From the moment a new life begins to grow inside the womb, an intricate dialogue unfolds between mother and child. Every heartbeat, every breath, and every molecular signal exchanged between them forms a delicate web of communication that shapes the developing brain and body. For decades, scientists have known that a mother’s health during pregnancy can profoundly influence the lifelong well-being of her child. But new research is beginning to reveal just how deep those influences may run—down to the molecular code that governs how genes express themselves.
Among the most striking findings in recent years is that infections during pregnancy, even when mild, can leave subtle yet lasting marks on a developing brain. These marks may increase the risk of neurodevelopmental disorders later in life, including one of the most mysterious and devastating conditions in psychiatry—schizophrenia.
When the Immune System Speaks to the Fetus
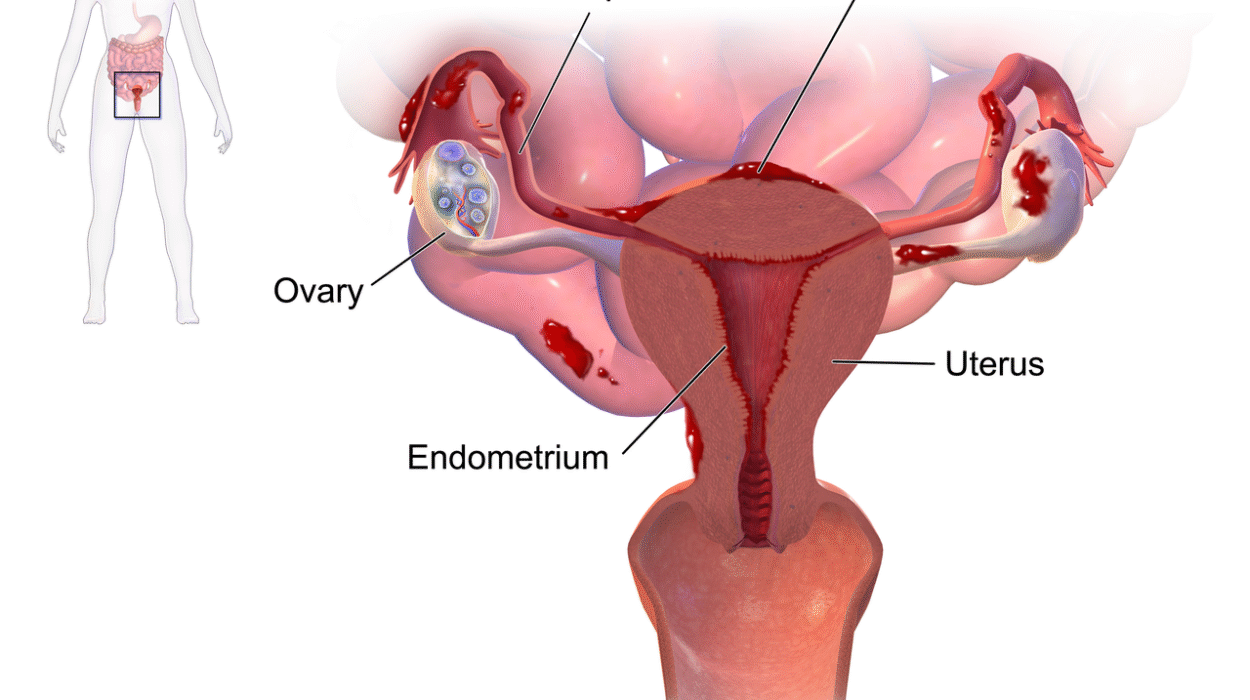
An infection is more than just a fever or sore throat. It is a full-body alarm. When bacteria, viruses, fungi, or parasites invade, the immune system launches a complex defense—releasing chemical messengers called cytokines that signal the body to fight back. For an expectant mother, this immune storm is not contained within her own body. Her immune system communicates across the placenta, the lifeline between her and the developing fetus.
Most of the time, this communication is protective. The maternal immune system provides antibodies and signals that prepare the fetus for life outside the womb. But sometimes, the response can have unintended consequences. If the immune system becomes overactive, the surge of inflammatory molecules can subtly alter how the fetal brain develops.
This process, known as maternal immune activation (MIA), has become a major focus in developmental neuroscience. MIA doesn’t directly infect the fetus. Instead, it changes the chemical environment in which the brain grows, influencing how neurons form, connect, and communicate. Scientists now believe this immune activation can sometimes set the stage for later cognitive or behavioral challenges.
The Search for Biological Traces
Epidemiological studies—those that look at patterns across large populations—have long shown a statistical link between infections during pregnancy and a higher risk of conditions like autism or schizophrenia in offspring. But correlation is not causation. For years, researchers have asked: What biological processes could explain this link?
To answer that question, scientists began to explore epigenetics—the study of how experiences and environmental factors influence gene expression without changing the underlying DNA sequence. Epigenetic mechanisms act like dimmer switches on genes, turning some up and others down, determining which genetic instructions get read and which stay silent.
It is through these molecular switches that maternal stress, diet, and even infection might shape the brain’s architecture. The new study from the University of Manchester and Manchester Metropolitan University takes this line of investigation a step further, exploring how maternal infection might alter the molecular landscape of the fetal brain in ways that echo into adulthood.
A Window Into the Developing Brain
Because it’s impossible to study human fetal brain development directly, the researchers turned to animal models—specifically, rats. Their goal was to mimic maternal immune activation in a controlled setting and observe how it influenced the brains of offspring, from prenatal life through adulthood.
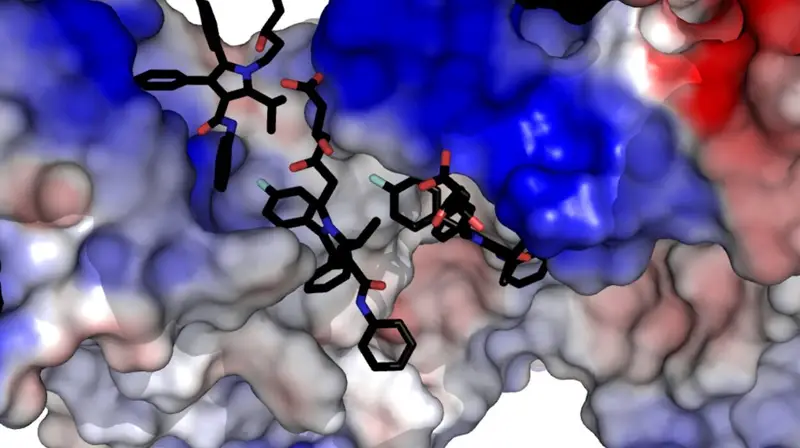
The team, led by Rebecca M. Woods and Harry G. Potter, focused on the cortex, the outer layer of the brain responsible for higher cognitive functions like thought, memory, and language. They examined two key molecules: S-adenosylmethionine (SAM) and S-adenosylhomocysteine (SAH). These molecules are central players in DNA methylation, an epigenetic process that acts as a chemical switchboard controlling gene activity.
The ratio between SAM and SAH serves as a measure of the cell’s “methylation capacity”—its ability to add or remove methyl groups that regulate gene expression. A balanced ratio keeps gene activity in harmony, while a disrupted one can lead to long-term changes in which genes are turned on or off.
The scientists found that when a pregnant rat’s immune system was activated to simulate infection, the SAM/SAH ratio in the fetal brain shifted dramatically. This meant that the methylation machinery in the fetal cortex was being altered in response to the mother’s immune reaction.
The Epigenetic Echo of Infection
The most fascinating—and unexpected—discovery came when the researchers traced these molecular changes across time. They found that the disruption in methylation was most pronounced during fetal development, faded shortly after birth, and then mysteriously re-emerged in adulthood.
This pattern suggested that the infection didn’t permanently damage the developing brain. Instead, it appeared to “program” the epigenetic system to behave differently later in life, resurfacing at a time when the brain undergoes major reorganization—precisely when schizophrenia tends to appear in humans.
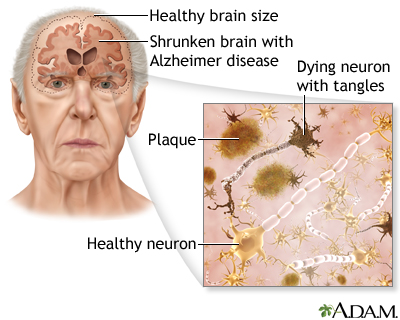
The adult rats that had been exposed to maternal immune activation displayed cognitive deficits resembling those seen in schizophrenia, including problems with attention, memory, and learning. When the researchers examined their brains, they found altered DNA methylation patterns in genes associated with schizophrenia risk and neural signaling.
In essence, an immune challenge during pregnancy had set in motion a molecular ripple effect that subtly rewired the offspring’s brain development and behavior.
How the Findings Illuminate Schizophrenia
Schizophrenia remains one of the most enigmatic mental health disorders, affecting roughly one in every hundred people worldwide. It is characterized by hallucinations, delusions, disorganized thinking, and cognitive impairments. Its origins have long been debated: is it genetic, environmental, or both?
The new findings support a view that schizophrenia may arise from an intricate dance between genetic vulnerability and environmental triggers. A child might inherit certain genetic risk factors, but those genes may stay dormant unless “switched on” by early-life events—like a maternal infection during pregnancy.
Epigenetics provides the missing link. It explains how non-genetic factors can influence how risk genes behave. Maternal immune activation, by altering methylation patterns, could create a brain that is more sensitive to later stressors or hormonal changes. The result might be an increased susceptibility to developing schizophrenia in adolescence or adulthood.
The Power and Promise of Epigenetics
The notion that life experiences—even before birth—can shape the brain through epigenetic changes is both sobering and hopeful. It challenges the old idea that our genes determine our destiny. Instead, it reveals a more dynamic truth: genes are responsive, adaptable, and sensitive to the environments we inhabit.
This flexibility means that early biological disruptions may not be irreversible. Understanding the precise epigenetic mechanisms linking maternal infection to later mental illness could open the door to new preventive and therapeutic strategies.
Imagine being able to identify at-risk pregnancies early, or developing medications that can rebalance methylation patterns before symptoms ever emerge. The goal is not to assign blame or fear to mothers, but to empower future generations with knowledge and care that protects brain health from the very beginning of life.
A Delicate Balance Between Protection and Risk
Pregnancy is a remarkable balancing act. The mother’s immune system must defend against pathogens while simultaneously tolerating a genetically distinct fetus. This requires a finely tuned regulation of inflammation. Too little immune response could allow infections to spread; too much could disrupt fetal development.
The recent findings underscore how easily this balance can be tipped. Even a mild infection, if it triggers strong immune signaling, may leave subtle marks on the developing brain’s chemistry. Yet it’s also important to remember that most pregnancies, even those involving infections, do not result in neurodevelopmental disorders.
The key lies in individual variation—in genes, immune responses, timing, and environmental context. Science is only beginning to unravel these intricate interactions, but each discovery brings us closer to understanding how to protect and nurture mental health before birth.
The Future of Research and Hope for Prevention
The study from Manchester is part of a growing wave of research exploring the biological origins of mental illness. By combining neuroscience, genetics, and immunology, scientists are piecing together a more complete picture of how the brain develops—and how it sometimes goes astray.
Future research will likely focus on mapping exactly which genes are most affected by maternal immune activation and identifying when during pregnancy the brain is most vulnerable. These insights could lead to new guidelines for prenatal care, new diagnostic tools, and even new treatments that restore healthy gene regulation.
It may also lead to a more compassionate understanding of mental illness itself. If conditions like schizophrenia begin as biological missteps in early development, rather than moral or personal failings, society can move toward more empathy, early intervention, and support.
Beyond the Laboratory: The Emotional Landscape
Science often deals in data, but behind every discovery lies a human story. For mothers, the idea that their health during pregnancy can shape their child’s mental future is both profound and emotional. It reminds us how interconnected we truly are—how a single infection, a single immune response, can ripple across generations.
Yet this understanding should not provoke fear. Instead, it offers empowerment. Knowledge of these mechanisms allows healthcare providers to design better prenatal care, promote vaccinations, manage infections safely, and monitor immune responses during pregnancy. It also encourages society to support maternal health as a cornerstone of public health, recognizing that the care we give to mothers is, quite literally, an investment in the minds of the future.
A New Frontier in Understanding the Mind
The discovery of how maternal infections may influence epigenetic patterns in the developing brain does not close the chapter on schizophrenia—it opens a new one. It challenges scientists to think of mental illness not just as a disease of the adult brain, but as the echo of developmental processes set in motion long before birth.
Every insight into these mechanisms deepens our understanding of what it means to be human: the fragility and resilience of life, the interplay between biology and environment, the invisible threads connecting one generation to the next.
In the end, this research carries a powerful message—that our beginnings matter, but they do not define us entirely. Within the molecular memory of the brain lies both the record of our origins and the potential for healing. The task of science, and of humanity, is to read that memory with compassion, curiosity, and care.
More information: Rebecca M. Woods et al, Developmental modulation of schizophrenia risk gene methylation in offspring exhibiting cognitive deficits following maternal immune activation, Molecular Psychiatry (2025). DOI: 10.1038/s41380-025-03147-1.