There is something deeply unsettling about the idea of the body turning against itself. Autoimmune diseases do just that—convince our immune systems, meant to defend us from harm, to attack the very tissues they are designed to protect. This betrayal is not just metaphorical but biological, unfolding at the cellular level where confusion and inflammation reign. Unlike infectious diseases caused by bacteria or viruses, autoimmune disorders are a dysfunction of self-recognition. The immune system mistakes healthy organs, cells, or tissues for foreign invaders, and the result is chronic, often life-altering, inflammation.
These diseases do not fit into neat diagnostic boxes. They include a wide range of conditions—rheumatoid arthritis, multiple sclerosis, lupus, Crohn’s disease, psoriasis, type 1 diabetes, and Hashimoto’s thyroiditis, to name just a few. Some target the skin, others the brain, joints, digestive tract, or endocrine system. They may appear suddenly or creep in over years, their symptoms waxing and waning in cruel unpredictability. No two patients experience them in exactly the same way.
The quest to reverse autoimmune disease has become a medical frontier. Scientists, doctors, and patients alike ask the same burning question: Can these diseases not just be managed but actually reversed? The answer is far more complex than a simple yes or no. To begin unraveling it, one must understand what causes autoimmune diseases in the first place and why the immune system loses its way.
Unraveling the Immune Puzzle: Causes and Complexity
The immune system is a marvel of evolutionary engineering. Its ability to distinguish between self and non-self is crucial for survival. Yet for reasons that are still not entirely clear, this recognition system can malfunction. What causes this breakdown is the subject of intense scientific inquiry. Current research suggests that autoimmune diseases arise from a combination of genetic predisposition and environmental triggers.
Certain genes make individuals more susceptible to developing autoimmunity, but genes alone are not destiny. Environmental factors such as viral infections, gut microbiome imbalances, chronic stress, toxins, and dietary components may all act as tipping points. It’s as if the immune system is a loaded gun, and the environment pulls the trigger.
In recent years, the gut has taken center stage in autoimmune research. Scientists have discovered that gut health and immune function are inextricably linked. The gut houses a significant portion of the immune system, and its microbial inhabitants—trillions of bacteria and other microorganisms—play a critical role in regulating immune responses. When the gut barrier becomes “leaky,” allowing undigested food particles, microbes, or toxins into the bloodstream, the immune system may respond with inflammation, sometimes mistaking these substances for threats and attacking the body’s own tissues.
This interplay between genes, the gut, and environmental factors suggests a dynamic rather than a static condition. It opens the door to the possibility that if the triggers can be identified and removed, and if the immune system can be recalibrated, reversal—or at least remission—might be possible.
Conventional Medicine’s Approach: Manage, Don’t Cure
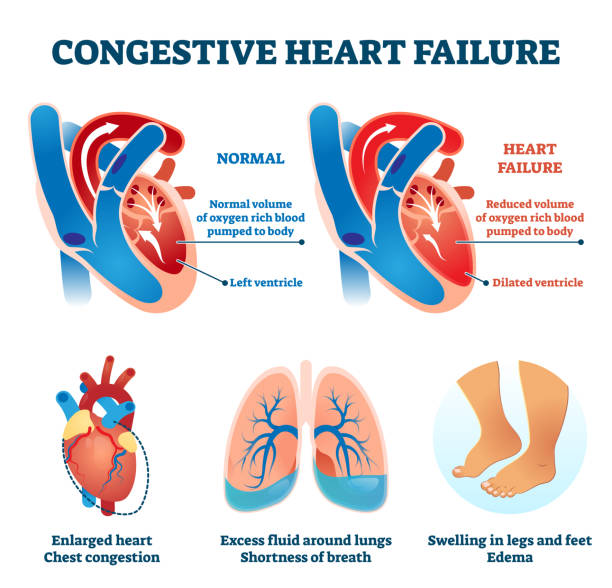
Traditionally, the goal of conventional medicine has been to manage autoimmune diseases rather than reverse them. This is not due to a lack of ambition but rather a reflection of the complexity involved. Autoimmune diseases are often lifelong conditions with no clear path to eradication. Physicians typically focus on controlling inflammation, reducing symptoms, and preventing long-term damage.
Treatment often begins with anti-inflammatory drugs, corticosteroids, or immunosuppressants. These medications can be life-saving and greatly improve quality of life. More advanced treatments involve biologic drugs that target specific components of the immune system. While these therapies have revolutionized autoimmune care, they come with significant trade-offs. Suppressing the immune system can increase the risk of infections and other complications.
The problem with this approach is that it often addresses the symptoms, not the underlying cause. It’s akin to silencing a car alarm without figuring out what triggered it. As such, patients are frequently left in a state of managed disease, their immune system kept in check but never truly corrected.
Still, this strategy has its merits, especially for patients with severe or life-threatening autoimmune activity. In these cases, the primary goal is stability and symptom control. Yet for those seeking deeper healing or even reversal, the limitations of conventional treatment create both frustration and motivation to explore alternatives.
Functional Medicine: A New Paradigm for Reversal?
In contrast to the standard model, functional medicine takes a different approach. It seeks not just to suppress symptoms but to uncover root causes. Practitioners in this field consider autoimmune diseases to be the result of a broader systems imbalance—often involving the gut, hormones, toxins, stress levels, and nutrient deficiencies. Instead of asking, “What drug matches this disease?” they ask, “What caused this immune dysfunction in the first place?”
Functional medicine operates on the idea that the body has an innate capacity to heal itself if given the right conditions. This includes restoring gut integrity, balancing hormones, detoxifying the liver, reducing inflammation through diet, and managing stress. Many in this field believe that autoimmune diseases, while perhaps not curable in the strictest sense, can be reversed into long-term remission.
The term “reversal” here does not imply a total cure or the erasure of all symptoms. Instead, it refers to a state in which disease activity is significantly reduced or dormant, symptoms are minimal or absent, and the immune system behaves in a more regulated manner. For some patients, this state can last months, years, or even indefinitely, particularly if they maintain the lifestyle changes that led them there.
There is anecdotal evidence and emerging clinical data to support these claims. Patients report remarkable improvements—or even the complete absence of symptoms—after implementing functional medicine protocols. These typically involve an anti-inflammatory diet, elimination of food triggers (such as gluten, dairy, and processed sugars), gut-healing supplements, mindfulness practices, and detoxification strategies. While more rigorous scientific studies are needed to validate these methods, the growing body of positive case reports suggests that reversal is not just a dream—it may be a possibility for some.
The Role of Diet: Fuel or Fire?
Diet may be one of the most powerful and yet controversial tools in the management of autoimmune diseases. Scientific literature increasingly supports the notion that what we eat can either exacerbate or ease autoimmune conditions. Certain foods are known to trigger inflammation or contribute to a “leaky gut,” while others seem to calm immune activity and promote healing.
Gluten, for example, has been linked not only to celiac disease but also to other autoimmune conditions. In genetically susceptible individuals, gluten may increase intestinal permeability, prompting immune responses that spill over into other systems. Similarly, dairy, refined sugar, trans fats, and food additives can fuel inflammation in some people.
Conversely, diets rich in whole foods, leafy greens, omega-3 fats, and antioxidants have been shown to lower inflammation. The so-called “Autoimmune Protocol” (AIP), a stricter form of the Paleo diet, has gained popularity for its emphasis on nutrient density and elimination of common food triggers. Some patients following the AIP report dramatic symptom improvement and even remission, though controlled clinical studies are still ongoing.
What becomes clear is that diet is not a secondary factor. It is a central player in immune function. Food can act as medicine—or as a slow-acting toxin. For individuals battling autoimmune diseases, identifying food sensitivities and nourishing the body with anti-inflammatory nutrition can be a critical step toward reversal.
The Gut-Immune Axis: Healing from the Inside Out
The importance of gut health in autoimmune diseases cannot be overstated. Scientists have discovered that the integrity of the intestinal lining plays a major role in preventing autoimmune activation. When the gut barrier becomes compromised—a condition often referred to as “leaky gut syndrome”—molecules that would normally stay within the digestive tract leak into the bloodstream, triggering systemic immune responses.
This phenomenon has been observed in conditions like rheumatoid arthritis, lupus, and type 1 diabetes. The gut microbiota—comprising trillions of bacteria—also plays a key role. Dysbiosis, or an imbalance in microbial populations, can lead to increased inflammation and immune dysfunction.
Healing the gut involves multiple strategies: removing irritants, replacing digestive enzymes, reinoculating the gut with beneficial bacteria through probiotics and fermented foods, and repairing the gut lining with nutrients such as zinc, L-glutamine, and collagen. While the science is still evolving, this model of gut-centric healing has gained traction among patients and clinicians who have witnessed significant turnarounds in autoimmune disease activity.
Stress, Sleep, and the Nervous System’s Role
While we often view stress as a psychological state, it has profound biological consequences. Chronic stress activates the hypothalamic-pituitary-adrenal (HPA) axis, leading to elevated cortisol levels and immune dysregulation. In individuals with autoimmune disease, stress can trigger flares or exacerbate symptoms. The relationship is bi-directional—autoimmunity increases stress, and stress feeds autoimmunity.
Sleep is another underappreciated variable. Poor sleep quality can impair immune function, increase inflammation, and reduce the body’s ability to repair itself. Studies show that individuals with autoimmune diseases often suffer from insomnia, sleep apnea, or non-restorative sleep, further complicating their condition.
Addressing stress and sleep is thus not optional—it is foundational. Mind-body practices such as yoga, meditation, breathing exercises, and even therapy have been shown to reduce inflammation and improve immune balance. In the pursuit of autoimmune reversal, the nervous system must be treated with as much care as the immune system itself.
The Limits of Reversal: What We Know and What We Don’t
Despite promising advances, it is important to acknowledge the limitations of current knowledge. Not all autoimmune diseases are equally reversible. Conditions that have led to significant tissue damage or organ destruction may not be fully repairable. For example, in type 1 diabetes, where insulin-producing cells are destroyed, reversal may not restore function to the pancreas. Similarly, in multiple sclerosis, existing neurological damage might be irreversible even if inflammation subsides.
Moreover, reversal depends on timing. Early intervention, before the immune system causes extensive damage, offers the best chance of turning the tide. Patients in advanced stages may still benefit from remission strategies, but full reversal becomes less likely.
Research is ongoing. Large-scale, randomized controlled trials are needed to test the long-term efficacy of lifestyle-based interventions. Until then, most evidence remains anecdotal or based on smaller pilot studies. Yet even in the absence of definitive answers, the accumulation of patient experiences suggests that, for some, autoimmune diseases need not be a life sentence.
The Future: Personalized Autoimmune Medicine
The future of autoimmune care lies in personalization. No two patients are alike, and no single protocol works for everyone. Genetic testing, microbiome analysis, hormone profiling, and immune mapping are making it possible to tailor treatments to the individual. This shift from disease-centered to patient-centered care marks a profound change in medicine.
Already, advances in genomics and AI are helping identify subtypes of autoimmune diseases, predict treatment responses, and uncover novel drug targets. The integration of conventional medicine with functional and integrative approaches offers the best of both worlds—scientific rigor combined with holistic care.
Autoimmune diseases may not yet be fully reversible across the board, but the trajectory of research and patient experience points to a more hopeful future. For many, remission is a realistic goal. For others, functional improvement and symptom control can feel like a rebirth. And for all, the growing understanding of immune regulation opens a pathway out of suffering and toward resilience.
A New Narrative of Healing
For too long, the narrative surrounding autoimmune diseases has been one of inevitability and decline. But emerging science is challenging that fatalism. From the gut to the brain, from food to feelings, every system of the body contributes to immune balance. When these systems are supported holistically, remarkable transformations can occur.
Reversal does not mean forgetting that a disease ever existed. It means living with vitality, often without symptoms, and reclaiming agency over one’s health. It means replacing fear with understanding and helplessness with action. It means honoring the complexity of the body while believing in its capacity for renewal.
Autoimmune diseases are not merely disorders—they are signals. And if we listen closely, they may teach us not only how to heal, but how to live.