Heart disease doesn’t come with flashing red lights or loud sirens. It rarely knocks on the door with a formal announcement. Instead, it creeps in silently, hiding behind everyday habits, stressful routines, poor diets, and unnoticed symptoms. And when it finally reveals itself—often as a heart attack or stroke—it does so with devastating consequences. The numbers don’t lie: heart disease is the number one killer in the world, claiming more lives annually than any other disease, war, or disaster.
From affluent urban centers to remote rural villages, heart disease shows no favoritism. It cuts across borders, affecting men and women, young and old, rich and poor. But why has this particular disease earned such a tragic title? Why does it kill more people each year than all cancers combined, more than infectious diseases, and more than any global pandemic in history?
The answer lies not in a single cause, but in a complex web of biology, lifestyle, environment, and culture. This article will dive deep into the fascinating and sometimes frightening story of why heart disease reigns supreme—and what we can do to dethrone it.
What Exactly Is Heart Disease?
Heart disease is a broad term that encompasses a variety of conditions affecting the heart and blood vessels. The most common type, and the one most responsible for deaths globally, is coronary artery disease (CAD), which occurs when the arteries supplying blood to the heart become narrowed or blocked by plaque—a mix of fat, cholesterol, and other substances.
But heart disease doesn’t stop there. It also includes:
- Heart failure, where the heart can’t pump blood effectively.
- Arrhythmias, or irregular heartbeats, which can be harmless or fatal.
- Cardiomyopathy, a disease of the heart muscle.
- Congenital heart defects, present from birth.
- Peripheral artery disease, affecting limbs and organs.
When people talk about “heart disease” as the leading killer, they’re often referring to CAD and its complications, particularly heart attacks and strokes. But the entire cardiovascular system plays a role—and when any part of it fails, the results can be catastrophic.
The Global Numbers: A Grim Reality
Each year, more than 17 million people die from heart disease, and that number is expected to increase to over 23 million by 2030, according to the World Health Organization. That’s nearly one-third of all global deaths. In some countries, heart disease accounts for almost half of all deaths. It outpaces infectious diseases, cancers, and accidents combined.
What’s more alarming is that many of these deaths are preventable. Lifestyle factors such as diet, exercise, smoking, alcohol, and stress contribute significantly to heart disease risk. So why, if the causes are well-known, does heart disease continue to dominate global mortality charts?
The answer is layered—rooted in modern life, behavioral psychology, economic inequalities, and even human biology itself.
The Modern Lifestyle: A Recipe for Disaster
Walk through any busy city, and you’ll see the hallmarks of modern life—fast food joints, sedentary office jobs, high stress, digital distractions, and convenience everywhere. This new way of living, while efficient, is also incredibly harmful to our hearts.
Sedentary Living
We sit more than any generation before us. From desks to couches to car seats, physical inactivity has become the norm. The human heart, a muscle that thrives on movement, begins to suffer when we don’t move enough. Inactivity leads to obesity, insulin resistance, and poor circulation—all of which increase heart disease risk.
Processed Diets
Food today is cheap, fast, and often nutrient-poor. Diets high in saturated fats, trans fats, sugar, and sodium are now common across the globe. These ingredients fuel high blood pressure, high cholesterol, diabetes, and inflammation—each a stepping stone toward cardiovascular catastrophe.
Chronic Stress
Stress might seem like a mental burden, but it leaves a biological footprint. Chronic stress triggers the release of cortisol, a hormone that, over time, damages blood vessels, raises blood pressure, and encourages fat storage. Modern stress isn’t just about survival—it’s about finances, deadlines, relationships, and existential dread. All of it puts a heavy toll on the heart.
Poor Sleep and Disrupted Rhythms
Sleep is when the body repairs itself. But in an always-on world, quality sleep is elusive. Sleep disorders, including sleep apnea, are directly linked to heart disease. And irregular sleep patterns—thanks to night shifts or excessive screen time—disrupt the body’s natural rhythms, increasing cardiovascular risk.
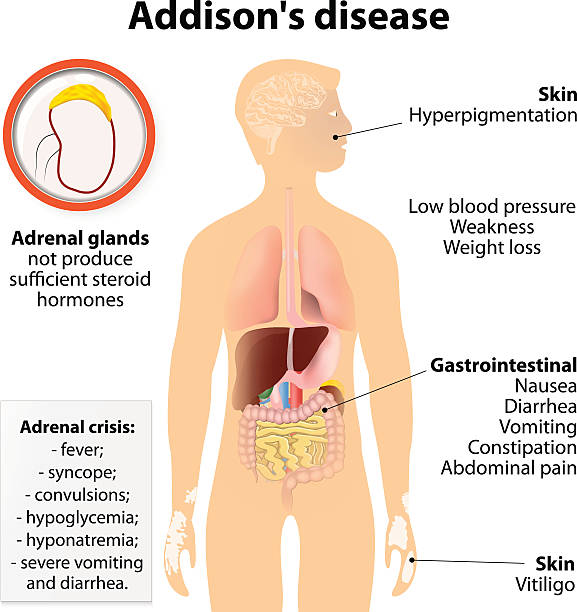
Biological Factors: When Your Body Turns Against You
Heart disease isn’t just about external factors. Our own biology plays a key role.
Genetics
Some people inherit genes that predispose them to high blood pressure, high cholesterol, or heart defects. Familial hypercholesterolemia, for example, is a genetic condition where cholesterol levels are dangerously high from a young age. Even if you live a healthy life, your DNA might still increase your risk.
Inflammation
Chronic inflammation in the body—caused by infections, autoimmune diseases, or even belly fat—contributes to plaque buildup in arteries. Over time, this plaque can rupture, triggering blood clots that lead to heart attacks or strokes.
Aging
The older we get, the more wear and tear accumulates in our cardiovascular system. Arteries stiffen, the heart muscle weakens, and the risks compound. With the global population aging, heart disease rates are naturally rising too.
The Role of Inequality and Globalization
Heart disease doesn’t strike evenly across the map. Where you live and how much money you have can vastly affect your heart health.
Economic Inequality
In low-income regions, access to healthcare is limited. Preventive care is rare. Diagnosis often comes late—after damage is already done. In wealthier nations, poor neighborhoods still experience higher rates of heart disease due to food deserts, unsafe environments for exercise, and limited access to care.
Urbanization and Globalization
As countries modernize, traditional diets and active lifestyles are replaced by processed food and sedentary jobs. Urbanization brings convenience—but also pollution, stress, and fast food. Heart disease often skyrockets as a byproduct of economic “progress.”
Cultural Factors
In some cultures, obesity is a sign of wealth or status. In others, meat-heavy diets are a central part of identity. Changing habits isn’t just a matter of knowledge—it’s about shifting cultural values, which takes time and sensitivity.
Medical Myths and Misunderstandings
Part of the reason heart disease is so deadly is that it’s misunderstood.
“It Won’t Happen to Me”
Many people see heart disease as an older man’s disease. But women are equally at risk—and symptoms in women can be different and harder to recognize. Younger people are increasingly affected too, thanks to obesity and diabetes.
“I Feel Fine, So I Must Be Fine”
Heart disease is often silent. High blood pressure, high cholesterol, and atherosclerosis don’t cause symptoms until it’s too late. That’s why it’s called a “silent killer.” Regular checkups are critical—but they’re often ignored.
“I Can Fix It Later”
Some believe they can eat poorly and avoid exercise now, then fix everything later. But damage accumulates over decades. A heart attack in your 50s is often the result of choices made in your 30s—or even earlier.
The Ripple Effects of a Broken Heart
Heart disease isn’t just a personal tragedy—it has massive societal costs.
Economic Burden
Treating heart disease drains healthcare systems. In the U.S. alone, it costs over $200 billion annually. Globally, it leads to lost productivity, rising insurance costs, and stretched healthcare infrastructure.
Emotional and Social Toll
When someone has a heart attack or heart failure, it affects their entire family. Caregivers often experience stress and burnout. Loved ones live in fear of another attack. Recovery can be slow and traumatic, changing lifestyles and family dynamics forever.
Intergenerational Impact
Children of heart disease patients often adopt the same risky habits—or grow up with fear and stress. The emotional and behavioral patterns around health can repeat across generations unless actively addressed.
The Role of Prevention: Hope on the Horizon
The good news? Heart disease is largely preventable. Up to 80% of cases are linked to lifestyle and behavioral factors. That means we have the power to change the story.
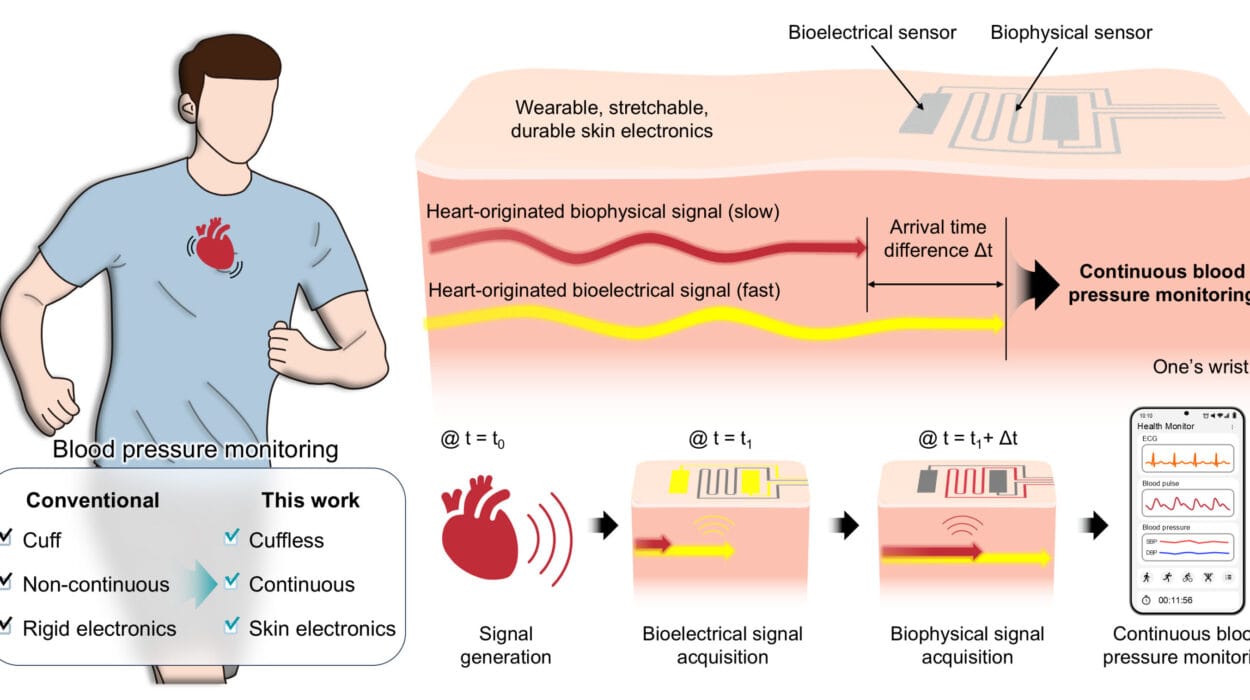
Early Detection
Routine screenings for blood pressure, cholesterol, blood sugar, and BMI can catch risk factors early. The sooner you know your numbers, the better your chances of avoiding serious complications.
Healthy Habits
Regular exercise—even a brisk 30-minute walk daily—strengthens the heart. A balanced diet rich in fruits, vegetables, whole grains, and healthy fats can lower risk dramatically. Quitting smoking, reducing alcohol, managing stress, and sleeping well are all part of the equation.
Public Health Campaigns
Governments and organizations are increasingly recognizing the need for education, access, and awareness. From smoking bans to food labeling, public policy plays a role in creating heart-healthy environments.
Conclusion: A Call to Action
Heart disease may be the world’s deadliest killer—but it doesn’t have to be. It’s not a fate we must accept. It’s a challenge we can rise to meet—with education, action, compassion, and innovation.
We need to change the way we think about our hearts—not just as organs, but as reflections of how we live. Every bite we eat, every step we take, every choice we make moves us closer to heart health—or heart harm.
Let this be the moment we stop underestimating the silent threat. Let it be the moment we take our hearts seriously—not just on World Heart Day, but every single day.
Because a healthy heart is not just a goal. It’s a legacy.