Pain is a part of life. It warns us of danger, signals when something is wrong, and often fades when the body heals. But for millions of people, the pain doesn’t stop. It lingers for months, sometimes years, without an obvious cause or cure. Chronic pain becomes more than a symptom—it becomes a shadow, darkening daily life.
Now, a new study from The Hebrew University of Jerusalem has uncovered why this happens. The research, published in Science Advances, reveals that the brain has a built-in system to quiet pain signals when they’re no longer needed. In short-term, or “acute,” pain, this system works like a brake, calming the nerves and helping the body return to normal. But in chronic pain, that brake fails—and the pain signals just keep coming.
This discovery is not only a breakthrough in our understanding of how pain works, but also a ray of hope for millions living with chronic suffering. It opens the door to new treatments that could stop pain from becoming permanent in the first place.
The Brain’s Hidden Pain Gate
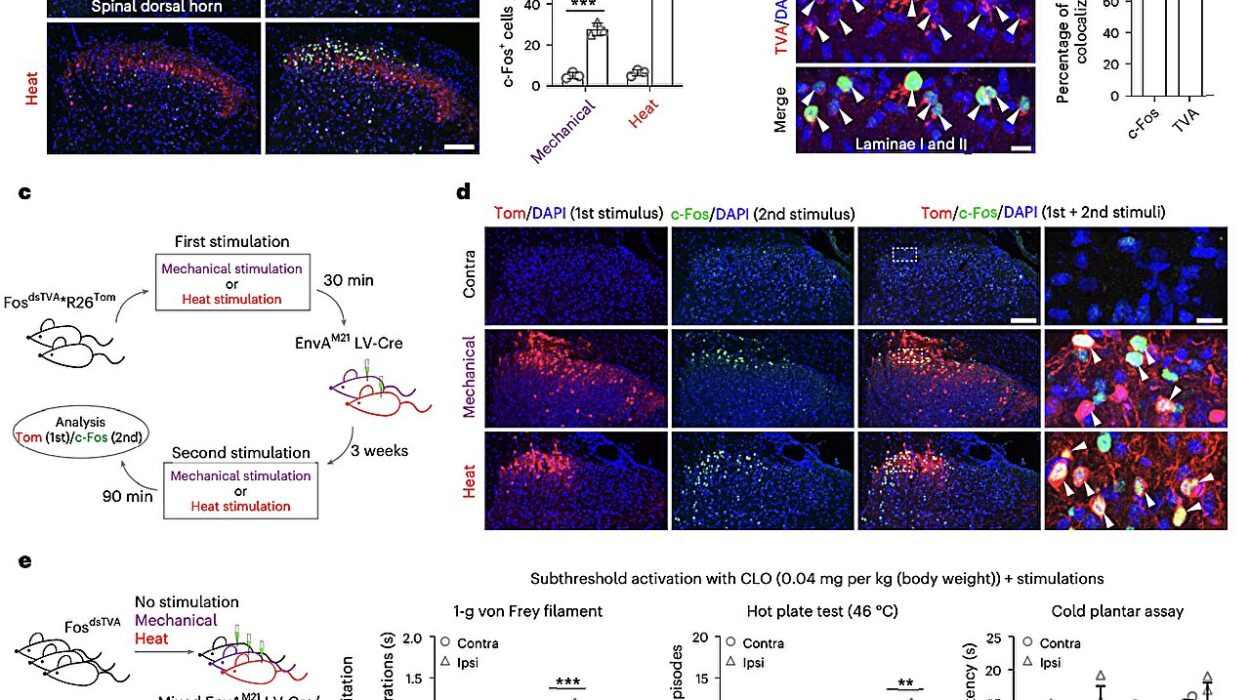
At the center of this research is a small but powerful part of the brainstem called the medullary dorsal horn. It doesn’t get much attention outside of neuroscience, but it plays a key role in how we feel pain. It’s here that “projection neurons” act like messengers, carrying pain information from the body up to the brain. These neurons don’t just pass along the message—they help control how loud the signal is.
In the case of acute inflammation—say, after you twist your ankle—these projection neurons turn down their own volume. They actually reduce their electrical activity, applying the brakes on how much pain information gets sent upstairs to the brain’s pain centers. It’s the nervous system’s way of saying, “The threat is over. You can calm down now.”
Doctoral student Ben Title, under the guidance of Professor Alexander M. Binshtok at The Hebrew University-Hadassah School of Medicine and the Edmond & Lily Safra Center for Brain Sciences (ELSC), led the team behind the study. Together, they discovered that in chronic pain, this system breaks down.
“In chronic conditions, these neurons stop using the brakes,” said Prof. Binshtok. “Instead, they become even more excitable—firing more pain signals, more often. That might be one reason chronic pain feels so relentless.”
A Potassium Current with Power
So what controls this neural braking system? The answer lies in a microscopic river of charged particles—a specific flow of potassium ions known as the A-type potassium current, or IA. This current regulates how easily neurons fire, helping to quiet overactive cells.
In short-term pain, IA ramps up. It helps keep the pain signals in check, preventing the nervous system from going into overdrive. It’s nature’s way of gently dimming the lights after a storm.
But in chronic pain, the IA current doesn’t rise. It stays flat, and the neurons lose their self-control. The electrical storm continues.
Using a combination of high-resolution electrophysiology—essentially listening in on the neurons’ conversations—and sophisticated computer models, the researchers were able to show this pattern again and again.
“This is the first time we’ve seen such a clear difference in how the same neurons behave in acute versus chronic pain,” said Title. “The discovery that IA plays such a central role gives us a very specific target for new kinds of therapy.”
Why Some Pain Persists—and What That Means for the Future
The implications of this research are profound. More than 50 million Americans suffer from chronic pain, according to the CDC. It’s a leading cause of disability, lost work, depression, and opioid use. Yet despite its enormous impact, chronic pain is still not well understood—and too often poorly treated.
Most current painkillers work broadly, numbing the entire nervous system. But they can come with side effects and, in some cases, risk of addiction. What’s been missing is a precise understanding of what goes wrong in the transition from acute to chronic pain.
This study provides that missing link. It suggests that when the IA braking mechanism fails, the body’s pain pathways become stuck in a loop. The nerves keep shouting “danger!” even when the original injury is long gone.
And if scientists can find a way to boost or mimic the IA current, they might be able to stop that feedback loop—essentially restoring the brakes and preventing chronic pain from ever taking hold.
“This changes how we think about pain,” Binshtok said. “It’s not just about treating the symptom. It’s about understanding the switch that turns off the body’s natural control. If we can flip that switch back on, we may be able to stop chronic pain before it begins.”
A New Frontier in Pain Science
This research is part of a broader shift in neuroscience: a move toward understanding pain not as a static experience, but as a dynamic process shaped by electrical and chemical patterns deep in the brain and spinal cord. For years, scientists have known that acute and chronic pain feel different. But now, they’re beginning to understand why—down to the behavior of individual neurons.
It also raises new questions. Why does the IA current fail in some people but not others? Could genetics, trauma, or environment play a role? And could other pain-relief systems in the body also be breaking down in chronic conditions?
The answers will take time. But this study is a leap forward—showing that the body’s natural pain controls are not only real, but modifiable. And that brings hope not just for pain relief, but for pain prevention.
From Lab Bench to Life
While this breakthrough is still in the research phase, its potential is already rippling through the world of pain medicine. Targeted therapies that restore the IA current or enhance the brain’s natural braking system could usher in a new generation of pain treatments—ones that are safer, smarter, and more effective than ever before.
It also offers validation for people who have been told their pain is “all in their head.” Chronic pain is real, and it has real biological roots. The nervous system, in some cases, has simply lost its ability to quiet itself.
By listening to the whispers of ancient neurons deep in the brainstem, scientists are now beginning to hear the truth behind the screams of chronic pain.
And that may be the beginning of healing—not just for bodies, but for millions of lives.
Reference: Ben Title et al, Opposite regulation of medullary pain-related projection neuron excitability in acute and chronic pain, Science Advances (2025). DOI: 10.1126/sciadv.adr3467. www.science.org/doi/10.1126/sciadv.adr3467