Every day, millions of people around the world swallow pills, receive injections, or apply creams—each one containing a substance designed to treat a disease, relieve pain, or support the body’s natural functions. Yet few stop to consider what actually happens when medicine enters the body. What path does it take? How does it “know” where to go? And why do some drugs work for some people but not others?
Understanding how medicines work is not just the realm of doctors and scientists—it’s a story about chemistry, biology, and the incredible complexity of the human body. It’s a story about molecules and messengers, locks and keys, risks and benefits. This scientific overview will take you deep into the fascinating journey a drug makes from ingestion to effect, breaking down complex processes into engaging insights you can understand without a medical degree.
What Is a Medicine?
At its core, a medicine—also called a drug—is a chemical substance that interacts with the body’s biological systems to produce a specific therapeutic effect. Medicines can cure diseases, alleviate symptoms, manage chronic conditions, or even prevent illness.
Medicines can be:
- Synthetic (manufactured in laboratories)
- Semi-synthetic (modified from natural sources)
- Natural (derived from plants, animals, or minerals)
- Biologic (produced from living organisms like bacteria or cells)
From a scientific standpoint, a medicine isn’t simply “good” or “bad.” It’s a powerful tool—like a scalpel, it can heal when used properly or harm if misused. That’s why understanding how it works inside the body is critical for both safety and effectiveness.
The Journey Begins: How Medicines Enter the Body
Before a medicine can do anything, it has to get into your system. This is called drug administration, and there are several routes:
- Oral (swallowed): The most common method.
- Topical (applied to skin or mucous membranes): For local effects.
- Inhalation (breathed in): Often used for respiratory diseases.
- Injection (intravenous, intramuscular, or subcutaneous): Fastest route.
- Transdermal (absorbed through skin): Delivers drug over time.
Each route affects how quickly and efficiently the drug is absorbed. For instance, intravenous injection sends the drug directly into the bloodstream for rapid action, while oral drugs must navigate the acidic stomach and complex digestive system first.
Absorption: Crossing Into the Body’s Inner World
Once inside, a drug must cross biological barriers to enter the bloodstream—the body’s superhighway. This process is called absorption.
Most drugs are absorbed through the small intestine, whose inner surface is covered in microscopic finger-like projections called villi. These increase surface area and enhance the transfer of drug molecules from the gut into the blood.
The rate and efficiency of absorption depend on several factors:
- Solubility: Fat-soluble drugs pass through cell membranes more easily.
- pH: Some drugs are better absorbed in acidic or alkaline environments.
- Formulation: Tablets, capsules, liquids, and time-release coatings affect how quickly a drug dissolves.
Once a drug molecule crosses the gut lining and enters the bloodstream, it’s no longer just a pill—it’s now an active participant in a molecular drama.
Distribution: The Bloodstream Highway
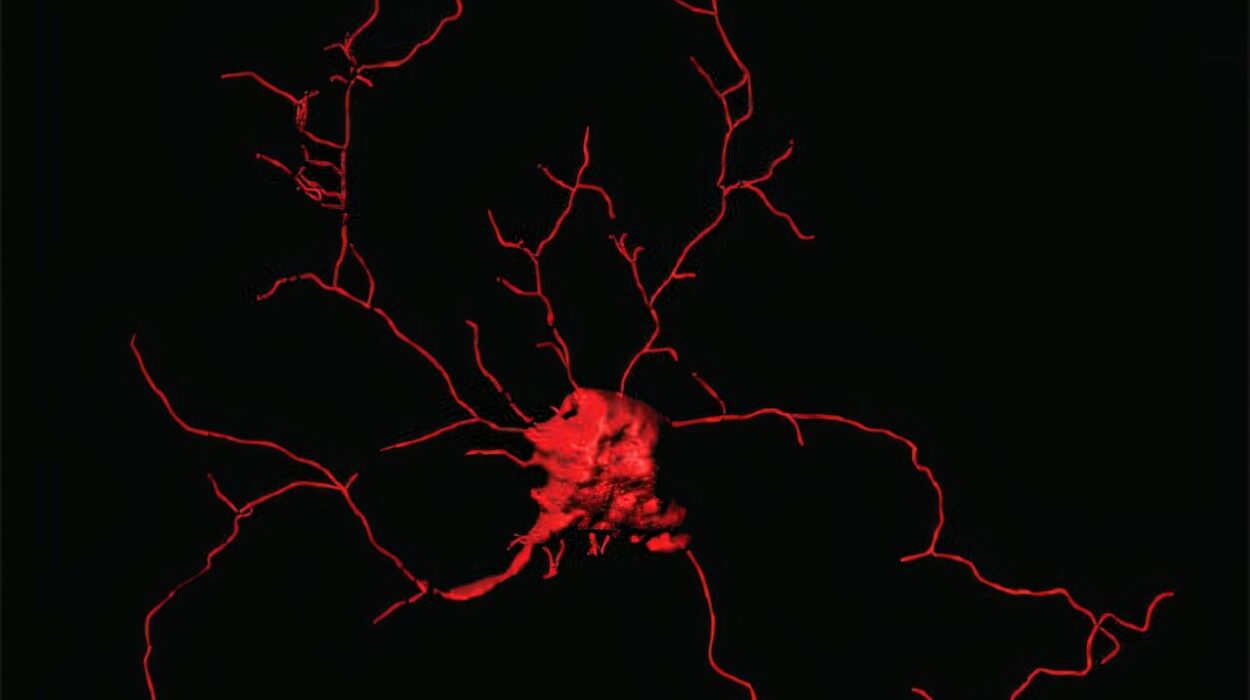
Now in circulation, the drug must reach its site of action—the specific cells, tissues, or organs it is designed to affect. This is the process of distribution.
However, the bloodstream is not an open road; it’s more like a crowded city with toll gates, traffic jams, and detours. Several factors influence distribution:
- Blood flow: Highly perfused organs like the brain, liver, and kidneys get more of the drug, faster.
- Plasma protein binding: Some drugs latch onto proteins like albumin in the blood. While bound, they’re inactive.
- Fat and water solubility: Fat-soluble drugs may accumulate in fatty tissue, creating reservoirs.
One of the most important distribution challenges is the blood-brain barrier (BBB). This tightly packed layer of cells protects the brain from toxins—but also keeps many drugs out. Only small, fat-soluble molecules or those with specific transport mechanisms can cross it.
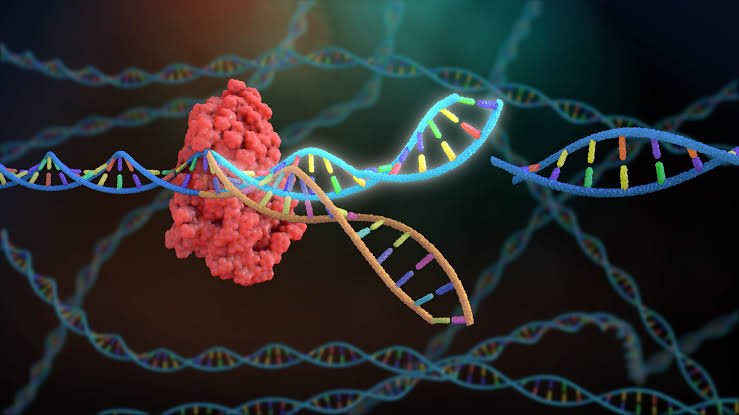
The Target: How Drugs Interact with the Body
Once a drug reaches its target tissue, it must interact with cellular structures to exert its effect. This is where the famous “lock-and-key” model comes in.
Receptors: The Locks
Cells have receptors—specialized protein molecules usually located on their surfaces or within their cytoplasm. These act like molecular locks, waiting for the right key. When the drug (the key) binds to the receptor (the lock), it triggers a specific response inside the cell.
Some drugs activate receptors. These are called agonists. For example, morphine activates opioid receptors to reduce pain.
Others block receptors. These are antagonists. For example, antihistamines block histamine receptors to reduce allergy symptoms.
Enzymes and Ion Channels
Not all drugs act on receptors. Some inhibit enzymes, like how aspirin blocks cyclooxygenase (COX) enzymes to reduce inflammation. Others affect ion channels, altering the flow of sodium, potassium, or calcium ions in and out of cells—essential in treating arrhythmias or epilepsy.
Still others may alter gene expression, bind to DNA, or change cell membrane fluidity.
Every drug action is a result of complex biochemical signaling—and even a small molecule can create massive downstream effects.
Metabolism: The Body’s Drug Processing Plant
After a drug does its job, the body needs to get rid of it. But before excretion, most drugs undergo metabolism, primarily in the liver.
The liver contains enzymes—particularly from the cytochrome P450 family—that chemically alter drug molecules. These changes usually make drugs:
- More water-soluble (so they can be excreted)
- Less active (detoxified)
However, metabolism can sometimes activate a drug instead. These are called prodrugs. For example, codeine is metabolized into morphine, which is the active painkiller.
Drug metabolism is affected by:
- Genetics: Some people metabolize drugs faster or slower.
- Age: Liver function varies across the lifespan.
- Diet and other drugs: Grapefruit juice, for example, can inhibit liver enzymes and raise drug levels dangerously.
Metabolism is why some drugs must be taken multiple times a day—once they’re broken down, their effect fades.
Excretion: Clearing the Body
After metabolism, the drug (or its byproducts) must be eliminated. This happens through excretion, primarily via the kidneys (in urine) or liver (in bile and feces).
The rate of excretion determines how long a drug stays in your system—its half-life. A short half-life means the drug leaves quickly; a long half-life means it lingers, sometimes building up to toxic levels if not managed.
Some drugs are also excreted through:
- Lungs (like alcohol or anesthetics)
- Sweat and saliva
- Breast milk (important for nursing mothers)
The entire process—from ingestion to excretion—can take minutes or days, depending on the drug.
The Role of Dosage
One of the most critical aspects of medicine is dosage. Too little, and the drug won’t be effective. Too much, and it could be toxic. The ideal dose is called the therapeutic dose—high enough to work, but low enough to avoid harmful side effects.
Pharmacologists use something called the therapeutic window—the range between the minimum effective concentration and the minimum toxic concentration. Narrow windows require careful monitoring, like with warfarin or lithium.
Side Effects: The Unintended Effects
No drug is perfect. Side effects—unintended consequences of a drug’s action—are common and sometimes unavoidable.
They may occur because:
- The drug affects multiple types of receptors.
- It reaches tissues beyond the target.
- The body responds in unpredictable ways.
For example, antihistamines may reduce allergy symptoms but also cause drowsiness by crossing into the brain and blocking receptors there.
Side effects range from mild (nausea, dry mouth) to severe (organ damage, allergic reactions). That’s why clinical trials and post-marketing surveillance are crucial to understanding a drug’s full impact.
Why Drugs Work Differently in Different People
A pill that cures one person’s headache might do nothing—or even harm—another. Why?
The answer lies in individual variation.
- Genetics: Variations in enzymes, receptors, or transport proteins affect drug response.
- Age: Infants and elderly people often process drugs differently.
- Sex: Hormonal differences influence metabolism and side effect profiles.
- Body weight and composition: Fat-soluble drugs distribute differently in heavier people.
- Health status: Liver or kidney disease alters metabolism and excretion.
- Interactions: Other drugs, foods, and supplements can change how a drug works.
This is the foundation of personalized medicine—an emerging field that tailors drug therapy to individual biology, using genetic testing and other biomarkers.
Vaccines: Special Medicines With Long-Term Impact
Vaccines are a special class of medicine. Instead of treating disease, they prevent it by training the immune system to recognize and attack specific pathogens.
Vaccines typically contain:
- Inactivated viruses
- Weakened (attenuated) viruses
- Fragments of bacteria or viruses
- Messenger RNA (mRNA) in newer vaccines
Once administered, the body generates antibodies and memory cells—creating immunity without causing illness. Vaccines have transformed public health, eradicating or reducing diseases like polio, measles, and smallpox.
Antibiotics: The Battle Against Bacteria
Antibiotics deserve their own section because of their profound impact. These medicines specifically target bacteria, either killing them (bactericidal) or stopping their growth (bacteriostatic).
They work by:
- Disrupting bacterial cell walls (penicillin)
- Inhibiting protein synthesis (tetracyclines)
- Blocking DNA replication (quinolones)
However, antibiotics don’t affect viruses. Overuse or misuse can lead to resistance, where bacteria evolve defenses against the drugs—posing a major threat to global health.
Hormones and Biologics: Mimicking Nature
Some drugs are hormone-based, replacing or modifying natural signaling molecules. Examples include insulin (for diabetes), estrogen (in hormone therapy), or thyroid hormones.
Biologics are larger, more complex molecules—like monoclonal antibodies—that target specific components of the immune system or cancer cells. Because they’re made from living organisms, they’re more difficult to produce but can be incredibly precise.
Biologics are transforming treatment for diseases like rheumatoid arthritis, psoriasis, and certain cancers.
Drug Development: From Idea to Pharmacy Shelf
The journey from concept to market is long and complex. Drug development follows several stages:
- Discovery: Identifying potential molecules through lab research or natural products.
- Preclinical testing: Testing on cells and animals for safety and biological activity.
- Clinical trials: Human testing in phases (1 for safety, 2 for efficacy, 3 for comparison).
- Approval: Regulatory agencies (like FDA) evaluate the data.
- Post-marketing surveillance: Ongoing monitoring for rare side effects.
On average, it takes 10–15 years and over a billion dollars to develop a new drug. Most candidates fail along the way.
Conclusion: The Dance Between Chemistry and Life
Medicines are miracles of modern science. They are also reminders of just how complex and finely tuned the human body is. Every pill swallowed, every injection given, every patch applied represents years of research, thousands of molecular interactions, and a precise balance between benefit and risk.
Understanding how medicines work—from absorption and distribution to action and elimination—empowers us to make better decisions, ask smarter questions, and appreciate the science behind the scenes. It’s a dance between chemistry and life—one that continues to evolve with every scientific breakthrough.
As personalized medicine, gene editing, and nanotechnology reshape the future of healthcare, one thing remains constant: the fundamental principle that every drug, no matter how small, must find its way through the vast, intricate network of the human body to fulfill its purpose.
And that, perhaps, is the greatest journey of all.