Emotional trauma is a shadow that lingers long after the triggering event has passed. Unlike physical injuries that can be seen, touched, or X-rayed, emotional wounds are hidden deep within the folds of the brain, affecting thoughts, feelings, and behavior in profound ways. Trauma can stem from a wide range of experiences—abuse, neglect, loss, violence, or even persistent stress—and leaves an imprint that disrupts the delicate balance of the brain’s architecture.
Yet, human beings are not merely victims of their trauma. The brain possesses an incredible capacity to heal, adapt, and grow beyond the scars of emotional injury. This process, complex and nuanced, unfolds over time and involves a remarkable interplay between biology, psychology, and environment.
To grasp how the brain heals from emotional trauma, we first need to understand what trauma does to the brain. Emotional trauma triggers an intense stress response, flooding the brain with chemicals like cortisol and adrenaline. This reaction, meant to protect, can become a source of damage when prolonged or overwhelming. Neural circuits responsible for safety, memory, and emotional regulation become altered. Regions like the amygdala—the brain’s alarm system—grow hyperactive, while the prefrontal cortex, which governs reasoning and impulse control, may weaken.
The effects of trauma ripple through every aspect of a person’s life, influencing relationships, self-esteem, and even physical health. Yet, as daunting as this seems, science reveals the brain is not locked in its trauma-induced state forever. With time, effort, and support, healing is possible. The brain’s plasticity—the ability to reorganize and form new connections—underlies this capacity for recovery.
The Brain’s Architecture Under Siege
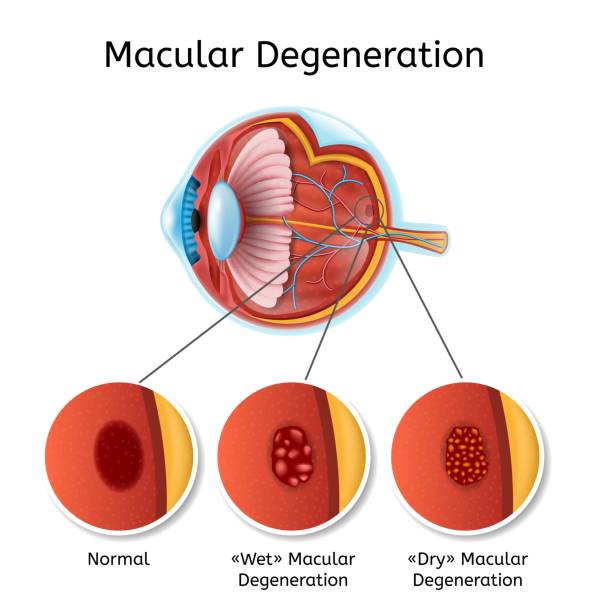
The trauma response is rooted in ancient brain structures that evolved to protect us from danger. The amygdala detects threats and triggers the fight, flight, or freeze response. The hippocampus processes memories and context, while the prefrontal cortex enables thoughtful decision-making and emotional regulation.
When trauma strikes, the amygdala lights up like a wildfire, flooding the system with stress hormones that prepare the body for immediate survival. While essential in the moment, chronic activation of this alarm system can impair the hippocampus, which struggles to distinguish between safe and threatening memories. This results in fragmented, intrusive memories that replay uncontrollably—a hallmark of post-traumatic stress disorder (PTSD).
Meanwhile, the prefrontal cortex, which helps modulate emotional reactions, can become less effective under chronic stress. This reduces the brain’s ability to “put the brakes on” the amygdala’s alarms. The result is a brain stuck in a loop of fear and hypervigilance, unable to relax or fully process traumatic memories.
Structural changes in these regions have been observed in neuroimaging studies of trauma survivors. The hippocampus is often smaller, the amygdala hyperactive, and prefrontal activity diminished. This rewiring reflects the deep imprint trauma leaves on the brain’s architecture.
The Power of Neuroplasticity: Rebuilding the Brain
Despite the profound effects trauma can have, the brain is not fixed. Neuroplasticity—the brain’s ability to change its structure and function in response to experience—is the foundation of healing. This remarkable capacity allows neurons to grow new connections, reorganize networks, and even generate new brain cells in certain areas like the hippocampus.
Healing begins when the brain learns to regulate its stress response. Therapies aimed at trauma recovery focus on calming the amygdala and strengthening the prefrontal cortex’s control. This rebalancing enables individuals to move from a state of survival to one of safety and integration.
Neuroplasticity also explains why repeated experiences can reinforce new neural pathways. Positive experiences, safe relationships, and supportive environments help the brain form healthier circuits that counteract trauma’s effects. Conversely, without intervention, negative patterns can become entrenched.
Importantly, healing is not about erasing memories of trauma but transforming their meaning and impact. Through neuroplastic change, traumatic memories become integrated into a coherent narrative, reducing their emotional charge and empowering individuals to reclaim their lives.
The Role of Memory: From Fragmentation to Integration
One of the most painful aspects of emotional trauma is the nature of traumatic memories. Unlike ordinary memories, which are stored in a coherent, accessible way, traumatic memories often become fragmented and disconnected. This disorganization arises because stress hormones disrupt the hippocampus during trauma encoding, impairing the brain’s ability to form a clear timeline or context.
As a result, trauma survivors may experience flashbacks, nightmares, or intrusive thoughts—sensory fragments of the event that feel as immediate and raw as the original experience. This fragmentation traps the brain in a loop of re-experiencing, preventing healing.
Healing the brain means reorganizing these memories. Through therapeutic approaches such as trauma-focused cognitive behavioral therapy (CBT), eye movement desensitization and reprocessing (EMDR), and narrative therapy, survivors can revisit their traumatic memories in a safe environment. This process encourages the hippocampus to contextualize memories, linking them to time and place and reducing their power to provoke fear.
The integration of traumatic memories transforms them from overwhelming emotional triggers into manageable parts of a person’s life story. The brain learns to store these memories in the same way it stores ordinary experiences, enabling emotional regulation and cognitive clarity.
The Neurochemistry of Healing: Rebalancing Stress Hormones
The biochemical environment of the brain plays a critical role in trauma and recovery. During trauma, stress hormones like cortisol surge, activating survival pathways but also suppressing systems related to growth, repair, and learning. Prolonged exposure to these hormones damages neurons, particularly in the hippocampus, and alters neurotransmitter systems that regulate mood and anxiety.
Healing involves restoring balance to this neurochemical landscape. Studies show that effective trauma therapy can normalize cortisol levels and improve neurotransmitter function. For example, serotonin and dopamine systems, essential for mood regulation and reward, are often dysregulated by trauma but can be recalibrated through therapy, medication, and lifestyle changes.
Additionally, oxytocin—a hormone associated with bonding and trust—plays a surprising role in trauma recovery. Positive social interactions boost oxytocin release, which in turn dampens the amygdala’s reactivity and promotes feelings of safety. This biochemical feedback loop highlights the importance of relationships in healing emotional wounds.
The Body-Mind Connection: Somatic Healing of Trauma
Trauma is not just stored in the brain but also in the body. The nervous system, muscles, and organs retain imprints of trauma through chronic tension, altered breathing patterns, and heightened physiological arousal. This somatic residue can perpetuate anxiety, pain, and emotional distress even when conscious memories are inaccessible.
Healing trauma, therefore, requires more than cognitive insight—it demands reconnecting the body and mind. Somatic therapies, such as sensorimotor psychotherapy, trauma-sensitive yoga, and the Feldenkrais method, focus on releasing physical tension and re-regulating the autonomic nervous system.
These therapies work by helping individuals become aware of bodily sensations linked to trauma and gently re-pattern their responses. As the nervous system shifts from sympathetic dominance (fight or flight) to parasympathetic activation (rest and digest), the brain receives signals that it is safe, supporting emotional regulation and healing.
This body-centered approach recognizes that trauma is a full-body experience and that healing must integrate all aspects of the self.
The Healing Power of Relationships
No brain heals in isolation. Human beings are wired for connection, and relationships are the soil in which the brain’s healing can flourish or falter. The presence of a safe, attuned caregiver or supportive community provides the external regulation needed to repair internal dysregulation caused by trauma.
Attachment theory explains how early relationships shape the brain’s capacity for trust, emotion regulation, and resilience. For trauma survivors, re-experiencing secure attachment through therapy or supportive bonds can reverse some of the damage caused by neglect or abuse.
Social support reduces stress hormones, increases oxytocin, and promotes neurogenesis—the growth of new brain cells—particularly in the hippocampus. These biological effects underscore why healing trauma often requires rebuilding trust and connection.
Moreover, therapeutic relationships act as corrective emotional experiences, where survivors learn they can be seen, heard, and valued without judgment. This relational safety is essential for accessing and processing traumatic memories, promoting neuroplasticity, and nurturing growth.
The Role of Mindfulness and Meditation in Brain Healing
Mindfulness and meditation have emerged as powerful tools for trauma recovery. These practices cultivate present-moment awareness and nonjudgmental acceptance of thoughts, emotions, and bodily sensations. This stance counters trauma’s tendency to trap individuals in the past or in overwhelming emotional states.
Neuroscientific studies show that mindfulness meditation alters brain function and structure in ways that support healing. Regular practice increases activity in the prefrontal cortex, enhancing executive control over the amygdala and reducing reactivity to stress. It also boosts connectivity between brain regions involved in self-regulation and emotional processing.
Mindfulness helps survivors observe traumatic memories or triggers without becoming overwhelmed, allowing for gradual desensitization and integration. Furthermore, it promotes self-compassion, reducing shame and self-blame that often accompany trauma.
The growing scientific evidence supporting mindfulness’s benefits has led to its incorporation into many trauma therapies, offering a non-invasive, accessible path to brain healing.
The Journey of Healing: Patience, Persistence, and Hope
Healing from emotional trauma is neither linear nor quick. The brain’s rewiring takes time, and setbacks are common. Some days may feel like progress, while others reveal lingering shadows. This journey requires patience, persistence, and often courage to face pain rather than avoid it.
It’s important to recognize that healing does not mean forgetting or erasing trauma but reclaiming power over one’s life. The brain’s plasticity offers hope that even deeply ingrained wounds can be transformed. With the right support, tools, and environments, survivors can build resilience, restore safety, and find meaning beyond their suffering.
Modern science continues to deepen our understanding of how the brain heals, guiding more effective therapies and empowering individuals to take an active role in their recovery. The path is unique for each person but always grounded in the timeless human capacity to heal.