Attention-deficit/hyperactivity disorder (ADHD) is often imagined as a childhood condition—restless kids in classrooms, distractibility, impulsive behavior. But for millions of adults worldwide, ADHD is a lifelong companion. It doesn’t fade with age; it evolves. Adults with ADHD often grapple with persistent problems: forgetfulness, mental fog, disorganization, difficulty focusing, and challenges with emotional regulation. While many scientific efforts have focused on neurotransmitters like dopamine and norepinephrine to explain these symptoms, new research is exploring an entirely different domain: how the brain takes out the trash.
In a study recently published in the Journal of Affective Disorders, researchers uncovered early evidence that adults with ADHD may have impairments in their brain’s waste-clearing system—an overlooked but essential component of neural health called the glymphatic system. While this discovery doesn’t rewrite what we know about ADHD, it offers a compelling new piece of the puzzle—one that connects sleep, brain inflammation, memory, and attention to a system that operates mostly in the dark.
What Is the Glymphatic System?
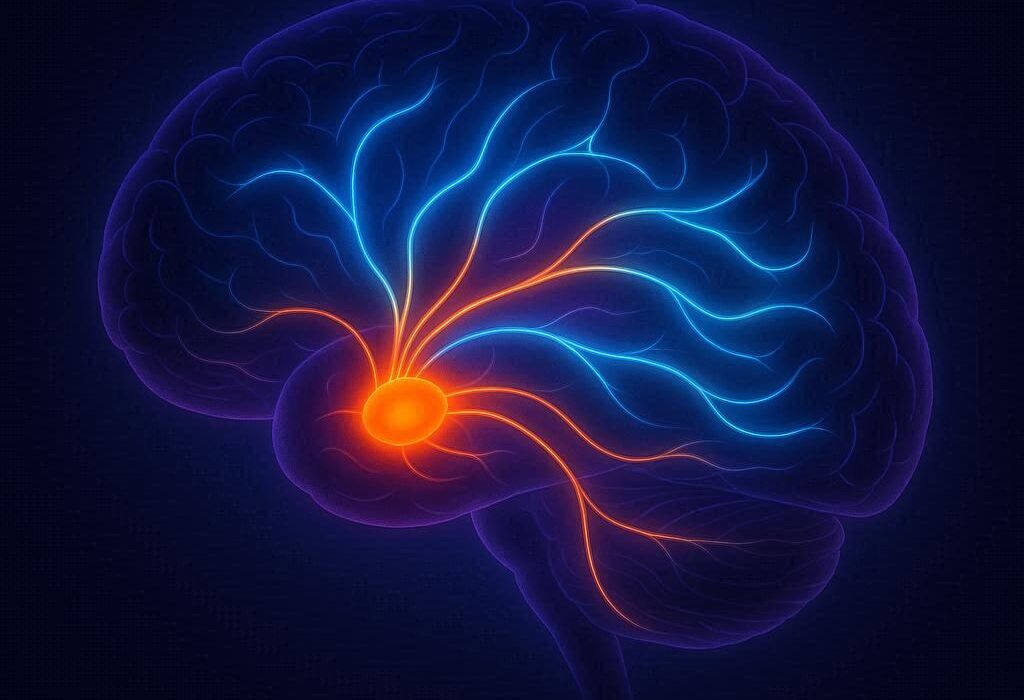
Imagine your brain as a bustling city. Each neuron is like a factory producing energy and information, and in the process, these factories create waste—metabolic byproducts, misfolded proteins, leftover neurotransmitters. Just like any efficient city, the brain needs a sanitation department to remove this clutter. That’s where the glymphatic system comes in.
First described in the past decade, the glymphatic system is a network that flushes out waste by pushing cerebrospinal fluid (CSF) through brain tissue, using perivascular pathways—tiny tunnels surrounding blood vessels. This system is most active during deep sleep, when neurons shrink slightly to create space for fluid to flow more freely. The term “glymphatic” combines “glial” (referring to the brain’s support cells) and “lymphatic,” because this system mimics the body’s traditional lymphatic clearance mechanism.
Disruptions in glymphatic function have already been linked to neurodegenerative diseases like Alzheimer’s and Parkinson’s. But until now, its role in neurodevelopmental conditions like ADHD remained largely unexplored.
The Study: Looking Inside the Brain’s Plumbing
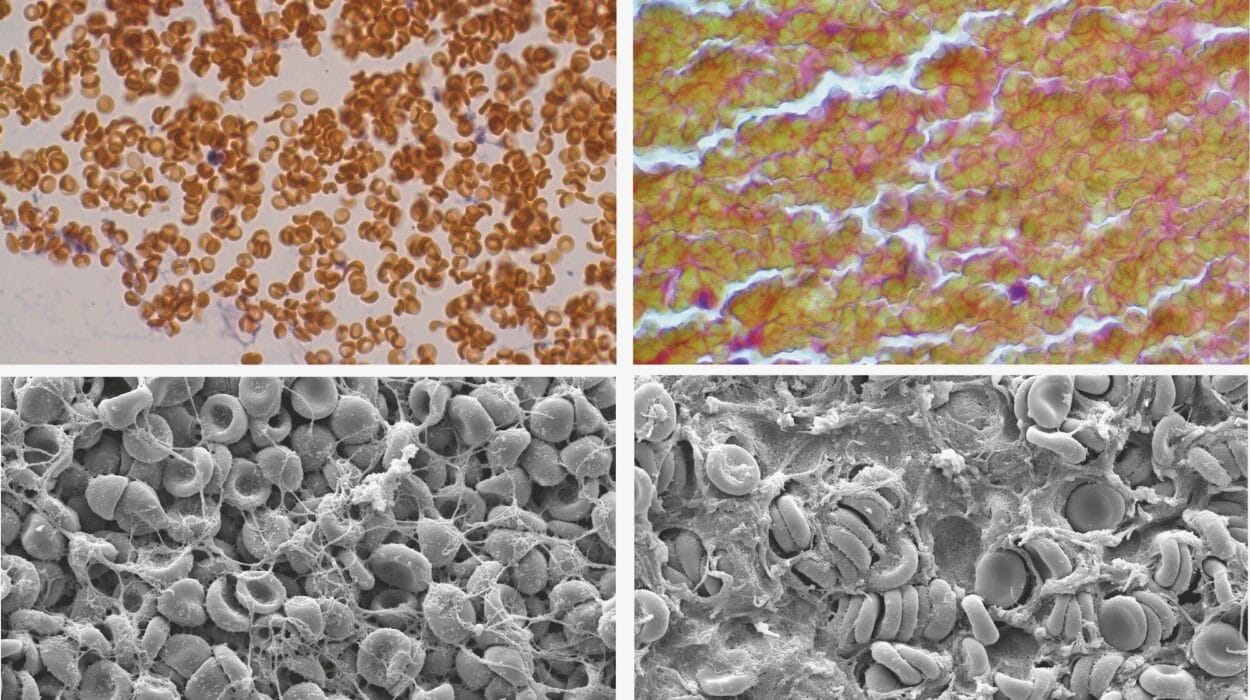
To investigate this hidden system, researchers analyzed data from the University of California, Los Angeles Consortium for Neuropsychiatric Phenomics LA5c Study. They looked at 149 adults in total—41 diagnosed with ADHD and 108 neurotypical controls. Using advanced MRI-based imaging techniques, the team assessed three different markers of glymphatic activity:
- The ALPS Index: Short for “Analysis Along the Perivascular Space,” this measure reflects the ease with which cerebrospinal fluid moves along blood vessels. Higher ALPS scores mean better fluid flow.
- Choroid Plexus Volume: This brain structure produces cerebrospinal fluid. An increased size may indicate altered CSF production or flow.
- gBOLD-CSF Coupling: This refers to how well fluctuations in brain activity (measured by the BOLD signal in fMRI) synchronize with CSF movement.
Participants also completed the Adult ADHD Self-Report Scale and several cognitive assessments, including the California Verbal Learning Test and Wechsler Memory Scale—tools used to assess memory, verbal learning, and attention.
The key finding? Adults with ADHD had significantly lower ALPS index scores. This suggests a sluggish glymphatic system—reduced clearance of waste via cerebrospinal fluid pathways.
What Happens When the Brain Can’t Clean Itself?
The implications of impaired glymphatic function are far-reaching. When the brain’s natural cleaning system slows down, metabolic waste—including amyloid-beta proteins and other potentially toxic molecules—can accumulate. In ADHD, this may help explain why cognitive symptoms like forgetfulness, attention lapses, and memory impairments are so persistent and difficult to manage.
More specifically, the study found that lower ALPS scores in adults with ADHD were linked to worse performance on visual memory tasks and delayed recognition tests. Interestingly, these correlations were stronger in the right hemisphere of the brain, a region often associated with attention control, spatial processing, and nonverbal memory.
There were other suggestive patterns too. The choroid plexus volume tended to be larger in the ADHD group, although this difference wasn’t statistically significant. This could hint at a compensatory mechanism—perhaps the brain tries to make more CSF in response to slowed clearance, or it may reflect underlying dysfunction in fluid regulation. The gBOLD-CSF coupling did not significantly differ between groups, suggesting that some aspects of fluid-brain synchronization remain intact.
Why Might Glymphatic Dysfunction Happen in ADHD?
Though the study wasn’t designed to uncover causes, several hypotheses emerge.
One major suspect is sleep dysfunction. The glymphatic system does most of its work during deep, slow-wave sleep—a state that many people with ADHD struggle to achieve. Insomnia, restless sleep, delayed sleep phase syndrome, and shorter sleep duration are all commonly reported in adults with ADHD. Poor sleep could mean reduced glymphatic activity, leading to a vicious cycle: impaired clearance worsens cognition, which further disrupts sleep, and so on.
Another candidate is inflammation. Neuroinflammation has increasingly been implicated in ADHD. Chronic low-grade inflammation may damage glial cells—especially astrocytes, the star-shaped support cells that help regulate the glymphatic system through specialized water channels called aquaporin-4. If these channels are impaired, fluid can’t move efficiently, and waste builds up.
A third possibility is neurotransmitter imbalance. Dopamine and norepinephrine are known to play key roles in attention, motivation, and impulse control. But they also influence cerebrovascular function and fluid dynamics. Disruptions in these systems could have knock-on effects on glymphatic function.
Lastly, structural brain differences—especially in white matter tracts and perivascular spaces—might directly affect fluid flow. The ALPS index specifically measures how well CSF moves along fiber pathways, and a reduction here could point to microstructural changes in the brain’s communication highways.
Implications for Treatment: A New Therapeutic Frontier?
If glymphatic dysfunction contributes to ADHD symptoms, could improving glymphatic flow help?
While speculative, this opens intriguing therapeutic avenues. First and foremost: improving sleep. Encouraging deep sleep through behavioral therapy, better sleep hygiene, or pharmacological support might offer more than just mood stabilization—it might help restore the brain’s cleaning system.
Physical activity is another potential ally. Exercise boosts circulation, improves sleep, and enhances lymphatic function elsewhere in the body. It may stimulate glymphatic flow as well.
Targeting inflammation is another possible strategy. Anti-inflammatory diets, omega-3 fatty acids, and even medications that modulate the immune system are being explored in other neurological conditions and might hold promise here too.
Researchers also suggest the possibility of astrocyte-targeted therapies. While not yet in clinical use, drugs that modulate aquaporin channels or glial function could one day help fine-tune fluid movement in the brain.
A Glimpse into the Future of ADHD Research
It’s important to temper excitement with caution. This study is cross-sectional, meaning it captures a single moment in time. It cannot determine cause and effect. Does glymphatic dysfunction cause cognitive impairment in ADHD—or does ADHD itself, through poor sleep and altered brain function, impair the glymphatic system?
The sample size, while respectable, is relatively small, and all participants came from a single dataset. Further studies in larger, more diverse populations are needed to confirm these findings and understand their broader implications.
Nonetheless, this research breaks new ground. It invites a broader view of ADHD—one that moves beyond dopamine and synapses, toward the slow, hidden processes that support brain health behind the scenes. It suggests that adult ADHD may not be just a chemical imbalance or behavioral issue—it may also be a disorder of clearance, structure, and sleep.
Reframing ADHD: From Hyperactivity to Homeostasis
For decades, ADHD has been framed as a disorder of behavior—something to be managed with medications and behavioral interventions. While these remain crucial, the growing body of research into sleep, inflammation, and now glymphatic function suggests a deeper biological story.
This new lens invites compassion and curiosity. The adult with ADHD struggling to concentrate may not simply lack willpower or discipline. They may be fighting against a tired brain burdened with metabolic waste, starved of deep sleep, and struggling to maintain internal balance.
Understanding the glymphatic system’s role in this process doesn’t just open up new treatment possibilities—it deepens our empathy. It reminds us that the mind is not separate from the body, and that health emerges from the quiet rhythms of flow, rest, and renewal that most of us take for granted.
As scientists continue to map these hidden networks, one thing becomes clear: sometimes, the answers to the most persistent mental health questions are hiding not in the firing of neurons, but in the spaces between them.