At first glance, the gut and the brain seem like two entirely separate entities. The gut is buried deep in your abdomen, churning food and digesting nutrients. The brain sits high in your skull, commanding your thoughts, emotions, and every beat of your heart. But as science digs deeper into the mysteries of human biology, an astonishing truth has emerged: your gut and brain are in constant, intimate communication. This dynamic relationship is so profound that some scientists now refer to the gut as the “second brain.”
Welcome to the world of the gut-brain axis—a powerful two-way communication network that shapes everything from your mood to your memory, from your decision-making skills to your risk of developing neurological diseases. At the heart of this connection is the microbiome: trillions of bacteria, viruses, fungi, and other microbes that call your digestive tract home. These tiny tenants don’t just help you digest food—they talk to your brain, influence your behavior, and even affect how you think and feel.
In this deep dive, we’ll explore how the gut influences the brain, why gut health is essential for mental well-being, and how you can harness this knowledge to improve your cognitive health and emotional balance. So grab a kombucha or your favorite probiotic yogurt, and let’s journey into the world within.
The Gut-Brain Axis: Your Inner Communication Superhighway
The gut-brain axis is the bidirectional communication system between your gastrointestinal tract and your central nervous system. This complex dialogue is mediated by a mix of neural, hormonal, and immunological signals. In simple terms, your brain talks to your gut—and your gut talks back.
The vagus nerve, one of the largest nerves in your body, is the primary information highway connecting the brain to the gut. This neural superhighway allows the brain to send messages to the gut, regulating digestion, secretion, and immune function. But what’s more surprising is that roughly 80–90% of the nerve fibers in the vagus nerve are afferent, meaning they carry information from the gut to the brain—not the other way around.
This means that your gut is constantly informing your brain about what’s going on inside you. It reports on everything from nutrient levels to the presence of pathogens, but it also conveys information that affects your mood, cognition, and emotional state.
On top of this neural dialogue, your gut also communicates with the brain through hormones (like serotonin and cortisol), immune system molecules (cytokines), and microbial metabolites (like short-chain fatty acids). All these messengers create a rich and dynamic feedback loop between your gut and your brain.
Your Microbiome: The Brain’s Invisible Influencer
Inside your gut lives a bustling metropolis of microbes—bacteria, viruses, fungi, and even archaea—collectively known as the gut microbiome. Each person’s microbiome is as unique as a fingerprint, shaped by factors like birth method, diet, environment, antibiotics, and stress.
These microorganisms are not mere passengers. They play active roles in digestion, vitamin synthesis, immune function, and the regulation of inflammation. But perhaps most astonishingly, they also influence your brain.
Your gut microbes can produce neurotransmitters like serotonin, dopamine, gamma-aminobutyric acid (GABA), and acetylcholine—all of which are crucial for brain function. In fact, more than 90% of the body’s serotonin is produced in the gut, not the brain. This has profound implications for mood and emotional health.
Microbial metabolites like short-chain fatty acids (SCFAs), produced when gut bacteria ferment fiber, can cross the blood-brain barrier and influence brain activity. These SCFAs have been shown to reduce inflammation, protect neurons, and support the integrity of the blood-brain barrier itself.
An imbalance in the microbiome—known as dysbiosis—can disrupt this entire system, leading to inflammation, leaky gut, and changes in neurotransmitter production. This, in turn, may contribute to anxiety, depression, brain fog, and even neurodegenerative diseases like Alzheimer’s and Parkinson’s.
Mental Health Starts in the Gut: Anxiety and Depression
If you’ve ever had butterflies in your stomach before a big presentation, or felt sick with worry during a stressful situation, you’ve experienced the gut-brain connection firsthand. But what science is now uncovering is that your gut doesn’t just react to your emotions—it can generate them.
Numerous studies have shown that people with anxiety and depression often have altered gut microbiomes. These individuals tend to have lower levels of beneficial bacteria like Lactobacillus and Bifidobacterium, and higher levels of potentially harmful microbes. These imbalances may influence how the brain processes stress, how inflammation is regulated, and how mood-related neurotransmitters are produced.
In animal studies, researchers have found that transferring gut bacteria from anxious or depressed mice to healthy mice can induce anxiety and depression-like behaviors in the recipients. Even more strikingly, transplanting healthy microbiomes into anxious mice can reduce their symptoms.
Probiotic supplementation has also shown promise in improving mood and reducing symptoms of depression and anxiety in some human studies. These “psychobiotics” may work by restoring microbial balance, reducing inflammation, and enhancing the production of feel-good neurotransmitters.
The relationship is complex and still under investigation, but the message is clear: caring for your gut may be one of the most effective ways to support your mental health.
The Gut and Cognition: Memory, Focus, and Learning
Your gut microbes don’t just influence how you feel emotionally—they also affect how you think. Emerging research suggests that the microbiome plays a critical role in cognitive processes like memory, learning, and focus.
One way the microbiome influences cognition is through inflammation. Chronic low-grade inflammation, often rooted in poor gut health, is associated with cognitive decline and slower processing speeds. By contrast, a healthy microbiome helps regulate immune responses and reduces the kind of brain inflammation linked to memory loss and neurodegeneration.
Animal studies have shown that manipulating gut bacteria can alter behavior in ways that mirror human cognitive deficits. For example, germ-free mice—raised in sterile environments without any microbes—display impaired memory and reduced neuroplasticity, which is the brain’s ability to form new connections.
Certain probiotics have been shown to improve learning and memory in both animals and humans. Fermented foods rich in beneficial bacteria—like yogurt, kefir, kimchi, and sauerkraut—have been associated with better cognitive performance, although more large-scale human studies are needed.
The connection may also be hormonal. Gut microbes influence the production of brain-derived neurotrophic factor (BDNF), a protein that supports the growth of new neurons and is vital for learning and long-term memory. Low levels of BDNF are linked to cognitive decline, depression, and Alzheimer’s disease.
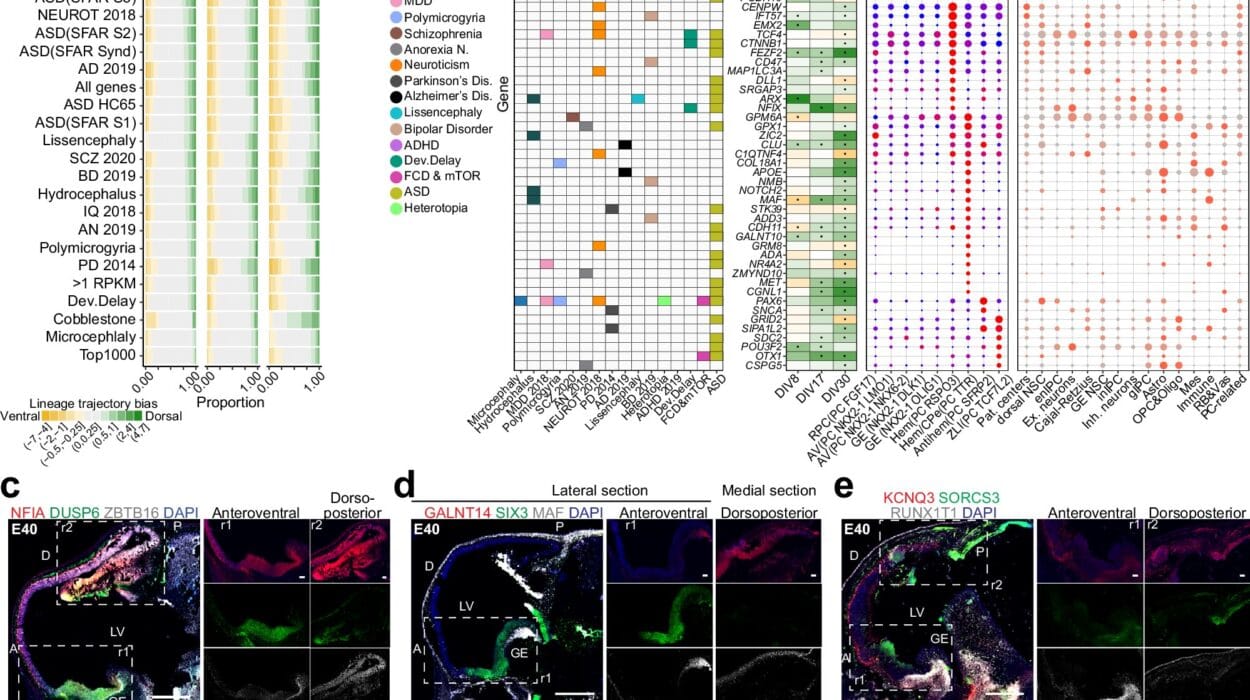
Autism, ADHD, and Neurodevelopmental Disorders
The gut-brain axis has also been implicated in neurodevelopmental conditions like autism spectrum disorder (ASD) and attention-deficit/hyperactivity disorder (ADHD). Many children with these conditions experience gastrointestinal symptoms, and researchers have found significant differences in the microbiomes of affected individuals.
In autism, studies have found altered microbial diversity and increased levels of bacteria that produce pro-inflammatory compounds. These changes may affect brain development, behavior, and sensory processing. Some small studies and clinical trials have shown that improving gut health through probiotics, diet, and even fecal microbiota transplantation (FMT) can lead to improvements in behavior, communication, and gastrointestinal symptoms.
While the science is still evolving, these findings suggest that gut health may play a more critical role in early brain development than previously thought. Understanding and addressing gut imbalances could open up new therapeutic pathways for managing neurodevelopmental disorders.
The Aging Brain and Gut Health
As we age, our gut microbiome undergoes significant changes. Diversity often declines, and beneficial bacteria may be replaced by more inflammatory species. These microbial shifts are thought to contribute to age-related diseases, including cognitive decline and dementia.
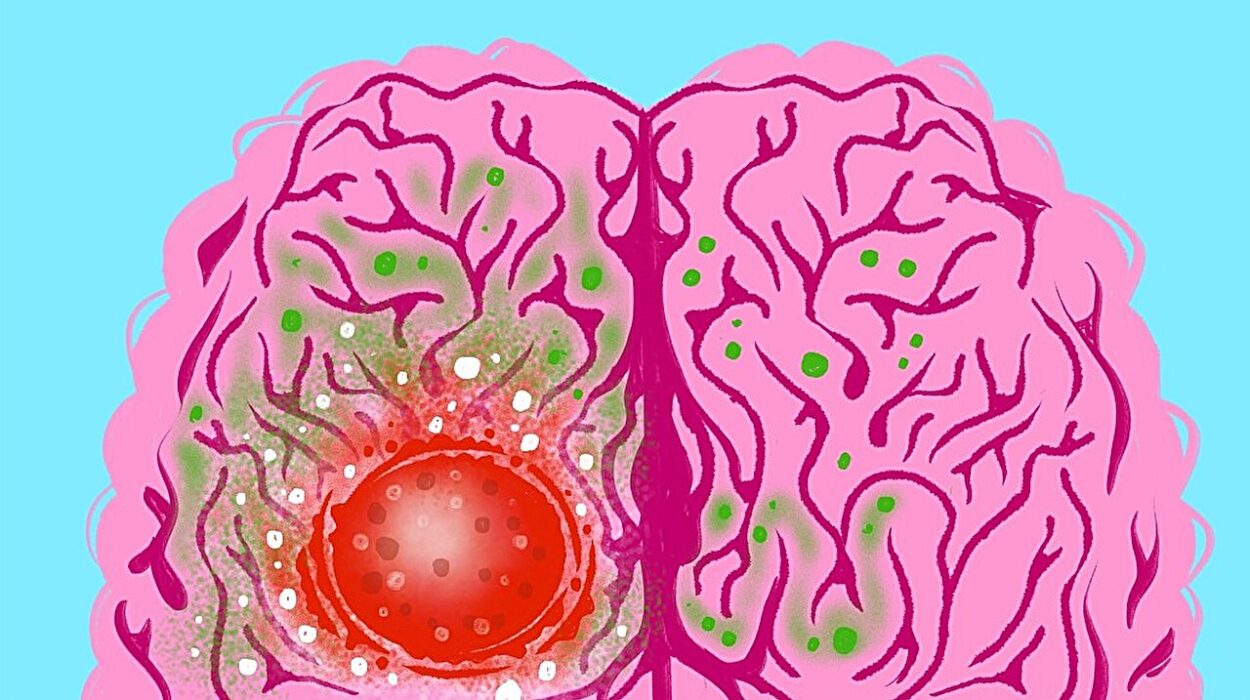
The gut-brain connection becomes even more crucial in old age, as the blood-brain barrier becomes more permeable and inflammation levels tend to rise. A compromised gut can lead to increased systemic inflammation, sometimes called “inflammaging,” which affects brain function and accelerates neurodegeneration.
There is growing interest in using probiotics, prebiotics, and dietary changes to support cognitive function in older adults. Preliminary studies have shown that enhancing gut health can lead to improvements in memory, executive function, and mood among the elderly.
By maintaining a healthy gut microbiome throughout life, we may be able to reduce the risk of Alzheimer’s disease and other forms of dementia, preserving cognitive function well into old age.
What Hurts Your Gut Hurts Your Brain
Modern life isn’t always kind to your gut—and by extension, your brain. A poor diet, high in processed foods and sugar, can lead to inflammation, dysbiosis, and leaky gut syndrome. Chronic stress, lack of sleep, antibiotic overuse, and sedentary lifestyles also wreak havoc on the microbiome.
When the gut barrier becomes permeable—a condition often referred to as “leaky gut”—undigested food particles, toxins, and microbes can escape into the bloodstream. This triggers an immune response and widespread inflammation, which can reach the brain and impair cognitive and emotional functioning.
Inflammation plays a central role in many mental health conditions, including depression, bipolar disorder, and schizophrenia. By reducing gut inflammation, we may be able to alleviate some of the symptoms and underlying mechanisms of these disorders.
The good news is that the gut is remarkably resilient. With the right care, it can often be restored to balance—leading to better brain function and overall health.
Healing Your Gut to Heal Your Mind
So, how do you support your gut to boost your brain? It starts with what you eat. A diet rich in fiber, plant-based foods, fermented products, and healthy fats provides the fuel your microbes need to thrive. Prebiotic fibers found in garlic, onions, leeks, asparagus, and bananas feed beneficial bacteria. Probiotics from yogurt, kefir, and fermented vegetables help repopulate the gut with friendly microbes.
Reducing processed foods, refined sugars, and artificial additives can prevent the growth of harmful bacteria. Drinking plenty of water and engaging in regular physical activity also promote gut motility and microbial diversity.
Managing stress through meditation, deep breathing, or therapy supports the gut-brain axis by reducing cortisol levels and protecting the gut lining. Prioritizing sleep, limiting unnecessary antibiotic use, and spending time in nature—where exposure to diverse environmental microbes helps build resilience—also contribute to a healthier gut and brain.
Some people may benefit from targeted probiotic supplements, but it’s important to remember that there is no one-size-fits-all solution. Your microbiome is unique, and what works for one person may not work for another. A personalized approach, ideally with guidance from a healthcare provider, is best.
The Future of Brain Health Lies in the Gut
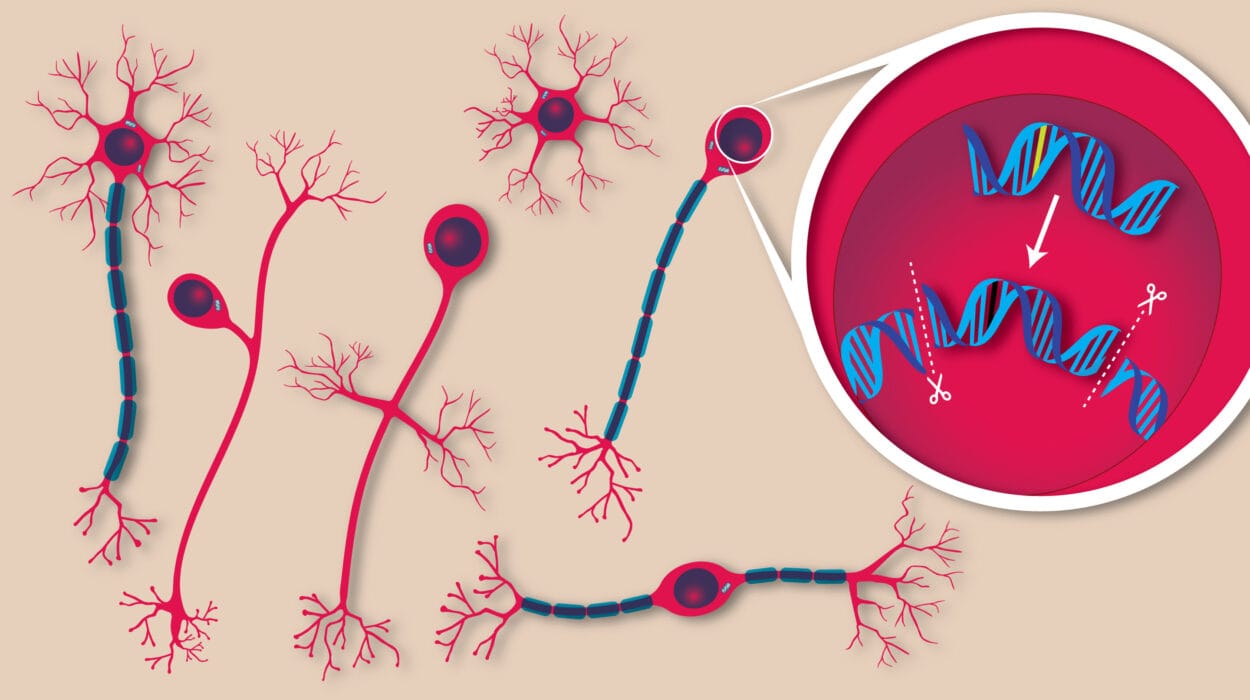
We are on the cusp of a revolution in neuroscience and medicine. As researchers continue to decode the gut-brain axis, we are beginning to see mental health, neurodegeneration, and cognitive function in a whole new light. The idea that treating the gut could ease depression, improve memory, or even prevent Alzheimer’s may once have seemed far-fetched—but today, it’s a serious scientific frontier.
In the years to come, we may see gut-targeted therapies become standard practice in the treatment of psychiatric and neurological disorders. Precision probiotics, tailored diets, microbiome transplants, and even engineered gut bacteria could offer new hope to millions of people worldwide.
But while the science advances, the basic principles remain timeless: eat whole foods, nourish your body, move your muscles, calm your mind, and treat your gut with the care it deserves. Because when your gut thrives, your brain follows.