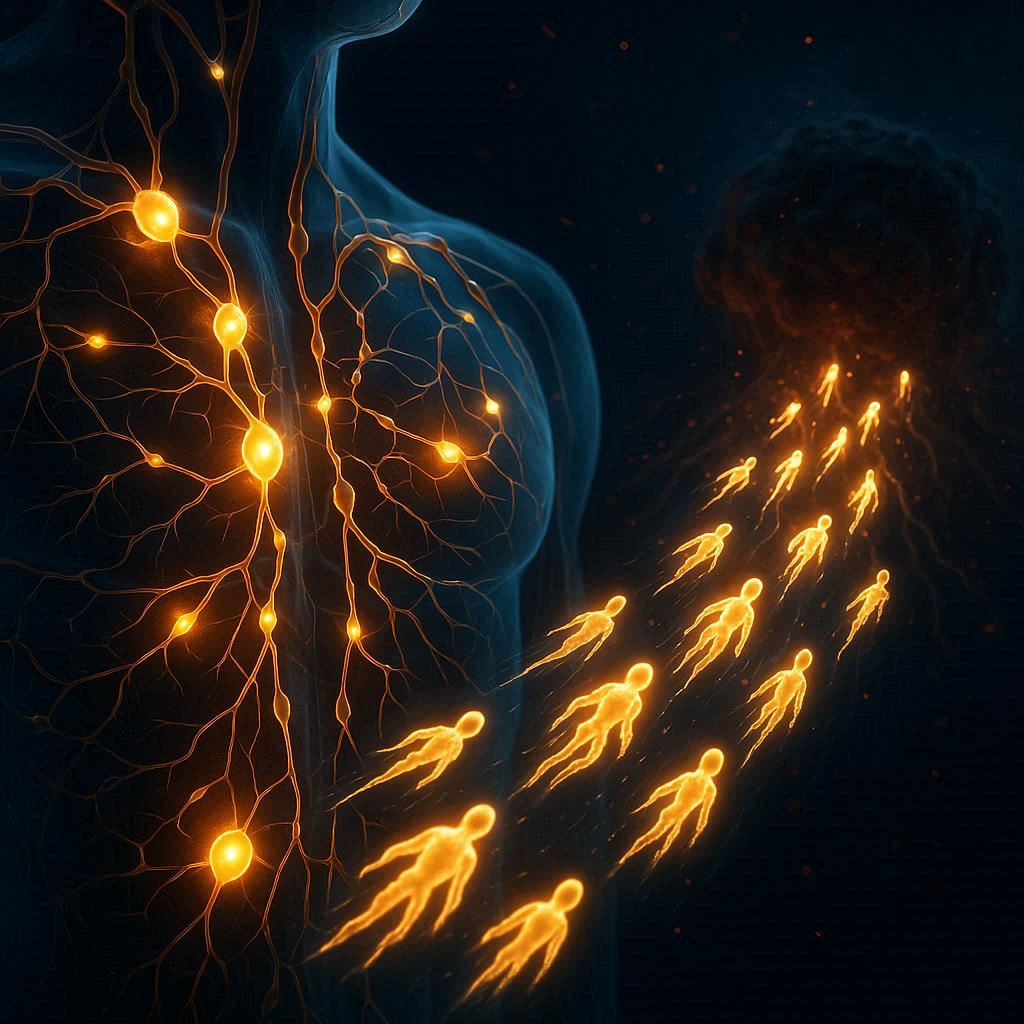
A groundbreaking study from the Peter Doherty Institute for Infection and Immunity (Doherty Institute), published across two papers in Nature Immunology, reveals that lymph nodes play a far more active and crucial role in cancer defense than previously believed. They are not passive checkpoints in the circulatory system. Instead, they are training grounds, schools, and launching pads for the immune system’s most powerful fighters: T cells.
How Lymph Nodes Shape the Fight Against Disease
T cells are a type of white blood cell that form the backbone of our adaptive immune system. Some of them specialize in directly attacking infected or cancerous cells—these are often referred to as “killer” T cells. But the production and maintenance of effective killer cells depend on the presence of a special group of stem-like T cells.
The Doherty Institute team, led by Professor Axel Kallies, discovered that lymph nodes provide the perfect environment for these stem-like T cells to thrive. Within the protective niches of the lymph nodes, these cells are able to survive, multiply, and differentiate into killer cells ready to be dispatched against tumors or chronic infections.
In contrast, when the same immune cells attempt to develop in other immune organs, such as the spleen, they fail to expand effectively. This finding underlines the essential role lymph nodes play—not only as gathering places for immune cells but as vital factories of anti-cancer warriors.
Rethinking Cancer Surgery and Immunotherapy
For decades, surgeons have often removed lymph nodes near tumors to reduce the risk of cancer spreading. While this practice has saved lives, the new research highlights a potential unintended consequence: by removing these immune hubs, we may also be weakening the body’s ability to fight back.
“Lymph nodes aren’t just passive waiting rooms for immune cells,” said Professor Kallies. “They actively train and educate T cells, and send them off to do their job.”
This insight has immediate implications for cancer therapies such as checkpoint inhibitors and CAR T cell therapy—treatments that rely on harnessing the immune system’s own strength. Preserving lymph nodes during surgery could allow patients to generate more robust immune responses, increasing their chances of success with these cutting-edge treatments.
Why Some Patients Respond Better Than Others
One of the greatest mysteries in cancer treatment is why some patients respond extraordinarily well to immunotherapy, while others see little or no effect. The Doherty Institute research provides a possible explanation.
The state and health of lymph nodes directly influence the body’s ability to generate effective killer T cells. If lymph nodes are damaged, missing, or function poorly, the immune system may be unable to mount a strong enough attack against the tumor. In contrast, healthy lymph nodes provide a fertile environment for T cells to flourish, giving patients a much stronger chance of responding to treatment.
Dr. Carlson Tsui, postdoctoral researcher and first author of one of the papers, explained that the team has identified specific molecular signals inside lymph nodes that control how stem-like T cells grow and function. These signals could one day be harnessed in new therapies designed not only to target tumors but also to boost the activity of lymph nodes themselves.
Toward a New Generation of Cancer Therapies
The findings suggest a shift in how we think about cancer treatment. Instead of focusing solely on destroying tumors, doctors may also need to preserve—and even enhance—the patient’s lymph nodes. By doing so, we could unlock the body’s full potential to fight back naturally.
“Rather than only focusing on the tumor itself, therapies should also be designed to preserve and enhance lymph node function,” said Dr. Tsui. “By targeting these critical immune hubs, we could boost the body’s natural ability to fight cancer, increase the effectiveness of existing immunotherapies, and help more patients respond to treatment.”
This new approach could lead to combination strategies where surgery, immunotherapy, and supportive lymph node-targeted treatments work hand in hand. The result could be not only longer survival but also more durable, life-changing responses to treatment.
From Laboratory Discovery to Clinical Impact
While these insights were discovered in animal models, the implications for human health are immense. Professor Shahneen Sandhu, Research Lead for the Melanoma Medical Oncology Service at the Peter MacCallum Cancer Center, emphasized the importance of moving quickly to explore these findings in patients.
“While this research was done in the laboratory with pre-clinical models, we’re excited to study these findings in clinical samples from patients receiving immune checkpoint inhibitors,” she said. “Combining clinical and preclinical studies will help us translate these discoveries from bench to bedside and back, ultimately improving outcomes for cancer patients.”
This bridge between basic science and clinical application is where breakthroughs become treatments, and where laboratory discoveries begin saving lives.
The Hidden Importance of What We Cannot See
Lymph nodes are small, often unnoticed structures scattered throughout the body. To most of us, they only come to mind when swollen during infection. Yet this research reminds us that they are unsung heroes of the immune system—quietly shaping, training, and unleashing the cells that defend us against some of the deadliest diseases known to humanity.
The work of the Doherty Institute team reveals that protecting and supporting these immune hubs could be just as important as targeting tumors directly. Cancer, it seems, cannot be fought on one battlefield alone. It must also be fought in the hidden halls of the lymph nodes, where the body prepares its army for war.
A Future Built on Immune Wisdom
The discovery that lymph nodes are more than passive players changes the way we think about cancer treatment. It opens doors to therapies that don’t just focus on destruction but also on empowerment—strengthening the natural defenses we already carry within us.
For patients, this could mean new hope. For doctors, new strategies. And for science, it represents another step toward understanding the intricate dance between disease and immunity.
The fight against cancer is far from over, but research like this reminds us that progress comes not only from attacking the obvious but also from listening to the quiet, hidden systems of the body. Within the small, resilient nodes of our immune system lies a key to unleashing our greatest defense—and perhaps, one day, defeating cancer itself.
More information: Carlson Tsui et al, Lymph nodes fuel KLF2-dependent effector CD8+ T cell differentiation during chronic infection and checkpoint blockade, Nature Immunology (2025). DOI: 10.1038/s41590-025-02276-7
Sharanya K. M. Wijesinghe et al, Lymph-node-derived stem-like but not tumor-tissue-resident CD8+ T cells fuel anticancer immunity, Nature Immunology (2025). DOI: 10.1038/s41590-025-02219-2