When we think of bones, we often imagine something lifeless and static—rigid white structures that exist solely to hold us upright. But bones are not the inert scaffolding we see in anatomy charts. They are living tissue, biologically active and constantly remodeling themselves in response to the body’s needs. They grow, adapt, repair, and even communicate with other tissues. Beneath the surface of their apparent stillness is a world in constant flux.
At the heart of bone health lies a balance between two key forces—construction and demolition. Bone-building cells called osteoblasts lay down new material, while bone-resorbing cells known as osteoclasts break it down. In youth and early adulthood, these two teams work in harmony, shaping and strengthening the skeleton. But over time, the balance can shift. The builders slow down, the demolition crew picks up speed, and the once-resilient bones begin to erode.
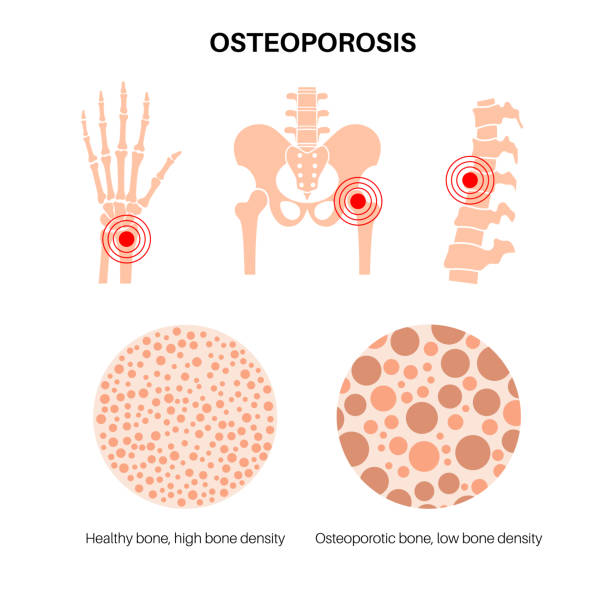
This process is the silent genesis of osteoporosis, a disease that weakens bones to the point where even a minor bump or fall can result in a fracture. It’s a condition that affects hundreds of millions of people worldwide, particularly older adults, and yet it often goes unnoticed until a bone breaks. Understanding how bones become fragile requires a journey into the biology of the skeleton, the forces of aging, the subtle signs of imbalance, and the ways we might prevent or reverse the process.
The Microstructure Beneath the Surface
To understand osteoporosis, we must first grasp the intricate architecture of healthy bone. Far from being solid throughout, bones are composed of two types of tissue: cortical bone and trabecular bone. Cortical bone forms the dense outer layer, strong and compact, while trabecular bone resides inside, a spongy lattice that resembles a honeycomb.
This internal scaffolding is crucial. Trabecular bone gives bones both lightness and resilience. It’s where most of the metabolic action happens, including the exchange of minerals like calcium and phosphate. Its structure adapts to the stresses placed upon it—becoming denser in athletes, thinner in those who are bedridden.
When osteoporosis sets in, it targets this spongy matrix first. The trabeculae—the tiny struts that form the honeycomb—begin to thin, and some disappear altogether. As the structure weakens, the bone becomes less able to bear weight or absorb shock. Cortical bone also becomes thinner and more brittle, further compounding the fragility.
This breakdown doesn’t happen overnight. It’s often a slow, silent erosion, accumulating over years or decades. But when enough bone mass is lost, the consequences can be swift and devastating.
The Role of Remodeling and the Balance of Power
Bone is the only tissue in the body that can regenerate itself without scarring. Throughout life, small areas of bone are constantly being resorbed and rebuilt in a process known as remodeling. This allows bones to repair microscopic damage, adapt to changing mechanical demands, and regulate mineral levels in the blood.
Remodeling is governed by a cellular ballet between osteoblasts and osteoclasts. Osteoclasts dig pits into old bone, releasing stored minerals into circulation. Osteoblasts then fill these pits with new bone matrix, restoring strength.
In youth, this process is balanced. During growth and early adulthood, bone formation even exceeds resorption, allowing the skeleton to increase in mass and density. Peak bone mass is typically reached in the late twenties to early thirties.
But as we age, this balance tilts. Hormonal shifts—especially the decline of estrogen in women after menopause—accelerate bone resorption. Osteoblasts can’t keep up. The result is net bone loss, and over time, a decline in structural integrity.
What’s more, the bone remodeling process becomes less efficient with age. The time it takes to replace resorbed bone lengthens, and the new bone laid down is often less well mineralized. This makes the skeleton increasingly porous and prone to fracture.
The Hormonal Orchestra Behind Bone Health
Hormones play a symphonic role in regulating bone density. Estrogen, in particular, is a master conductor. It suppresses bone resorption by inhibiting osteoclast activity and promotes bone formation by supporting osteoblasts. When estrogen levels fall, as they do during menopause, the protective brake on bone loss is released.
Testosterone also supports bone health, and while men typically experience a more gradual hormonal decline with age, low testosterone can still lead to bone loss in men. Other hormones—including parathyroid hormone, calcitonin, and vitamin D—contribute to the regulation of calcium metabolism and bone turnover.
Parathyroid hormone, for example, is secreted when calcium levels drop in the blood. It signals osteoclasts to resorb bone and release calcium, helping to maintain homeostasis. Chronic overactivity of this system, such as in hyperparathyroidism, can lead to excessive bone loss.
Vitamin D, on the other hand, facilitates calcium absorption in the gut and plays a key role in bone mineralization. Without sufficient vitamin D, bones become soft and weak, a condition called osteomalacia in adults and rickets in children.
Disruptions in any of these hormonal pathways can tip the scales toward bone fragility. In many cases, osteoporosis is not caused by a single deficiency but by a subtle interplay of multiple hormonal imbalances.
The Silent Progression of a Fragile Disease
One of the most insidious aspects of osteoporosis is that it progresses without pain or symptoms—until a fracture occurs. The disease has earned the moniker “silent thief” because it can quietly steal away bone mass for years.
Spinal compression fractures are often the first sign. These occur when weakened vertebrae collapse under normal pressure. They can cause sudden back pain, height loss, and stooped posture. Many go undiagnosed, mistaken for ordinary back strain or the inevitable signs of aging.
Hip fractures are more dramatic and more dangerous. They often result from a simple fall and are a major cause of disability and mortality in the elderly. A person who suffers a hip fracture may never regain full mobility, and the risk of death in the year following a hip fracture can be alarmingly high.
Wrist fractures, particularly of the radius, are another common presentation, especially in postmenopausal women. These typically result from falls onto outstretched hands and can significantly impact daily functioning.
By the time these fractures occur, the underlying bone loss is already advanced. This is why early detection and prevention are so crucial—because osteoporosis doesn’t announce itself until the damage is done.
The Risk Factors That Shape Bone Destiny
Osteoporosis is not an equal opportunity affliction. Several factors increase the likelihood of developing the condition, some modifiable and others written into our genetic code.
Age is the most significant risk factor. Bone mass declines naturally with time, and the risk of osteoporosis rises sharply after age 50. Women are at higher risk than men, largely due to hormonal differences, and the risk increases further after menopause.
Genetics also plays a substantial role. If your parents or grandparents had osteoporosis or suffered fractures in old age, your risk is elevated. Ethnicity matters too—Caucasian and Asian individuals tend to have lower peak bone mass compared to those of African descent, placing them at higher risk.
Lifestyle factors are equally important. Smoking, excessive alcohol consumption, and a sedentary lifestyle all contribute to bone loss. Diets low in calcium and vitamin D starve the skeleton of the raw materials it needs to maintain strength.
Certain medications can also accelerate bone loss. Long-term use of corticosteroids, for example, disrupts the bone remodeling process. Other drugs, such as some anticonvulsants, antidepressants, and chemotherapy agents, can negatively impact bone health.
Chronic medical conditions—including rheumatoid arthritis, celiac disease, kidney disease, and hormonal disorders like hyperthyroidism—can all increase fracture risk by affecting bone metabolism or nutrient absorption.
Understanding these risk factors is the first step in prevention. By identifying those at risk early, interventions can be put in place before bones become dangerously fragile.
The Role of Nutrition and Lifestyle in Building Strong Bones
Nutrition is not just a footnote in bone health—it’s a cornerstone. Calcium and vitamin D are the headliners, but they are far from the only nutrients that matter.
Calcium is the main mineral found in bone. Adults need around 1000 to 1300 mg per day, depending on age and sex. Good sources include dairy products, leafy greens, fortified foods, and certain types of fish like sardines and salmon with bones.
Vitamin D is necessary for calcium absorption and utilization. Without it, even a calcium-rich diet won’t build bone. Sunlight triggers vitamin D synthesis in the skin, but geographic location, season, skin pigmentation, and age can all affect production. Supplements may be needed in some cases to maintain optimal levels.
Other nutrients also play supporting roles. Vitamin K helps regulate bone mineralization and works in concert with vitamin D. Magnesium, phosphorus, and zinc are essential cofactors in bone-building processes. Protein is critical too—while excessive protein without adequate calcium can leach calcium from bones, moderate intake supports bone matrix formation.
Exercise, particularly weight-bearing and resistance activities, is one of the most effective ways to stimulate bone growth. Activities like walking, jogging, dancing, and lifting weights apply stress to the skeleton, signaling it to strengthen in response. Conversely, prolonged immobility or zero-gravity environments, such as during space travel, result in rapid bone loss.
Avoiding smoking and limiting alcohol intake are also crucial. Both substances impair bone-forming cells and increase fracture risk. Taken together, lifestyle interventions can significantly delay or even prevent the onset of osteoporosis.
Diagnosing the Invisible Condition
Because osteoporosis has no symptoms until a fracture occurs, screening is vital. The gold standard for diagnosis is the dual-energy X-ray absorptiometry scan, or DEXA. This painless, non-invasive test measures bone mineral density (BMD) and compares it to the optimal peak bone mass of a healthy young adult.
The results are given as a T-score. A T-score of -1.0 or higher is considered normal. Scores between -1.0 and -2.5 indicate osteopenia, a condition of low bone mass that may progress to osteoporosis. A T-score of -2.5 or lower confirms osteoporosis.
Doctors may also use FRAX, a tool developed by the World Health Organization, to estimate an individual’s 10-year risk of fracture based on bone density and other risk factors.
Regular screening is especially important for women over 65, men over 70, and younger individuals with known risk factors. Early diagnosis allows for timely intervention, potentially preventing devastating fractures.
Modern Approaches to Treatment and Prevention
Treating osteoporosis involves both slowing bone loss and stimulating new bone formation. A variety of medications are available, each with different mechanisms and benefits.
Bisphosphonates, such as alendronate and risedronate, are the most commonly prescribed drugs. They work by inhibiting osteoclast activity, thereby reducing bone resorption. They can significantly lower the risk of spine and hip fractures, though long-term use may be associated with rare side effects like jaw osteonecrosis.
Selective estrogen receptor modulators (SERMs) mimic estrogen’s protective effects on bone without stimulating breast or uterine tissue. They are often used in postmenopausal women who cannot take hormone replacement therapy.
Denosumab, a monoclonal antibody, also targets osteoclasts and is administered as a biannual injection. It’s effective for those who cannot tolerate oral medications.
Newer anabolic treatments, like teriparatide and abaloparatide, stimulate osteoblasts to build new bone. These are typically reserved for individuals with severe osteoporosis or multiple fractures.
Romosozumab, a dual-acting agent that both stimulates bone formation and inhibits resorption, represents a novel approach and has shown promising results.
In addition to medication, treatment plans should include lifestyle changes, fall prevention strategies, physical therapy, and ongoing monitoring.
The Emotional and Social Cost of Fragility
Osteoporosis doesn’t just affect the body—it alters lives. The psychological toll of fractures can be immense. Loss of independence, fear of falling, chronic pain, and reduced mobility often lead to depression, anxiety, and social isolation.
In older adults, hip fractures in particular can mark a turning point, triggering a cascade of decline. Hospitalization, surgery, rehabilitation, and long-term care may follow. For many, the fracture becomes a symbol of aging and vulnerability—a loss of control over one’s own body.
Public awareness and support are vital. Education can empower people to take preventive steps. Community programs and public health campaigns can promote screening, encourage healthy habits, and provide resources for those already affected.
A Vision for Healthier Bones Across the Lifespan
Osteoporosis is not inevitable. While aging will always bring changes to bone structure, fragility fractures are not a guaranteed consequence. Prevention begins in childhood, with proper nutrition, physical activity, and habits that support skeletal development.
As we move through life, continuing to challenge our bones with activity, fueling them with the right nutrients, and monitoring their health can help preserve strength well into old age.
In the end, our bones are more than structural supports—they are the silent partners in every step we take, every gesture we make. They carry our histories, adapt to our needs, and suffer in silence when neglected.
By understanding osteoporosis and the hidden processes that underlie it, we can listen to the silent signals, care for our bones as we do our hearts and minds, and carry ourselves more surely into the future.