Addiction is often spoken about as a moral failing, a lack of willpower, or simply a bad habit. But beneath these misconceptions lies a far more complex and profound story—one written in the circuitry of the brain itself. Addiction is a chronic brain disorder that hijacks the neural systems governing reward, motivation, and self-control. It is a battle fought deep inside the mind, where chemicals and neurons orchestrate behaviors that feel impossible to resist. To truly grasp addiction, we must venture beyond judgment and into the intricate dance of biology and experience that transforms desire into compulsion.
The Brain’s Reward System: Nature’s Motivational Engine
At the heart of addiction lies the brain’s reward system—a complex network designed by evolution to reinforce behaviors essential for survival. Eating, socializing, reproducing—these activities activate this system, releasing chemicals that make us feel pleasure and encourage us to repeat them. This system is built around the neurotransmitter dopamine, often called the brain’s “feel-good” messenger.
When dopamine floods certain regions, particularly the nucleus accumbens and the ventral tegmental area (VTA), it signals that something important and positive is happening. This flood reinforces the behavior, making us want to seek it out again. It’s a finely tuned mechanism that ensures survival by motivating us to eat nourishing food or bond with others.
Yet, this system is vulnerable. Drugs, alcohol, and even certain behaviors can stimulate dopamine release far beyond natural levels. The brain interprets these surges as extraordinary events, assigning them outsized importance. This initial flood is seductive—a chemical promise of euphoria that the brain craves to relive.
Hijacking the Brain: How Addiction Begins
When a person first uses an addictive substance, their brain’s reward circuitry is hit with an intense rush of dopamine. The experience is often intensely pleasurable—whether it’s the rush of heroin, the buzz of alcohol, the high of nicotine, or the thrill of gambling. This surge rewires the brain’s priorities. The substance or behavior becomes a “super-reward,” overshadowing natural incentives like food or social connection.
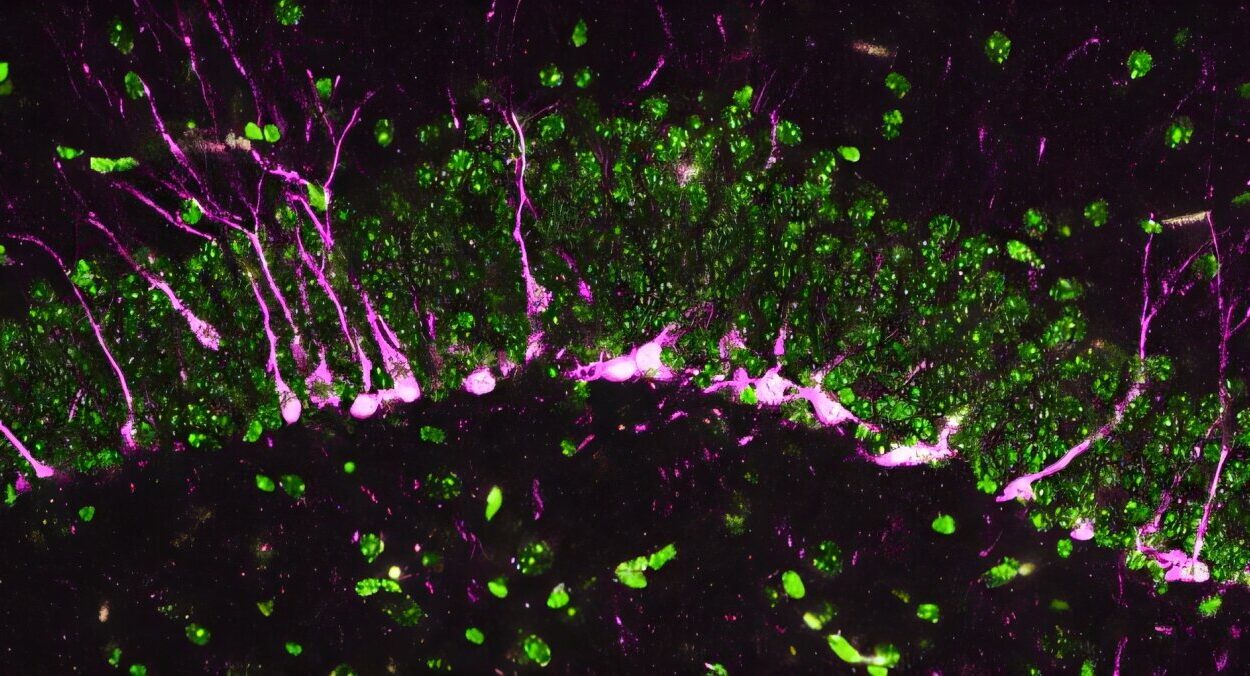
With repeated exposure, the brain begins to adapt. It reduces the number of dopamine receptors or their sensitivity in an effort to maintain balance—a phenomenon known as downregulation. What this means for the individual is a diminishing ability to feel pleasure from everyday activities. The world becomes dull, colorless, and uninspiring. Only the drug or addictive behavior can temporarily fill the void.
This neurochemical transformation is the seed of addiction, where the voluntary pursuit of pleasure gradually morphs into an uncontrollable compulsion.
The Prefrontal Cortex: When Decision-Making Goes Awry
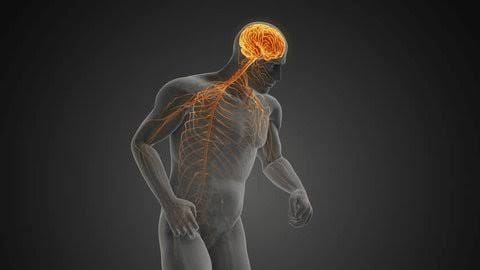
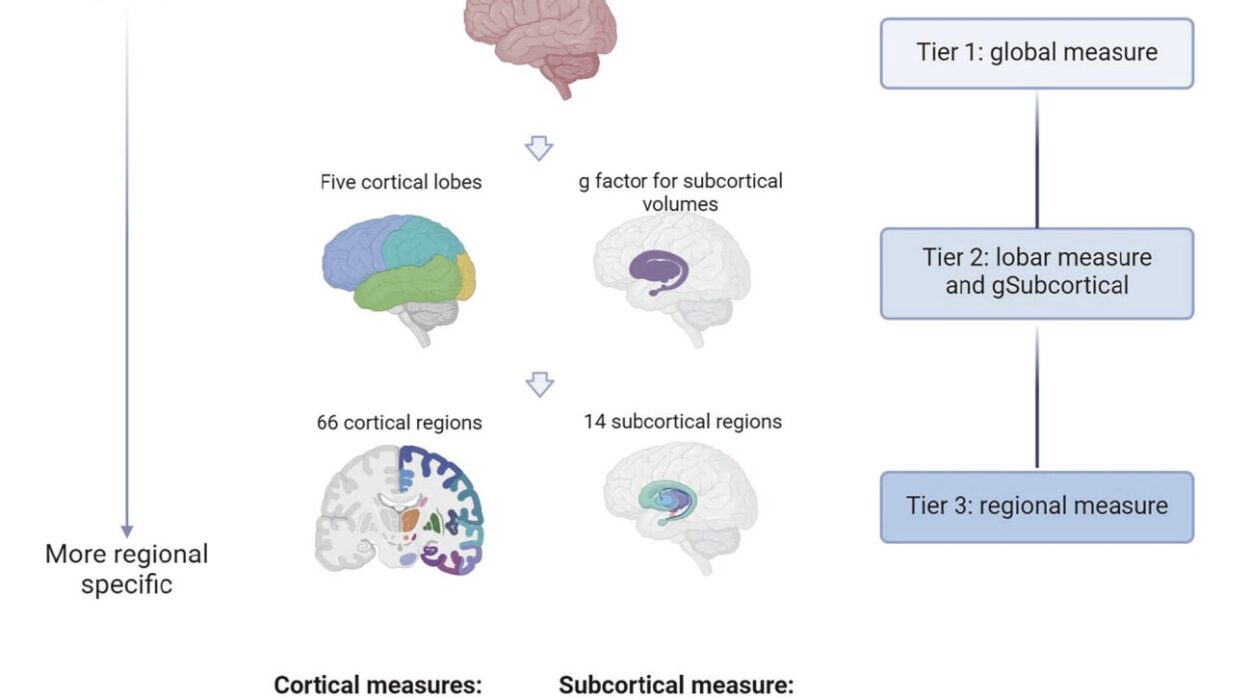
While dopamine-driven reward circuits fuel craving, the brain’s prefrontal cortex—the region responsible for judgment, decision-making, and impulse control—plays a critical role in addiction. In a healthy brain, this region acts as a brake, helping us evaluate consequences and resist short-term temptations for long-term gains.
Addiction disrupts this balance. Chronic drug use impairs the prefrontal cortex’s ability to regulate impulses and exert self-control. Studies using brain imaging reveal decreased activity and structural changes in this area among addicted individuals. The result is a weakening of willpower and an erosion of the capacity to weigh risks realistically.
This dysfunction explains why addiction often leads to decisions that seem irrational or self-destructive. The brain is no longer simply seeking pleasure; it is trapped in a cycle where desire overwhelms judgment.
The Role of Memory and Learning: Addiction as a Learned Behavior
Addiction is not merely about pleasure and compulsion—it also deeply involves the brain’s memory and learning systems. The hippocampus and amygdala, regions critical for forming memories and emotional responses, become entwined with the reward circuitry.
When a person experiences the pleasure of drug use, the brain encodes not just the sensation but the context—the sights, sounds, people, and emotions present. These cues become powerful triggers, capable of eliciting cravings long after the drug has left the body. A certain smell, a street corner, or even a mood can ignite the desire to use again, setting the stage for relapse.
This powerful association reflects how addiction is a learned behavior deeply embedded in the brain’s neural fabric, making recovery a continuous struggle against both biology and environment.
Stress, Emotion, and Addiction: The Brain’s Vulnerability
Addiction doesn’t occur in a vacuum. Emotional stress plays a crucial role in vulnerability and relapse. The brain’s stress response system, involving the hypothalamic-pituitary-adrenal (HPA) axis, interacts closely with addiction pathways.
Chronic stress releases cortisol, a hormone that can alter brain function and structure. In people vulnerable to addiction, stress heightens craving and weakens self-control by further impairing the prefrontal cortex. Emotional distress becomes both a trigger and a consequence of addiction, creating a vicious cycle.
Moreover, addiction alters the brain’s reward threshold, making it harder for natural rewards to soothe stress or produce pleasure. This double bind can deepen dependence, as the substance or behavior becomes the only perceived escape.
The Genetics of Addiction: Nature Meets Nurture
While environment and experience shape addiction, genetics also plays a significant role. Twin and family studies estimate that genetic factors contribute between 40 and 60 percent of the risk for developing addiction. Genes influence how the brain processes dopamine, how sensitive it is to stress, and how substances are metabolized.
For example, variations in genes regulating dopamine receptors can affect the intensity of reward from drugs. Some people have a genetic makeup that makes their brains more vulnerable to the hijacking effects of addictive substances.
However, genetics is not destiny. It interacts dynamically with life experiences. Early trauma, social environment, and mental health conditions all weave together with biology to determine the course of addiction.
Neuroplasticity: The Brain’s Double-Edged Sword
The brain is remarkably plastic, capable of rewiring itself in response to experience—a process called neuroplasticity. This ability is essential for learning, memory, and adaptation. But in addiction, neuroplasticity becomes a double-edged sword.
Repeated drug use strengthens certain neural pathways associated with craving and compulsive behavior, making these patterns more entrenched and automatic. At the same time, pathways involved in self-control and natural reward diminish.
Yet, neuroplasticity also offers hope. The brain’s wiring can be reshaped through recovery efforts, therapy, and changes in behavior. New synapses form, and brain function can improve over time, demonstrating that addiction is not an irreversible fate.
The Complexity of Withdrawal: The Brain’s Demand for Balance
When an addicted person stops using a drug, they often face withdrawal—a collection of physical and psychological symptoms caused by the brain’s adjustment to the absence of the substance. Withdrawal reflects the brain’s demand for balance and the profound changes addiction has wrought.
For example, the downregulated dopamine system struggles to function without the drug’s artificial boost, resulting in feelings of depression, anhedonia (inability to feel pleasure), and intense cravings. The brain’s stress systems may become hyperactive, producing anxiety, irritability, and physical discomfort.
Withdrawal symptoms vary widely depending on the substance but always represent the brain’s effort to restore equilibrium. This painful phase is a major hurdle to recovery, as it tempts many back to use to alleviate distress.
Beyond the Brain: Addiction’s Impact on the Whole Person
Though rooted in brain biology, addiction’s consequences ripple outward, affecting every aspect of a person’s life. Emotional turmoil, damaged relationships, social isolation, and physical health problems all intertwine with neural dysfunction. The stigma surrounding addiction adds further wounds, fostering shame and preventing many from seeking help.
Understanding the brain mechanisms behind addiction allows us to see beyond blame and opens the door to empathy and effective treatment. It reveals addiction as a disease—a disorder of brain circuits that requires comprehensive approaches to healing.
Modern Treatments: Healing the Addicted Brain
The science of addiction has guided the development of treatments that address its biological and psychological dimensions. Medications such as methadone and buprenorphine for opioid addiction work by stabilizing brain chemistry and reducing cravings. Other drugs target neurotransmitter systems to ease withdrawal or block the effects of substances.
Behavioral therapies, like cognitive-behavioral therapy (CBT) and contingency management, retrain the brain’s response to triggers and strengthen self-control. Mindfulness and stress-reduction techniques help repair the brain’s stress systems and improve emotional regulation.
Importantly, effective treatment recognizes addiction as a chronic condition. Relapse is common but does not signal failure—it is part of the brain’s ongoing struggle to rewire itself.
The Future: Neuroscience’s Promise and the Battle Ahead
As neuroscience advances, new frontiers in understanding and treating addiction emerge. Brain imaging technologies allow unprecedented glimpses into addiction’s neural networks. Emerging therapies, such as transcranial magnetic stimulation and deep brain stimulation, hold promise for directly modulating brain activity.
Genetic research offers potential for personalized medicine, tailoring treatments to individuals’ biological profiles. Meanwhile, public health approaches emphasize prevention, early intervention, and addressing social determinants of addiction.
Yet, the battle against addiction remains daunting. It demands compassion, science, and a recognition that addiction is not a failure of character but a struggle within the delicate, powerful organ that defines our humanity—the brain.