Adolescence is a period of rapid neurological and physiological change. During this time, the brain undergoes significant remodeling, particularly in areas responsible for emotional regulation, decision-making, and sensory processing. Against this backdrop, the widespread prescription of antidepressants such as fluoxetine—better known by its commercial name, Prozac—has sparked both hope and caution. As mental health challenges among young people surge, so too has the use of selective serotonin reuptake inhibitors (SSRIs), with fluoxetine often at the forefront.
A recent study published in the Journal of Psychiatric Research adds a new layer of complexity to our understanding of fluoxetine’s long-term effects. The research, led by psychology professor Sergio Iñiguez at the University of Texas at El Paso, reveals that female mice exposed to fluoxetine during adolescence exhibited increased sensitivity to pain and reduced body weight well into adulthood. These changes persisted long after the drug had cleared from their systems, suggesting permanent alterations to neurological and physiological systems.
The Science Behind the Study
To investigate the potential long-term consequences of adolescent fluoxetine exposure, Iñiguez and his team designed a controlled laboratory experiment using a well-established model organism: the C57BL/6 female mouse. These mice are widely favored in biomedical research due to their consistent genetics and well-characterized behavioral patterns, making them ideal for testing hypotheses about drug effects.
The adolescent mice were divided into two groups. One group received fluoxetine dissolved in their drinking water for a 15-day period coinciding with a critical window of brain development—postnatal days 35 to 49, which roughly parallels human adolescence. The control group received regular water. The fluoxetine dosage was carefully calibrated to replicate antidepressant levels used in human adolescents, with adjustments made to account for the higher metabolic rate of young female mice.
Three weeks after the treatment ended—once the mice had reached full adulthood—the researchers conducted a hot plate test to evaluate pain sensitivity. This test involves placing a mouse on a heated surface and recording the time it takes to react to the discomfort, such as by licking its hind paw. Shorter reaction times indicate heightened pain sensitivity, known in clinical terms as hyperalgesia.
Pain Sensitivity and the Hidden Legacy of Early Medication
The results were striking. Mice that had been treated with fluoxetine during adolescence reacted significantly faster to the thermal stimulus than their untreated peers. This difference was not subtle—it indicated a profound increase in pain sensitivity that could not be easily attributed to transient drug effects. Notably, the fluoxetine had long since been metabolized and eliminated from their systems by the time of the test.
This heightened sensitivity suggests that fluoxetine may interfere with the development of neural circuits involved in pain regulation. One plausible explanation lies in the role of serotonin, the neurotransmitter targeted by SSRIs like fluoxetine. Serotonin is not only central to mood regulation but also modulates pain perception. By altering serotonin levels during a critical developmental phase, the drug may leave a lasting imprint on how the brain processes discomfort.
Weight Changes That Persist
In parallel with pain sensitivity, the researchers tracked body weight across the treatment and post-treatment phases. A subtle but persistent pattern emerged. Starting as early as the second day of treatment, the fluoxetine-exposed mice gained less weight than their control counterparts. This trend continued into adulthood, with the treated mice maintaining a significantly lower body mass even weeks after the drug was withdrawn.
While body weight can influence pain sensitivity—leaner animals may respond differently to physical stimuli—the researchers took care to ensure that movement capabilities remained unaffected. Prior studies have demonstrated that fluoxetine does not impair motor activity in rodents, which helped rule out general mobility differences as a factor in the pain tests.
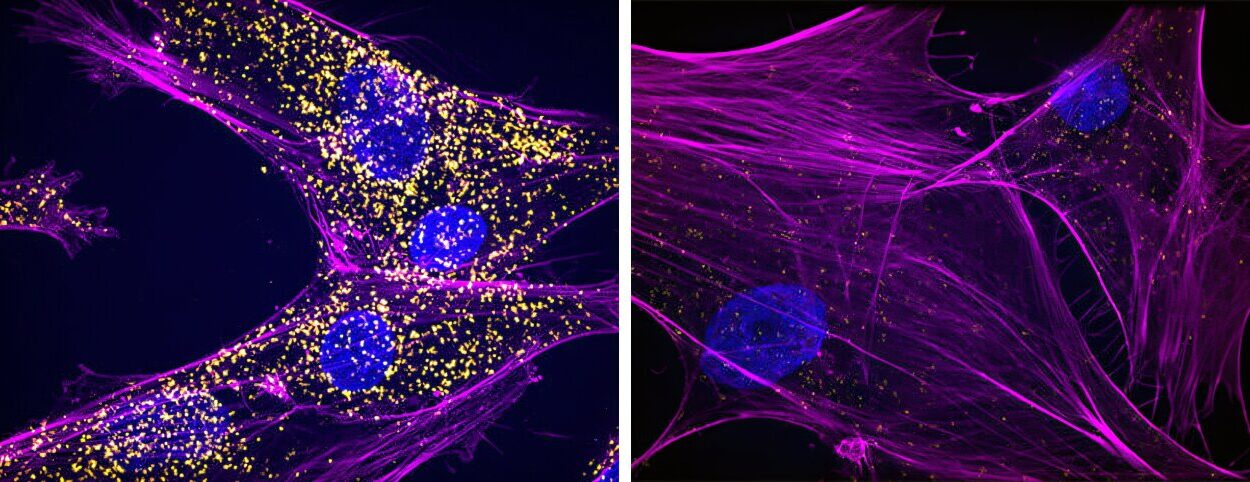
The Brain, Serotonin, and the Overlooked Side Effects
The idea that antidepressants could shape pain perception may seem surprising, but it aligns with emerging evidence about serotonin’s multifaceted role in the body. Beyond its famous mood-regulating effects, serotonin is deeply involved in sensory integration, pain modulation, and even inflammation. Disrupting this chemical balance during adolescence, when the brain is still forging critical connections, can have ripple effects far beyond emotional well-being.
Key brain regions like the prefrontal cortex, amygdala, and hypothalamus continue to mature throughout adolescence. These areas are implicated not just in mood disorders but also in how pain is interpreted and managed. Fluoxetine may interfere with the normal pruning and strengthening of neural pathways, effectively rerouting how the brain handles both emotional and physical stimuli.
Inflammation and Pain: A Second Mechanism?
Another potential mechanism behind the increased pain sensitivity involves inflammation. SSRIs, including fluoxetine, have been shown in both animal and human studies to alter levels of inflammatory markers. In children and teens, long-term fluoxetine use has been associated with elevated levels of molecules like interleukin-6 (IL-6) and interleukin-1β—key players in the body’s immune response. Chronic low-grade inflammation is known to sensitize pain pathways, possibly making individuals more reactive to discomfort.
If fluoxetine triggers or amplifies inflammatory processes during adolescence, it may contribute to a biological environment in which pain sensitivity is heightened. This dual pathway—via serotonin modulation and immune signaling—could help explain the enduring effects observed in the mice.
A Word of Caution for Prescribers
While the study’s findings are derived from an animal model and cannot be directly extrapolated to human adolescents without additional research, they raise vital concerns about how widely used antidepressants may produce unintended side effects. The prospect that fluoxetine might alter pain perception or body development highlights the need for a more nuanced understanding of its long-term impact, especially when prescribed during sensitive developmental periods.
Professor Iñiguez emphasized this point in a statement to PsyPost, noting that the findings “underscore the importance of careful consideration when prescribing SSRIs to young people. The effects are not necessarily confined to mood—they may also shape how the brain processes pain and other sensory inputs, potentially for years to come.”
The Bigger Picture: Depression, Pain, and the Complexity of Treatment
Depression and pain share a complicated relationship. Both conditions are highly comorbid, with individuals suffering from chronic pain often experiencing depression, and vice versa. This overlap makes it all the more critical to understand how treatments for one may influence the other. If SSRIs like fluoxetine affect pain sensitivity, then their long-term use could have unintended consequences that either help or hinder overall well-being.
This is especially relevant considering that fluoxetine is often prescribed not just for depression, but for eating disorders and premenstrual mood disorders—both of which are more prevalent in adolescent girls and can involve pain symptoms. Understanding whether fluoxetine contributes to or alleviates these symptoms over the long term is a pressing question for both clinicians and researchers.
Looking Ahead: What Future Research Should Explore
The current study opens several promising avenues for further investigation. One important limitation noted by the authors was the absence of environmental stressors in the experimental setup. In real-world scenarios, adolescents taking fluoxetine are often coping with significant stress, trauma, or co-occurring psychiatric conditions. How fluoxetine interacts with these factors to influence brain development and pain processing remains largely unknown.
Future studies should consider integrating psychological stress models and exploring additional variables such as sex differences, dosage timing, and the impact of combined medication regimens. Moreover, delving into molecular pathways—particularly those involving the prefrontal cortex, hypothalamus, and inflammation—may help clarify how exactly fluoxetine reshapes neural and immune architecture.
A Call to Rethink Adolescent Psychiatric Treatment
In light of these findings, it may be time to reevaluate how and when SSRIs are prescribed to adolescents. While fluoxetine can be life-changing for those battling severe depression, its growing use among young people—with prescriptions often rising in tandem with societal stressors—demands a closer look at potential trade-offs.
Ultimately, this study doesn’t suggest that fluoxetine should be abandoned, but rather that its use should be carefully tailored, monitored, and continuously reassessed as new evidence emerges. The adolescent brain is still building the blueprint for adulthood, and even small chemical interventions during this stage may echo across a lifetime.