Hot flashes are one of the most well-known—and often misunderstood—symptoms of menopause. For many women, they come out of nowhere like a flash of internal fire, surging heat through the body, reddening the skin, and leaving behind a sheen of sweat and a wave of discomfort. These episodes can strike during meetings, while cooking dinner, or in the dead of night, disrupting sleep and sapping energy. But what exactly are hot flashes? Why do they happen, and most importantly, how can they be managed?
The experience of hot flashes can feel anything but subtle. Some women describe it as standing in front of a furnace, others liken it to being suddenly drenched in heat from the inside out. Yet despite how common they are, the exact cause of hot flashes remains only partially understood. What we do know is that they’re strongly tied to hormonal changes—particularly the fluctuations and eventual decline of estrogen during perimenopause and menopause.
The Science Behind the Sizzle
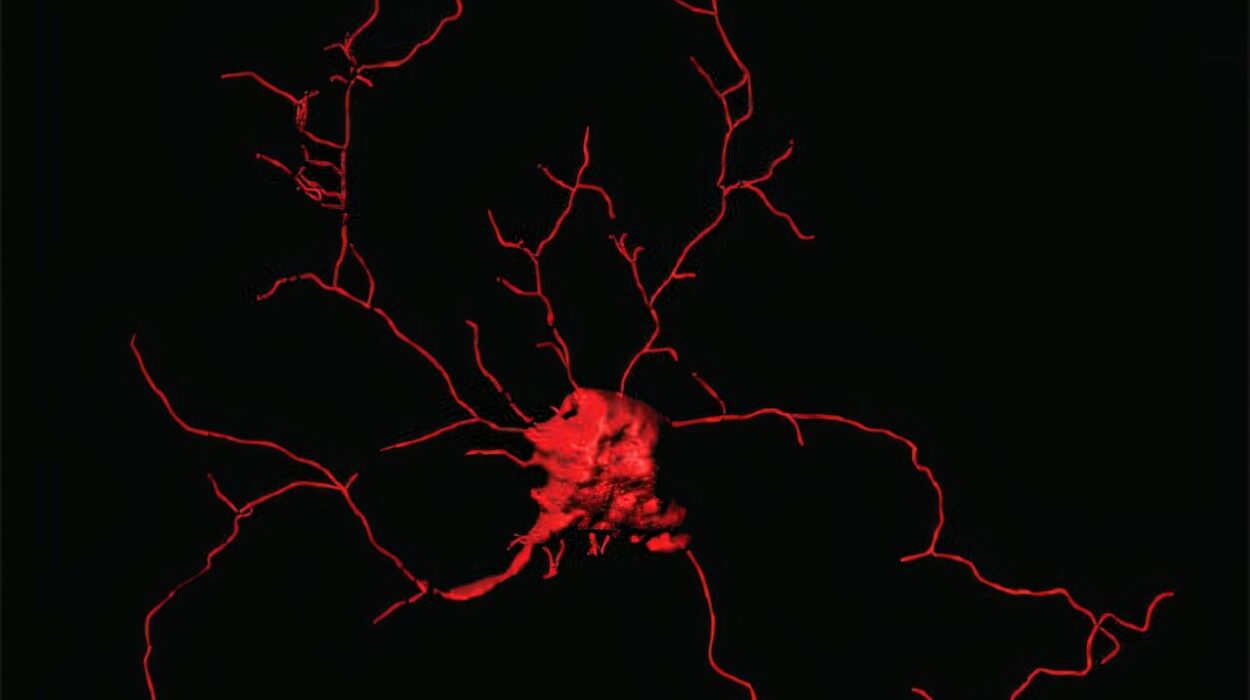
To grasp why hot flashes occur, it helps to look at the role of estrogen in the female body. Estrogen is more than just a reproductive hormone. It also affects the brain, heart, bones, and even body temperature. One of its many jobs is to help regulate the hypothalamus, the part of the brain responsible for controlling internal temperature.
During menopause, when estrogen levels begin to drop, the hypothalamus becomes more sensitive to slight changes in body temperature. Think of it like a thermostat gone haywire. Even a minor increase in temperature can trigger the hypothalamus to overreact, setting off a cascade of events designed to cool the body down. Blood vessels dilate to release heat, sweat glands go into overdrive, and a hot flash is born.
This process doesn’t always happen quietly. For some, a hot flash lasts only a few seconds; for others, it can stretch to several minutes. The frequency varies wildly—some women experience multiple episodes a day, while others might have just a few per month. The severity, too, can differ from a gentle warmth to a full-body inferno followed by chills and fatigue.
The Menopausal Connection
Hot flashes are most commonly associated with the transition to menopause, the time when a woman’s menstrual cycles gradually cease. This transition, known as perimenopause, can begin as early as a woman’s late 30s or early 40s and last several years. It’s during this phase that hormones start fluctuating unpredictably, creating the perfect storm for hot flashes and other symptoms like mood swings, insomnia, and night sweats.
While menopause is defined as 12 consecutive months without a period, the symptoms don’t necessarily stop once that milestone is reached. In fact, hot flashes can persist into postmenopause, sometimes continuing for a decade or longer.
What’s especially frustrating is the unpredictability. There’s no set timeline, no countdown clock that signals when the hot flashes will start—or when they’ll stop. Genetics, lifestyle, and overall health all play a role in determining the experience.
Night Sweats: The After-Dark Cousin of Hot Flashes
When hot flashes strike during sleep, they’re often referred to as night sweats. These nighttime episodes can be particularly disruptive, drenching pajamas and sheets, causing frequent awakenings, and leading to chronic sleep deprivation. Women who suffer from regular night sweats often wake up feeling as though they’ve run a marathon rather than gotten a restful night’s sleep.
This lack of restorative sleep can compound other menopausal symptoms. It can exacerbate mood swings, impair memory and focus, and lower the immune response. Over time, chronic sleep disturbance can even increase the risk of depression and cardiovascular problems.
Addressing night sweats often requires a two-pronged approach: managing the symptoms directly and improving sleep hygiene overall. But before jumping into solutions, it’s important to understand the various triggers that can amplify hot flashes and night sweats.
Triggers That Fan the Flames
While hormone fluctuations are the main culprits behind hot flashes, certain behaviors and environmental factors can act as triggers, making episodes more frequent or intense. Spicy foods, for example, can turn a mild hot flash into a fiery inferno. Caffeine and alcohol are also frequent offenders, stimulating the nervous system and causing the blood vessels to expand.
Stress is another major factor. When you’re anxious or emotionally overwhelmed, your body releases adrenaline and cortisol—hormones that can interfere with temperature regulation and set off hot flashes. It’s not uncommon for women to notice more frequent episodes during periods of high emotional stress or after a particularly busy day.
Hot environments, like a crowded room or a hot bath, can also provoke symptoms. Even tight clothing or synthetic fabrics that don’t breathe can contribute. And then there’s smoking, which not only exacerbates hot flashes but also speeds up the onset of menopause itself.
Understanding these triggers is a crucial step in managing symptoms. What affects one woman might not bother another, so keeping a journal to identify personal patterns can be incredibly helpful.
Natural Relief and Lifestyle Strategies
Many women prefer to try natural remedies before turning to medication. This makes sense, especially given the growing interest in holistic wellness and the desire to avoid potential side effects of pharmaceuticals. Fortunately, there are several lifestyle strategies and home-based remedies that can significantly reduce the frequency and severity of hot flashes.
Diet plays a powerful role. Eating more plant-based foods, particularly those rich in phytoestrogens—natural compounds that mimic estrogen—may help regulate hormonal fluctuations. Foods like soy, flaxseeds, chickpeas, and lentils contain these compounds and have been linked to reduced menopausal symptoms in some studies.
Hydration is another essential piece. Drinking plenty of cool water throughout the day can help regulate body temperature and prevent overheating. Wearing breathable clothing and dressing in layers can also make a big difference, allowing you to peel off items as needed when a hot flash strikes.
Exercise, too, offers multiple benefits. Regular physical activity helps balance hormone levels, reduce stress, and improve sleep quality. Activities like yoga and tai chi not only support physical health but also teach breathing techniques and mindfulness practices that can be used in the heat of a hot flash.
Mind-body techniques such as meditation, deep breathing, and progressive muscle relaxation can calm the nervous system and lower the intensity of an episode. These techniques help the body remain in a parasympathetic—or relaxed—state, rather than the hyper-aroused state that triggers hot flashes.
The Role of Hormone Replacement Therapy (HRT)
For some women, lifestyle changes alone aren’t enough. When hot flashes become severely disruptive, hormone replacement therapy (HRT) can offer relief. HRT involves supplementing the body with estrogen, often in combination with progesterone, to replace what the ovaries are no longer producing.
Studies have shown that HRT is highly effective in reducing hot flashes, sometimes eliminating them entirely. It can also help with other symptoms of menopause, such as vaginal dryness, bone loss, and mood changes. However, HRT is not without risks. Long-term use has been linked to an increased risk of breast cancer, stroke, and blood clots in some women, particularly if started many years after menopause.
Because of these risks, HRT is typically recommended at the lowest effective dose for the shortest possible duration. Decisions around hormone therapy are deeply personal and should be made in consultation with a healthcare provider who can assess individual risks and benefits.
There are also newer, lower-dose formulations and non-hormonal medications that can offer relief, such as certain antidepressants, anticonvulsants, and blood pressure drugs that have been shown to reduce the frequency and severity of hot flashes in some women.
Exploring Alternative and Complementary Therapies
Beyond lifestyle changes and hormone therapy, many women explore alternative remedies for managing hot flashes. Acupuncture has been studied for its effects on menopausal symptoms, with some women reporting significant improvement. The theory is that acupuncture may influence neurotransmitters involved in temperature regulation and hormone production.
Herbal supplements like black cohosh, red clover, dong quai, and evening primrose oil have also been widely used, although scientific evidence on their effectiveness remains mixed. Some women find relief, while others notice no change or experience unwanted side effects. As with any supplement, it’s important to consult a healthcare professional before starting, especially if you’re taking other medications or have underlying health conditions.
There’s also a growing interest in CBD and medical cannabis for symptom relief, particularly for sleep issues and anxiety, though research is still in its early stages. While anecdotal reports are promising, more clinical studies are needed to establish safety and efficacy.
The Emotional and Psychological Side of Hot Flashes
Hot flashes don’t just affect the body—they can take a significant emotional toll as well. Feeling constantly overheated and uncomfortable can lead to frustration, embarrassment, and even social withdrawal. Night sweats that rob women of sleep can heighten irritability and reduce the ability to cope with everyday stress.
What’s more, hot flashes often hit during a time of life when many women are already navigating major changes: aging parents, career transitions, or empty nests. The combination of physical discomfort and emotional upheaval can feel overwhelming.
That’s why emotional support and open dialogue are so important. Talking to friends or joining a menopause support group can reduce the sense of isolation and help women share strategies that work. Therapy or counseling may be helpful for those experiencing depression or anxiety, and mindfulness practices can teach women how to accept and ride the wave of symptoms rather than resist them.
Menopause in a Modern Context
The conversation around menopause and hot flashes is evolving. Once a taboo topic, it’s now being discussed more openly in media, healthcare, and society at large. Celebrities, authors, and physicians are speaking out about their own experiences, pushing for better research, better treatment options, and greater awareness.
And this matters—because despite how common hot flashes are, they’re still under-treated and often dismissed. Women are frequently told to “tough it out,” but that approach fails to recognize how disruptive these symptoms can be. Just because menopause is natural doesn’t mean women should suffer in silence.
Empowering women with accurate information and access to care is key. Menopause is not a disease, but it is a significant physiological transition, and hot flashes are its most visible—and visceral—symptom. With the right support, women can navigate this chapter with confidence and resilience.
Hope on the Horizon
Research into menopause is advancing. Scientists are developing new medications that target hot flashes more precisely, including non-hormonal options that affect the brain’s temperature-regulating centers. Precision medicine—tailoring treatment based on a woman’s unique genetics, environment, and lifestyle—is becoming a reality.
Wearable tech is also being developed to track hot flash patterns and predict episodes, giving women better tools for managing symptoms in real-time. Cooling clothing, smart bedding, and home temperature-control systems are already making life more comfortable for many.
Perhaps most importantly, the cultural tide is turning. Menopause is being reframed not as an ending, but as a powerful transformation—a time to refocus on health, purpose, and personal well-being. With awareness and innovation growing, the future looks a lot cooler.
Conclusion: Finding Your Cooling Path
Every woman’s experience of hot flashes is unique. Some breeze through menopause with only a few fleeting episodes, while others grapple with years of unpredictable heat, drenched sheets, and fatigue. There is no one-size-fits-all solution—but there are many tools to explore.
From lifestyle changes and dietary tweaks to hormone therapy and emerging treatments, relief is possible. The key is to stay curious, stay informed, and advocate for your own health. Don’t be afraid to talk about your symptoms, ask questions, or seek second opinions.
Hot flashes may be part of the menopausal journey, but they don’t have to define it. With the right knowledge and support, women can step into this new chapter with strength, grace—and a fan, just in case.