Sleep is supposed to be a sanctuary, a nightly retreat where the body restores itself and the mind processes the day’s experiences. Yet for millions of people around the world, sleep is not a refuge but a battlefield. Night after night, their breathing falters. Their bodies gasp for air. Their hearts pound with the strain of survival. They wake up exhausted, confused, and often unaware of what is happening to them. This condition has a name—sleep apnea—and though it is common, it remains misunderstood, underdiagnosed, and underestimated in its impact.
Sleep apnea is more than just loud snoring or disrupted rest. It is a serious sleep disorder with far-reaching consequences for health, relationships, and quality of life. It can increase the risk of heart disease, stroke, diabetes, depression, and accidents caused by fatigue. For some, untreated sleep apnea can be life-threatening. Understanding this condition is not just a matter of medical interest—it is a matter of reclaiming vitality, dignity, and years of life that might otherwise be lost to an invisible enemy.
What is Sleep Apnea?
Sleep apnea is a disorder in which breathing repeatedly stops and starts during sleep. These pauses in breathing, known as apneas, can last anywhere from a few seconds to a minute and may occur dozens or even hundreds of times in a single night. Each time it happens, the oxygen level in the blood drops, and the brain signals the body to wake up briefly to resume breathing. Most of the time, the awakening is so brief that the person does not remember it—but the effects accumulate, fragmenting sleep and preventing the body from reaching deep, restorative stages.
There are three primary types of sleep apnea:
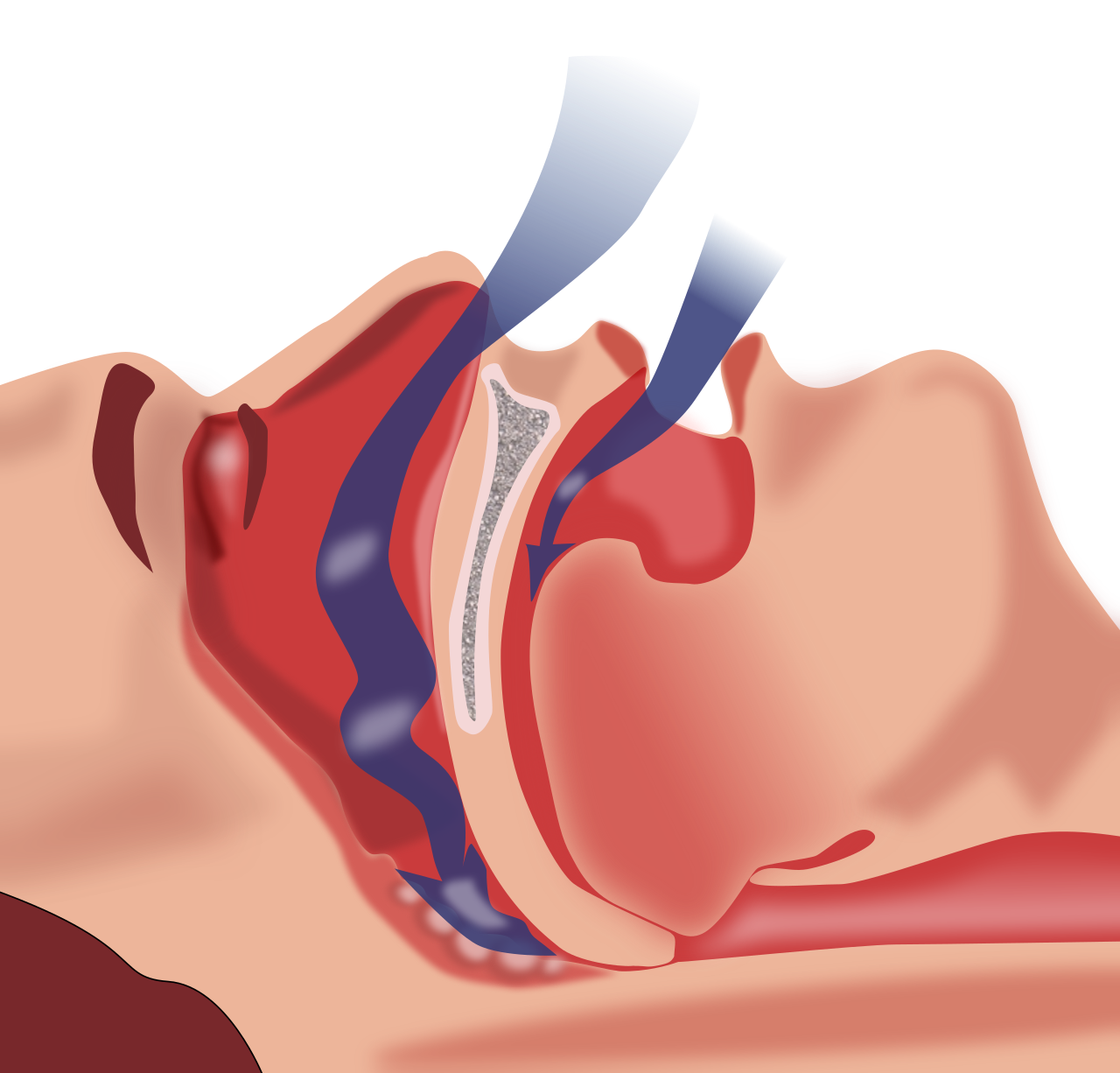
- Obstructive Sleep Apnea (OSA): The most common form, caused by relaxation of throat muscles that block the airway.
- Central Sleep Apnea (CSA): Less common, occurring when the brain fails to send proper signals to the muscles that control breathing.
- Complex Sleep Apnea Syndrome (also called Treatment-Emergent Central Sleep Apnea): A combination of obstructive and central sleep apnea.
While the mechanisms differ, the outcome is the same: disrupted breathing, fragmented sleep, and a cascade of health problems.
The Causes of Sleep Apnea
Sleep apnea does not have a single cause. Instead, it arises from a combination of anatomical, physiological, genetic, and lifestyle factors. The precise cause depends on the type of sleep apnea.
Causes of Obstructive Sleep Apnea (OSA)
OSA occurs when the muscles in the back of the throat relax too much during sleep. These muscles support critical structures such as the soft palate, uvula, tonsils, and tongue. When they relax, the airway narrows or closes, obstructing airflow.
Several factors increase the likelihood of this happening:
- Excess Weight: Fat deposits around the upper airway can obstruct breathing. Obesity is one of the strongest risk factors for OSA.
- Anatomical Features: A thick neck, narrow airway, large tonsils, or a deviated nasal septum can all contribute.
- Age: Muscle tone decreases with age, increasing the likelihood of airway collapse.
- Sex: Men are more likely to develop OSA than women, though risk for women increases after menopause.
- Alcohol and Sedatives: These substances relax throat muscles, worsening airway obstruction.
- Sleeping Position: Sleeping on the back can cause the tongue and soft palate to fall backward, narrowing the airway.
Causes of Central Sleep Apnea (CSA)
CSA is not about airway obstruction but about miscommunication between the brain and the respiratory muscles. It often arises from:
- Heart Disorders: Conditions such as heart failure or atrial fibrillation can interfere with the brain’s regulation of breathing.
- Neurological Conditions: Strokes, brainstem lesions, or neurodegenerative diseases may impair the brain’s respiratory centers.
- High Altitude: Reduced oxygen levels at high altitudes can trigger CSA in some individuals.
- Certain Medications: Opioids and other central nervous system depressants can disrupt breathing regulation.
Complex Sleep Apnea
Complex sleep apnea appears in patients initially diagnosed with obstructive sleep apnea who begin treatment with continuous positive airway pressure (CPAP). Instead of resolving, central apneas emerge during therapy, suggesting a more complex underlying mechanism.
Symptoms of Sleep Apnea
Sleep apnea can be elusive because many of its hallmark symptoms occur during sleep, unnoticed by the individual. Often, it is a bed partner, family member, or roommate who observes the problem first. Yet, the consequences spill into waking life, making themselves known in ways that affect health, performance, and relationships.
Nighttime Symptoms
- Loud Snoring: Often the most obvious and disruptive symptom, though not everyone who snores has sleep apnea.
- Pauses in Breathing: Witnessed by others, often followed by gasping, choking, or snorting sounds.
- Restless Sleep: Frequent tossing and turning, fragmented by awakenings.
- Night Sweats: Episodes of waking drenched in sweat due to the body’s stress response.
- Frequent Urination (Nocturia): Sleep apnea increases the production of atrial natriuretic peptide, leading to nighttime urination.
Daytime Symptoms
- Excessive Daytime Sleepiness: Feeling unrefreshed even after what seems like a full night’s sleep.
- Morning Headaches: Caused by changes in oxygen and carbon dioxide levels.
- Difficulty Concentrating: Impaired memory, attention, and problem-solving skills.
- Irritability and Mood Changes: Depression, anxiety, and short temper are common.
- Dry Mouth or Sore Throat: Due to breathing through the mouth at night.
The Health Consequences of Untreated Sleep Apnea
Sleep apnea is not just about poor sleep. Over time, the constant oxygen deprivation and stress response strain nearly every organ system. Untreated, it can contribute to:
- Cardiovascular Disease: Hypertension, heart attack, heart failure, and arrhythmias.
- Stroke: Increased risk due to blood pressure fluctuations and vascular stress.
- Metabolic Disorders: Insulin resistance, type 2 diabetes, and obesity.
- Cognitive Decline: Impaired memory, reduced executive function, and higher risk of dementia.
- Mood Disorders: Heightened risk of depression and anxiety.
- Accidents: Increased likelihood of workplace and motor vehicle accidents due to fatigue.
Diagnosis of Sleep Apnea
Because sleep apnea occurs during sleep, diagnosing it requires specialized tests. Self-reported symptoms are important but not sufficient for confirmation.
Clinical Evaluation
A physician begins by gathering a detailed medical history, including symptoms, sleep patterns, and risk factors. Questionnaires such as the Epworth Sleepiness Scale may help quantify daytime sleepiness. Physical examination focuses on airway anatomy, neck circumference, and cardiovascular health.
Polysomnography (Sleep Study)
The gold standard for diagnosing sleep apnea is an overnight sleep study, known as polysomnography. Conducted in a sleep lab, this test records brain activity, eye movement, heart rate, breathing patterns, blood oxygen levels, and body movements. It provides a comprehensive picture of sleep quality and breathing disturbances.
Home Sleep Apnea Testing (HSAT)
For certain patients, home-based tests are available. These portable monitors measure breathing, oxygen levels, and heart rate but do not capture as much detail as in-lab studies. They are most useful for diagnosing moderate-to-severe OSA in otherwise healthy individuals.
Severity Classification
The Apnea-Hypopnea Index (AHI) is used to classify severity:
- Mild: 5–14 events per hour
- Moderate: 15–29 events per hour
- Severe: 30+ events per hour
Treatment Options for Sleep Apnea
Treatment for sleep apnea aims to restore normal breathing during sleep, improve sleep quality, and reduce associated health risks. Approaches vary depending on the type and severity of apnea, as well as patient-specific factors.
Lifestyle Modifications
For mild cases, lifestyle changes can significantly improve symptoms:
- Weight loss reduces airway obstruction.
- Avoiding alcohol and sedatives prevents excessive muscle relaxation.
- Changing sleep position (side-sleeping instead of back-sleeping) can help keep the airway open.
- Quitting smoking reduces inflammation and swelling in the airway.
Continuous Positive Airway Pressure (CPAP)
CPAP is the most widely used and effective treatment for obstructive sleep apnea. It delivers a steady stream of air through a mask, keeping the airway open. While highly effective, adherence can be challenging due to discomfort, noise, or claustrophobia.
Alternatives to CPAP
- Bi-level Positive Airway Pressure (BiPAP): Provides different pressure levels for inhalation and exhalation, useful for patients who struggle with CPAP.
- Adaptive Servo-Ventilation (ASV): For central sleep apnea and complex cases, adjusts airflow based on detected breathing patterns.
- Oral Appliances: Custom-fitted devices reposition the jaw or tongue to keep the airway open. They are less effective than CPAP but more tolerable for some patients.
Surgical Options
Surgery may be considered for patients who cannot tolerate CPAP or oral appliances:
- Uvulopalatopharyngoplasty (UPPP): Removes tissue from the throat to widen the airway.
- Genioglossus Advancement: Moves the tongue muscle attachment forward to open the airway.
- Maxillomandibular Advancement: Repositions the upper and lower jaws to enlarge the airway.
- Hypoglossal Nerve Stimulation: An implantable device stimulates the nerve controlling the tongue, preventing collapse.
Treatment of Central Sleep Apnea
For CSA, treatment focuses on addressing underlying causes such as heart failure or medication use. Options may include:
- Optimizing heart failure therapy.
- Reducing or changing medications that depress breathing.
- Using adaptive servo-ventilation devices.
- Supplemental oxygen therapy.
Living with Sleep Apnea
Treatment is not the end of the journey but the beginning of a new relationship with health. Patients often describe the profound difference once therapy begins: waking up refreshed, experiencing improved mood, and rediscovering energy they had forgotten was possible.
However, challenges remain. CPAP adherence can be difficult, requiring support, patience, and sometimes multiple mask trials. Lifestyle changes demand commitment. Emotional support is crucial, as sleep apnea can affect self-esteem, intimacy, and family dynamics.
With proper management, people with sleep apnea can lead full, healthy lives. Early diagnosis and treatment not only improve sleep but also protect the heart, brain, and overall longevity.
The Future of Sleep Apnea Care
Research continues to shed light on new treatment options and diagnostic tools. Advances in wearable technology may soon allow for more accessible home-based monitoring. Personalized medicine, considering genetics and individual anatomy, may lead to tailored treatments. Novel devices, such as minimally invasive nerve stimulators, promise new hope for patients resistant to traditional therapies.
The conversation around sleep apnea is also expanding culturally. Greater awareness campaigns aim to destigmatize the disorder, encourage early evaluation, and promote public understanding that sleep health is as vital as nutrition or exercise.
Conclusion: Restoring Breath, Restoring Life
Sleep apnea is not simply about snoring or fatigue; it is about interrupted life itself. Each pause in breathing is a reminder of the body’s vulnerability, yet also of its resilience when given the right support. By understanding its causes, recognizing its symptoms, seeking timely diagnosis, and committing to effective treatment, individuals can reclaim not just their nights, but their days.
To heal sleep apnea is to restore more than breath—it is to restore vitality, clarity, and the simple, profound joy of waking up refreshed to meet the day.