Stress. It’s a word we casually toss around in conversation like a stray pebble—“I’m so stressed,” “Work is stressing me out,” “This week has been insane.” But unlike that harmless pebble, stress is no small matter. Beneath the surface, it can carve deep canyons in your physical and mental health. It’s the invisible weight we carry on our shoulders, even when we don’t notice it, and over time, it can break us down in subtle yet powerful ways.
While a bit of stress here and there is a normal part of life—and can even be helpful—chronic, unrelenting stress is a different beast entirely. It quietly corrodes our bodies, alters brain chemistry, weakens immunity, and paves the way for a host of diseases. Understanding how stress works, how it harms us, and—most importantly—what we can do about it can make the difference between merely surviving and truly thriving.
Let’s peel back the layers of this modern epidemic and explore the science, symptoms, and solutions.
What Exactly Is Stress?
Stress, at its core, is a survival mechanism. Imagine yourself in the wilderness thousands of years ago. You spot a saber-toothed tiger. Your brain activates its built-in alarm system: the “fight-or-flight” response. Your heart rate jumps, breathing quickens, muscles tense, and non-essential systems—like digestion and reproduction—slow down. Cortisol and adrenaline flood your bloodstream. You’re primed to escape or fight for your life.
That’s acute stress, and it can save your life.
But in today’s world, that “tiger” isn’t a wild animal. It’s a demanding boss, unpaid bills, relationship drama, deadlines, or doomscrolling news about a chaotic world. Our bodies respond to these psychological threats the same way they would a physical one—triggering the same physiological changes. The problem is that instead of a quick burst of energy followed by rest, modern stress tends to be chronic. We don’t outrun the “tiger.” It moves into our homes, our pockets (via smartphones), and even our dreams.
And that’s when stress turns toxic.
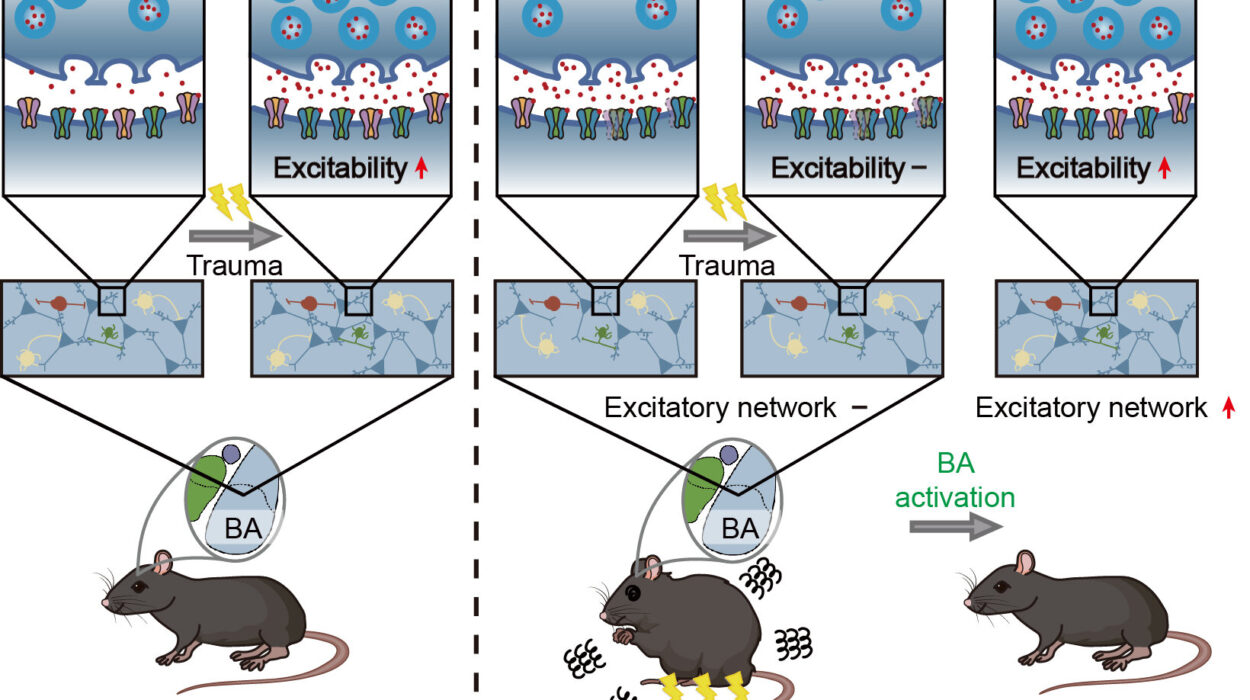
How Stress Hijacks Your Brain
The first organ stress attacks is the brain—and it’s not subtle about it. Your brain is the command center of the stress response, orchestrating hormone releases and directing your body’s every move. But prolonged stress actually remodels the brain in ways that make it harder to cope with life.
In the short term, cortisol—the stress hormone—can help sharpen your focus and memory. But when cortisol levels remain elevated over long periods, the story changes dramatically.
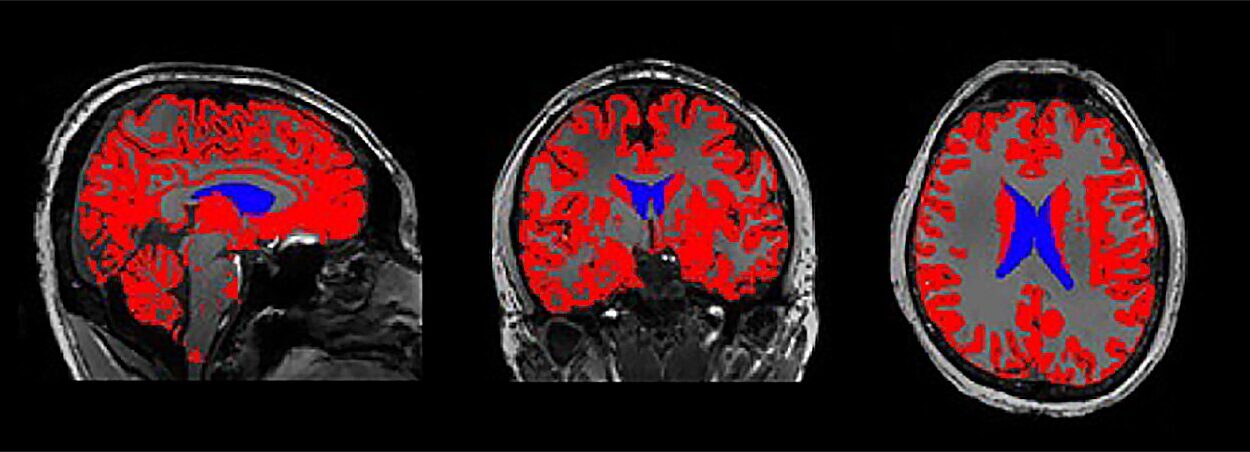
Chronic stress reduces the size of your hippocampus, the area responsible for memory and learning. You may find yourself forgetting simple things, struggling to concentrate, or feeling mentally foggy. At the same time, the amygdala—the brain’s fear center—becomes more active and grows in size. This makes you more reactive, anxious, and emotionally volatile.
Worse yet, the prefrontal cortex, the part of your brain responsible for rational thinking, decision-making, and impulse control, takes a hit too. That means chronic stress doesn’t just make you feel bad; it makes it harder to think clearly and make good choices—creating a vicious cycle of overwhelm.
Stress and the Cardiovascular System: A Dangerous Liaison
When stress becomes a constant companion, your heart and blood vessels feel the strain. Remember that fight-or-flight response? Every time it’s triggered, your heart rate spikes and blood pressure rises. That’s not so bad in short bursts. But chronic stress keeps your cardiovascular system revved up like a car engine that never shuts off.
The result? Wear and tear on your arteries, increased risk of high blood pressure, and a higher chance of heart disease—the leading cause of death worldwide.
Stress also contributes to inflammation in the blood vessels, a key factor in the development of atherosclerosis, where plaque builds up and narrows arteries. This can eventually lead to heart attacks or strokes. People under chronic stress are also more likely to engage in risky behaviors like smoking, overeating, or drinking excessively—all of which compound cardiovascular risks.
Your heart wasn’t built to race all day, every day. Yet chronic stress makes it do just that.
Stress and the Immune System: A Silent Saboteur
Your immune system is your body’s defense army. It fights off viruses, bacteria, and anything else that shouldn’t be there. But chronic stress weakens this army—often without you noticing—until you find yourself getting sick more often, recovering more slowly, or developing strange autoimmune symptoms.
In the short term, stress hormones can actually enhance immune function—one of nature’s ways of helping you deal with injury or infection during a crisis. But with long-term exposure, the immune system becomes less sensitive to cortisol’s regulatory effect. This leaves inflammation unchecked and immune cells sluggish.
Chronic stress has been linked to increased susceptibility to colds, flu, and other infections. It’s also associated with autoimmune diseases like rheumatoid arthritis and lupus, where the body’s immune system mistakenly attacks its own tissues. Moreover, stress may hinder your body’s ability to heal wounds or respond properly to vaccines.
In a world where immune health is more important than ever, chronic stress is a stealthy enemy.
Digestive Mayhem: Stress in the Gut
Have you ever felt butterflies in your stomach before a big presentation? Or lost your appetite during a stressful week? That’s no coincidence. Your gut and brain are intimately connected through the gut-brain axis—a two-way communication network involving nerves, hormones, and microbes.
Stress disrupts digestion in several ways. It slows down or speeds up the movement of food, leading to symptoms like bloating, diarrhea, constipation, or cramping. It increases stomach acid production, which can worsen heartburn or lead to ulcers. And it alters the composition of your gut microbiome—the trillions of bacteria that help digest food, regulate mood, and support immunity.
People with conditions like irritable bowel syndrome (IBS) often report that stress makes their symptoms worse. But even without a formal diagnosis, anyone can experience digestive distress from prolonged stress. It’s your gut’s way of waving a red flag.
Stress and Sleep: The Unrested Mind
One of the cruelest tricks of stress is how it steals your sleep. You’re exhausted, yet when your head hits the pillow, your brain begins its nightly replay of every worry, mistake, and deadline. You toss, turn, and check the clock until it’s 3 a.m.
Stress disrupts sleep in multiple ways. It can delay the onset of sleep, cause frequent awakenings, and reduce the amount of deep, restorative sleep your body craves. Over time, this leads to sleep deprivation—which, in a cruel feedback loop, makes you more vulnerable to stress the next day.
Sleep deprivation impairs memory, mood, and immunity. It increases appetite (especially for sugar and carbs), disrupts blood sugar control, and makes everything feel harder. Without adequate sleep, your ability to cope with stress plummets.
Sleep and stress are strange bedfellows—each making the other worse.
Hormones Out of Balance: Cortisol and Chaos
Cortisol is a bit of a Jekyll and Hyde hormone. In small doses, it’s helpful. It gives you energy, regulates metabolism, and helps you respond to danger. But when stress is chronic, cortisol production goes into overdrive—or eventually, into dysfunction.
Prolonged high cortisol levels can lead to weight gain, especially around the abdomen, where fat cells are more sensitive to cortisol. It can cause blood sugar issues, muscle breakdown, and reduced bone density. In women, it can disrupt menstrual cycles and fertility. In men, it can lower testosterone.
Eventually, in cases of extreme burnout, the body may struggle to produce adequate cortisol at all, leading to a state sometimes referred to as “adrenal fatigue” (a controversial term, but the symptoms—chronic fatigue, low mood, brain fog—are very real).
Your hormonal balance is like a symphony. Chronic stress throws off the entire performance.
Emotional and Mental Health Fallout
It’s no secret that stress messes with your mood. But it’s more than just feeling “off.” Chronic stress is a major contributor to anxiety, depression, irritability, and even burnout. It can erode self-esteem, strain relationships, and sap the joy from daily life.
Prolonged stress alters brain chemistry, reducing levels of serotonin and dopamine—the feel-good neurotransmitters. It also sensitizes the amygdala, making you more reactive to future stress. People under constant pressure often feel trapped in a cycle of overthinking, catastrophizing, and helplessness.
Over time, this can lead to clinical mental health disorders. And in a society that often glorifies busyness and stoicism, many people suffer in silence until the damage is significant.
You can’t separate mind from body. What stresses the soul scars the flesh.
The Good News: Stress Isn’t Destiny
If all of this sounds grim, take heart. Stress may be powerful, but it’s not invincible. Your body has remarkable capacity for healing—if you give it the right tools and environment. And science shows that there are proven, effective ways to reduce stress and even reverse its effects.
The key lies not in eliminating all stress—because that’s impossible—but in managing it skillfully, building resilience, and knowing how to rest and recover.
What You Can Do About It: Science-Backed Solutions
The first step is awareness. Notice your stress patterns. Do you clench your jaw? Snap at loved ones? Skip meals? Lose sleep? Naming stress is the first act of taking back control.
Next, nourish your body. Eat real, whole foods. Prioritize protein, healthy fats, and fiber. Avoid sugar highs and caffeine crashes. Stay hydrated. A well-fed body is a stress-resilient body.
Move your body daily. Exercise is a natural antidepressant. It burns off excess cortisol and floods your brain with endorphins. It doesn’t have to be intense. Even walking, yoga, or dancing counts.
Practice deep breathing. Your breath is a remote control for your nervous system. Slow, deep breathing tells your brain: “I’m safe.” Try box breathing, 4-7-8 breathing, or just sit still and breathe deeply for five minutes a day.
Sleep like it’s your job. Create a calming bedtime routine. Avoid screens before bed. Keep your room cool and dark. Go to bed at the same time every night. Sleep is your brain’s reset button.
Connect with others. Human connection is a powerful antidote to stress. Call a friend, hug someone, join a group, or talk to a therapist. You’re not meant to carry it all alone.
Learn to say no. Boundaries protect your time, energy, and peace. You can’t pour from an empty cup. It’s okay to rest. It’s okay to disappoint others to stay true to yourself.
Try mindfulness and meditation. You don’t need to sit cross-legged for hours. Just notice your thoughts without judgment. Tune into your senses. Be present. Even a few minutes a day changes your brain.
Engage in hobbies. Do something that brings you joy, even if it seems “unproductive.” Paint, garden, bake, write, play an instrument. Joy is medicine.
Seek professional help if needed. If stress is overwhelming or chronic, therapy can be life-changing. Cognitive-behavioral therapy (CBT), mindfulness-based stress reduction (MBSR), and EMDR are powerful tools. There’s no shame in getting help.
The Takeaway: Stress Is Serious—But So Are You
Stress isn’t a badge of honor. It’s not proof of how hard you work or how much you care. It’s a biological response that, left unchecked, can erode your health from the inside out. But it’s also a signal—an invitation to slow down, reassess, and choose a better way.
You are not powerless. You are not weak for needing rest or support. In fact, recognizing the impact of stress and taking steps to manage it is one of the bravest, smartest things you can do.
Your body has been fighting for you. Now it’s time to fight for your body.