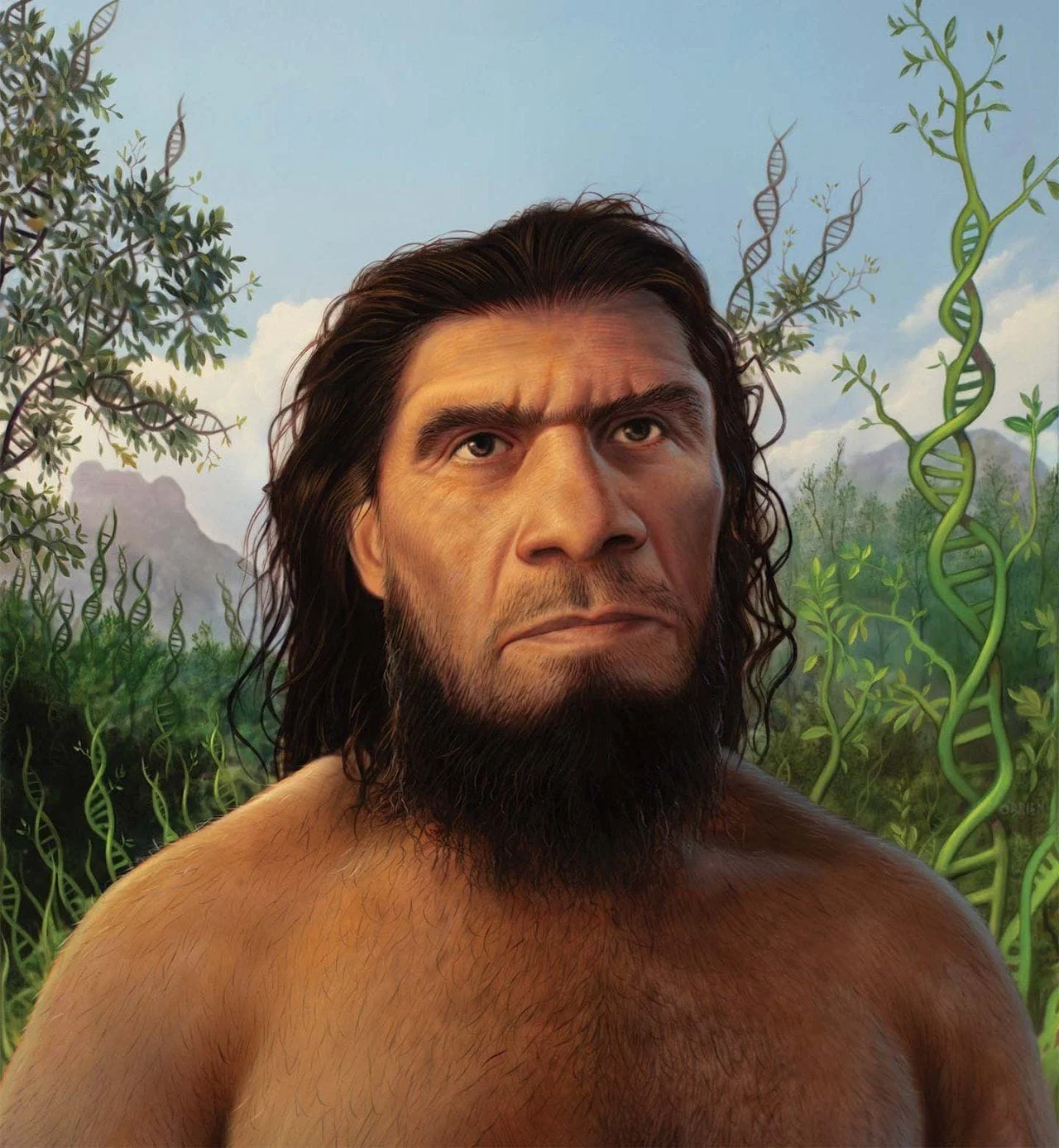
The story of human evolution is not just one of adaptation to climate, landscape, or food. It is also the story of an eternal war—a war fought silently, invisibly, and without pause. Disease, in all its forms, has stalked humanity from its earliest beginnings. Long before the first Homo sapiens walked the African savannas, parasites were already evolving alongside our ancestors. Pathogens have been more than mere adversaries; they have been sculptors, chiseling away at our genes, rewiring our immune systems, and even influencing the structure of our societies. While wars and empires may dominate the pages of history books, disease has shaped the very biology of the human species.
Life and Death in the Pleistocene
The earliest humans did not live long. Fossil records show that the average lifespan of a Homo erectus or even early Homo sapiens was often under 30 years. While predators, injuries, and starvation took many lives, disease was always lurking in the background. Long before agriculture or cities existed, hunter-gatherers encountered parasites from contaminated water, suffered wounds that led to infections, and endured periodic outbreaks of viral or bacterial illnesses passed between close-knit groups.
Yet in those times, disease dynamics were different. Small populations meant that epidemics could not sustain themselves for long. A deadly virus might burn through a band of foragers and die out with them. Pathogens that relied on human-to-human transmission had a harder time surviving unless they caused long-term, chronic infections. This favored slower, more insidious diseases, like tuberculosis or leprosy, which could lie dormant or persist in hosts for years.
These early threats began to exert evolutionary pressure. Human immune systems became more sophisticated, adapting to recognize a broader range of invaders. Genes that offered some resistance to common diseases began to spread. Even blood types may have evolved in response to pathogens; the differences between type A, B, AB, and O are not random—they may reflect ancient battles between humans and microbes.
The Agricultural Revolution and the Rise of Epidemics
The real transformation in disease dynamics came with the Neolithic Revolution. Around 10,000 years ago, humans began to settle into agricultural communities. They domesticated plants and animals, built permanent homes, and formed denser populations. These changes brought many benefits: stable food supplies, the birth of civilization, and the rise of complex societies. But they also invited a new kind of danger—epidemic disease.
Farming communities lived closer together, in proximity to both each other and their animals. This created perfect conditions for zoonotic diseases—illnesses that jump from animals to humans. Smallpox, measles, influenza, and many others are believed to have originated in domesticated animals. Once these diseases took hold in human populations, they could spread rapidly and become endemic.
For the first time, humans were exposed to plagues that could wipe out large portions of entire populations. And evolution responded. Those who survived left behind genes that made them more resistant, creating selective pressure that forever altered the human genome.
One of the most famous examples is the CCR5-Δ32 mutation, a genetic variant that confers resistance to HIV. It is especially common in European populations, and while HIV is a modern disease, the mutation likely became widespread during earlier epidemics—possibly smallpox or the Black Death. Individuals with two copies of the mutation are largely immune to HIV infection, and those with one copy have a delayed progression to AIDS. This is a textbook case of how past disease outbreaks shaped future immunity.
The Black Death: A Turning Point in European Genetics
In the 14th century, the Black Death tore through Europe, killing an estimated 30 to 60 percent of the population in just a few years. Caused by the bacterium Yersinia pestis and transmitted by fleas, the plague was more than just a catastrophe—it was an evolutionary bottleneck.
Mass mortality meant that only the most resistant individuals survived. Recent genetic studies have shown that the plague selected for specific variants of immune-related genes in Europe, especially in the HLA (human leukocyte antigen) system. These genes play a critical role in recognizing pathogens. Certain HLA variants that were rare before the plague became more common afterward, suggesting that the Black Death had exerted immense selective pressure on the European gene pool.
But this survival came at a cost. The same genetic variants that helped protect against the plague may also increase the risk of autoimmune diseases, like Crohn’s disease or rheumatoid arthritis. Evolution is a balancing act, and what protects us in one era may harm us in another.
Malaria and the Global Impact of a Tiny Parasite
Malaria has been one of the deadliest diseases in human history, and its effects on evolution are among the best understood. Caused by Plasmodium parasites and spread by mosquitoes, malaria has likely killed more humans than any other infectious disease.
In regions where malaria is common—especially sub-Saharan Africa—evolution has selected for several genetic mutations that provide some protection. One is the sickle cell trait. Individuals who inherit one copy of the sickle cell gene (heterozygotes) have red blood cells that are less hospitable to the malaria parasite. This gives them a survival advantage in malaria-prone regions. However, those who inherit two copies (homozygotes) develop sickle cell disease, a painful and often deadly condition.
This tragic trade-off is a powerful example of “balancing selection” in evolution. A harmful gene can be maintained in a population if it provides a survival benefit in carriers. Similar evolutionary adaptations have occurred elsewhere. The thalassemia gene, prevalent in Mediterranean populations, and the Duffy-negative blood type in West Africa, are other responses to the relentless pressure of malaria.
These mutations are etched into the genomes of entire populations, reflecting a long and bloody history of survival.
Smallpox and the Shaping of Immunity
Smallpox, caused by the Variola virus, has been one of humanity’s oldest and deadliest enemies. Its distinctive pockmarked scars are found on mummies from ancient Egypt, and historical records show it repeatedly decimated populations over thousands of years.
In Europe, smallpox outbreaks occurred frequently from the medieval period onward. Over time, repeated exposure likely drove genetic selection for greater resistance. Survivors passed on traits that strengthened the immune system. Like the CCR5 mutation mentioned earlier, other less-understood variants may have helped Europeans resist not just smallpox, but other viral threats as well.
The role of smallpox in colonial history cannot be overstated. When European colonizers arrived in the Americas, they brought with them a host of diseases to which Indigenous populations had no previous exposure. Smallpox alone killed tens of millions, causing societal collapse in many regions. The deaths were not due to weakness, but to evolutionary mismatch—Native populations had never encountered these pathogens before, and their immune systems were unprepared.
This tragic episode is another reminder of how disease acts not just on individuals, but on entire cultures and civilizations. Evolution, too, is not confined to biology—it shapes the fates of nations.
Cholera, Typhoid, and the Battle of Urbanization
As cities grew during the Industrial Revolution, new evolutionary pressures emerged. Overcrowded, unsanitary urban environments gave rise to outbreaks of cholera, typhoid, and dysentery. These diseases, transmitted through contaminated water, turned thriving cities into death traps.
Natural selection, again, came into play. Those with genes for more robust immune responses, or with gut microbiomes that could better handle bacterial invaders, were more likely to survive.
Moreover, the need for collective hygiene triggered a form of cultural evolution. The development of public health systems, water filtration, and sanitation infrastructure became critical not just for survival, but for economic and societal advancement. In this way, disease didn’t just change our bodies—it reshaped our behavior and built the modern world.
HIV and Contemporary Evolution in Real Time
The HIV/AIDS pandemic, beginning in the late 20th century, has provided a rare opportunity to observe human evolution as it happens. Unlike many past plagues, HIV does not kill immediately. It integrates into the host’s DNA and can remain dormant for years. Its slow but devastating progression allows for complex evolutionary interactions.
Some individuals have natural resistance, like those with the CCR5-Δ32 mutation. Others, called “elite controllers,” are infected but do not progress to AIDS, suggesting the presence of unique immune responses. Studies of these individuals are helping researchers identify genetic factors that could be the future of HIV treatment—or even a cure.
What’s more, HIV has exerted evolutionary pressure not just biologically but behaviorally. It has reshaped sexual practices, public health messaging, and international cooperation in fighting disease.
The Microbiome Revolution
One of the most exciting areas of evolutionary medicine today involves the human microbiome—the trillions of bacteria, viruses, and fungi that live in and on our bodies. These microscopic companions are not just passive stowaways; they are active participants in our health, immunity, and even mood regulation.
Over thousands of years, our microbiomes have co-evolved with us, influenced by diet, environment, and exposure to disease. Antibiotics and modern hygiene have altered this relationship dramatically in the last century. Some scientists believe that changes in our microbiome may be contributing to rising rates of autoimmune disease, allergies, and even obesity.
In a very real sense, evolution is still happening—not just to our genes, but to the complex ecosystems within us.
The Evolutionary Cost of Survival
Surviving disease often comes at a price. Genetic mutations that once offered protection may now be maladaptive. For example, the same inflammatory responses that helped early humans survive infections can contribute to chronic diseases today. Autoimmune disorders, asthma, and allergies may all stem from an immune system that evolved in a world full of parasites and pathogens—but now has too little to fight.
This is part of what evolutionary biologists call the “mismatch hypothesis.” Our bodies evolved in a very different environment than the one we now inhabit. The genes we carry were selected for conditions that no longer exist, and the result is a rise in “diseases of civilization.”
Understanding this mismatch is critical for modern medicine. It forces us to view disease not just as something to eliminate, but as something to understand in context. Evolution, after all, does not strive for perfection—only survival.
Looking Ahead: Evolution in the Age of Biotechnology
Today, humanity stands at a strange crossroads. For the first time in history, we are not merely responding to evolution—we are guiding it. With vaccines, antibiotics, and gene-editing technologies like CRISPR, we have begun to take control of the evolutionary process. We are engineering immunity, altering DNA, and manipulating the very forces that once acted blindly upon us.
But nature is not passive. Pathogens evolve too. Antibiotic-resistant bacteria are on the rise. New viruses, like SARS-CoV-2, remind us that evolution never sleeps. The battle between humans and disease is not over—it is simply entering a new phase.
Perhaps the greatest challenge is to use our understanding of evolution wisely. We must consider the long-term consequences of our choices. We must remember that every medical advance creates new pressures, new adaptations, and new risks.
In this new era, disease will continue to shape us—not just through natural selection, but through the decisions we make, the technologies we wield, and the responsibilities we bear.
Conclusion: The Hand That Shaped Us
Disease has been humanity’s most persistent companion, our deadliest foe, and, paradoxically, one of our greatest teachers. It has exposed our vulnerabilities and refined our strengths. It has guided our biology, shaped our societies, and carved its signature into our DNA.
Every cough, every fever, every pandemic carries echoes of the past—of ancestors who suffered, adapted, and survived. In their blood runs the story of evolution, written not in ink, but in immune cells and silent genes.
To understand ourselves, we must understand disease. For in the shadows of sickness, we find the outlines of our shared humanity—resilient, adaptive, and ever evolving.