For millions of people across the world, pain is not just a fleeting sensation but a constant, uninvited companion. Chronic pain affects more than 1.5 billion people globally. Its grip often goes beyond the body, weaving itself into the fabric of the mind, where depression and anxiety deepen its sting. The result is a vicious cycle: pain worsens mood, poor mood magnifies pain, and the spiral continues, draining vitality and hope.
For decades, the medical system has tried to manage this suffering with opioids, anti-inflammatories, and antidepressants. Yet too often, these treatments come with heavy costs—addiction, dependency, and incomplete relief. But a recent study from the Perelman School of Medicine at the University of Pennsylvania offers a new kind of possibility. Researchers there have uncovered how psilocybin—the active compound in certain psychedelic mushrooms—interacts with specific brain circuits. Their findings, published in Nature Neuroscience, may open the door to an era of non-opioid, non-addictive therapies for managing pain and its emotional burden.
Breaking the Cycle of Pain and Mood
Dr. Joseph Cichon, anesthesiologist, neuroscientist, and senior author of the study, has seen firsthand how chronic pain and depression intertwine. “In many cases,” he explains, “patients aren’t even sure which came first. But what they do know is that one always makes the other worse.”
This is what makes psilocybin so intriguing. Unlike typical pain medications that target the site of injury, psilocybin works at the level of the brain, shifting the way pain signals are processed and, at the same time, lifting mood. It doesn’t silence the body’s warning systems altogether; instead, it gently retunes them. The metaphor researchers use is a dimmer switch rather than an on-off button. Psilocybin modulates key serotonin receptors—5-HT2A and 5-HT1A—adjusting the brain’s internal rhythms instead of bludgeoning them into silence.
In mouse studies, a single dose of psilocybin significantly reduced both chronic pain and the anxiety- or depression-like behaviors that pain often fuels. Remarkably, these benefits lasted nearly two weeks, far longer than most conventional treatments.
Targeting the Brain’s Pain–Emotion Hub
The Penn team wanted to go deeper: where in the nervous system was this relief coming from? To find out, they injected psilocin—the metabolized form of psilocybin—into specific regions of the brain and spinal cord.
The results were striking. When psilocin was directed into the prefrontal cortex, and more precisely into the anterior cingulate cortex (ACC)—a region known to regulate both pain and emotions—the same relief appeared as with whole-body psilocybin. But when psilocin was injected into the spinal cord, there was no comparable effect.
This suggests that psilocybin’s power lies not in numbing signals at the site of pain but in rebalancing the brain’s perception of pain itself. It eases the distressing emotional component of pain, offering relief that is both physical and psychological.
“Psilocybin may offer meaningful relief for patients by bypassing the site of injury altogether,” Cichon explains. “Instead, it modulates brain circuits that process pain while simultaneously lifting those that regulate mood.”
A Window Into the Brain’s Inner Symphony
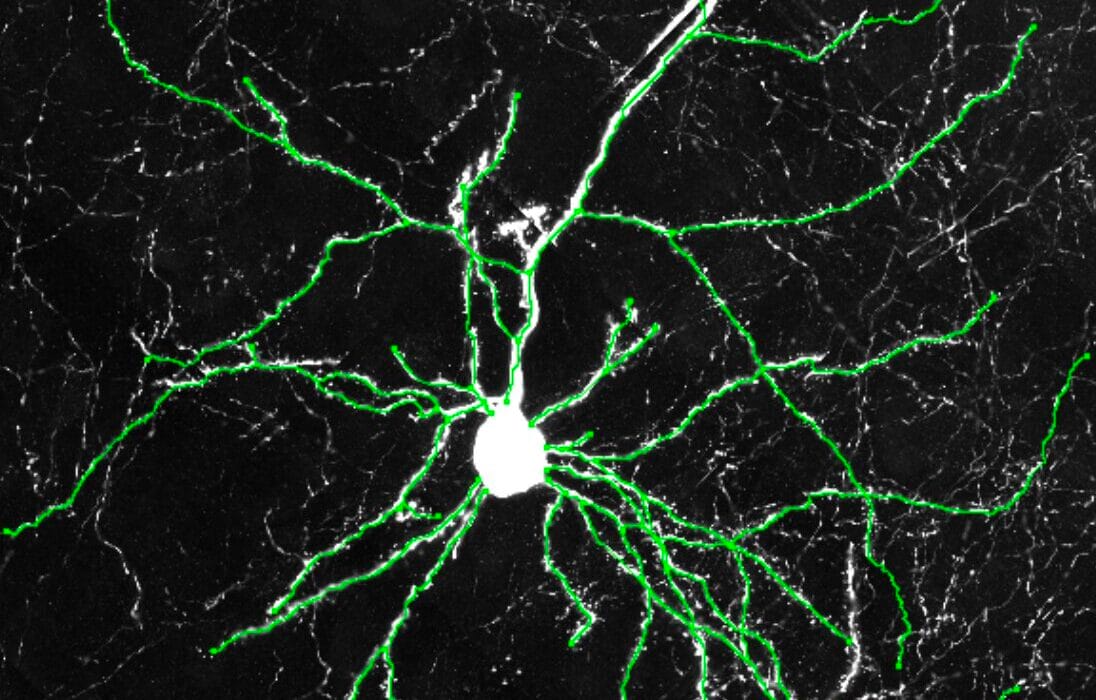
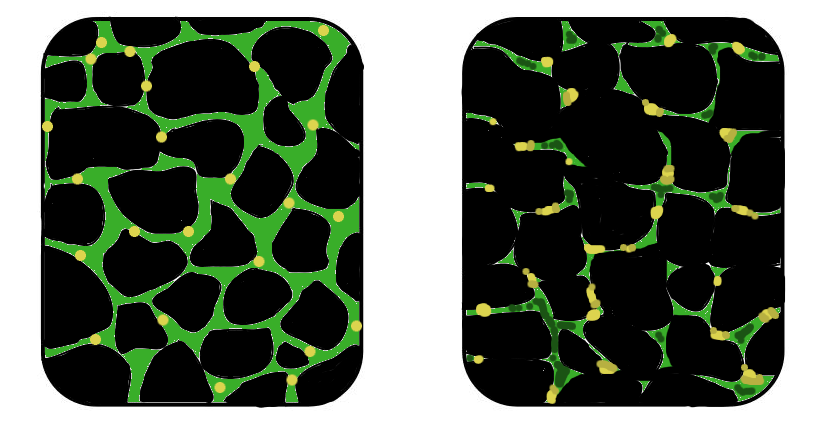
To observe this process in action, researchers employed advanced fluorescent microscopy, a technique that uses glowing dyes to track neuronal activity. In chronic pain models, neurons in the ACC showed abnormal firing patterns—as though the brain were locked into a feedback loop of distress. But after psilocin was introduced, those firing patterns calmed. The brain’s inner orchestra, once chaotic and discordant, regained harmony.
The fact that a single treatment could achieve this is especially noteworthy. Chronic pain often leads to long-term changes in the nervous system, rewiring the brain into a state of hypervigilance where pain is amplified. Psilocybin, it seems, has the potential to break that loop, at least temporarily, and perhaps guide the brain toward healthier wiring.
Beyond Pain: Implications for Mental Health
While this study focused on pain and mood, its implications stretch far wider. Many conditions—post-traumatic stress disorder, addiction, anxiety disorders—also involve dysregulated brain circuits. If psilocybin can restore balance in one domain, might it do so in others?
The idea is not new. Psychedelics have long been studied for their effects on depression and trauma, and clinical trials in recent years have shown promise. But this study brings a new layer of precision, tying those effects to specific circuits in the brain. By showing where and how psilocybin works, it moves the field closer to designing targeted therapies that can be both effective and safe.
The Road Ahead: Questions and Caution
For all its promise, this research is still in its early stages. The Penn team is careful to emphasize what remains unknown. How long do the benefits of psilocybin truly last? What happens with repeated doses? Can the brain’s rewiring be sustained, or does it fade with time? And how do we balance potential benefits with the risks of psychedelic experiences in vulnerable patients?
Dr. Stephen Wisser, a Penn Neuroscience Ph.D. student and co-author of the study, highlights the challenge: “While these findings are encouraging, we don’t know how long-lived psilocybin’s effects are or how multiple doses might be needed to adjust brain pathways involved in chronic pain for a longer-lasting solution.”
Safety also remains an open question. While psilocybin is not considered addictive, its hallucinogenic effects raise concerns about use in medical settings—particularly in patients recovering from surgery or coping with severe illness. Researchers will need to refine dosing strategies, delivery methods, and support systems to ensure that benefits can be harnessed without undue risk.
A Shift in Perspective
The significance of this work lies not only in what it reveals about psilocybin but in how it reframes the conversation about pain. For centuries, medicine has treated pain as a signal to be silenced, a fire alarm to be switched off. But this study suggests a more nuanced approach: instead of cutting the wires, we can adjust the brain’s response, helping patients live with less suffering even when the pain itself cannot be fully eliminated.
This shift mirrors a broader trend in neuroscience—away from brute force and toward modulation, away from numbing symptoms and toward rebalancing networks. Psilocybin’s role in this shift could be transformative.
Toward a Future of Healing
The journey ahead will be long. Clinical trials in humans will be essential, and the path from mouse studies to medicine is never simple. But hope matters, especially to those who live daily with pain that medicine has so far failed to ease.
For patients, psilocybin is not just a chemical—it represents the possibility of freedom from cycles of suffering, of waking up one morning without the crushing weight of both pain and despair. For physicians, it represents a chance to move beyond opioids, to offer care that heals without addiction. And for science, it represents another step toward understanding the extraordinary complexity of the brain.
As Dr. Cichon reflects, “These findings open the door to developing new, non-opioid, non-addictive therapies.” It is a door worth pushing wider.
Conclusion: Light in the Darkness
Chronic pain is more than a symptom; it is a condition that reshapes lives, minds, and futures. For those trapped in its grasp, even a glimmer of relief can feel like sunlight breaking through storm clouds. Psilocybin may not be a cure, but it could be a guide—a molecule that helps the brain find its way back to balance, harmony, and hope.
The story is just beginning. And with each discovery, the possibility grows that one day, millions of people may wake to a world where pain no longer rules their lives, where healing is not only about the body but about the mind and spirit too.
More information: Single-dose psilocybin rapidly and sustainably relieves allodynia and anxiodepressive-like behaviors in mouse models of chronic pain, Nature Neuroscience (2025). DOI: 10.1038/s41593-025-02068-0.