Diabetes is more than just a single disease—it’s a complex metabolic disorder that affects millions of people worldwide in diverse and often deeply personal ways. At its core, diabetes interferes with how the body manages blood sugar, also known as glucose, which serves as a vital energy source for cells. But the implications of that interference are far-reaching, influencing everything from heart health and kidney function to eyesight and nerve signaling.
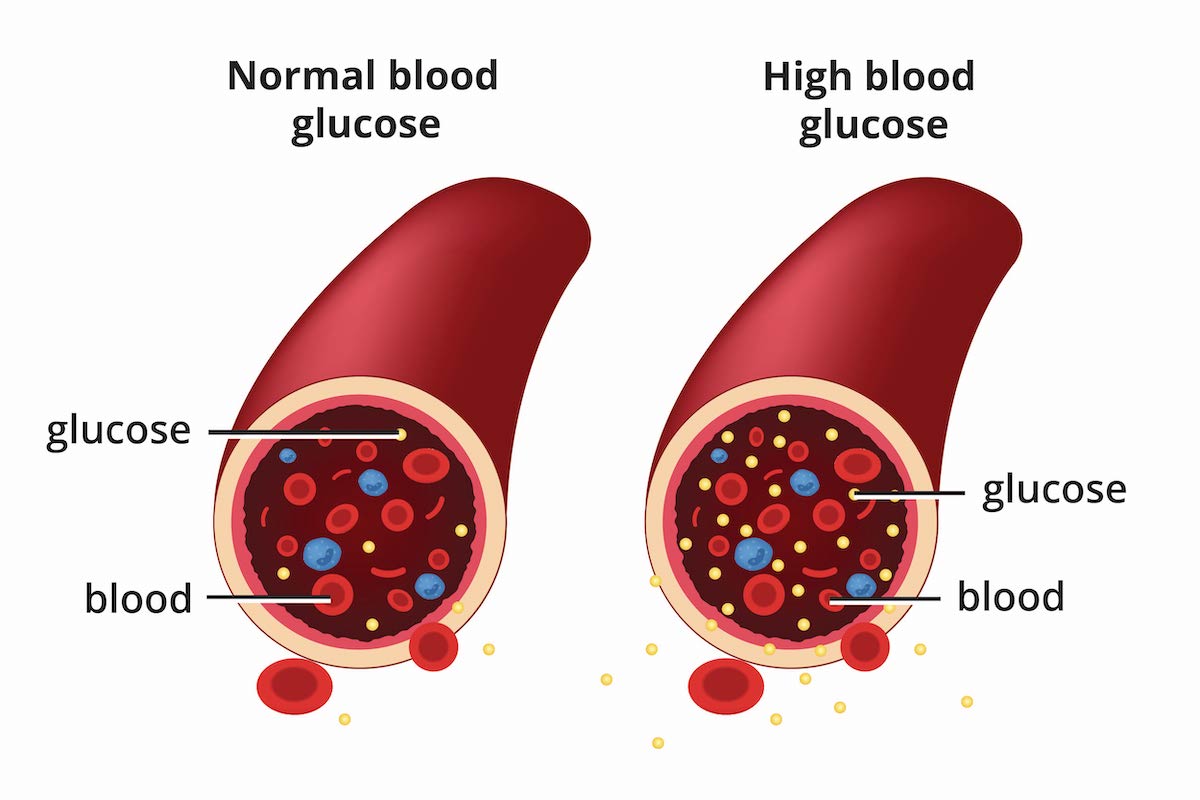
Though the mechanisms behind diabetes can vary, all forms of the disease share a common problem: glucose cannot enter cells efficiently, causing sugar to build up in the bloodstream. That buildup can silently wreak havoc on the body over time if not properly managed. Understanding the different types of diabetes, the causes behind them, and the treatments available offers a window into one of the most pressing public health challenges of our time—and into the stunning intricacies of human metabolism.
The Silent Sugar in the Blood
To grasp what goes wrong in diabetes, we must first understand what happens when things go right. After you eat, carbohydrates in food are broken down into glucose. This glucose travels through the bloodstream and acts like fuel for cells. But to use this fuel, cells require insulin, a hormone produced by the pancreas. Think of insulin as a key that unlocks the door, allowing glucose to enter cells and provide energy.
In diabetes, that lock-and-key system malfunctions. Either the body stops making insulin, doesn’t make enough of it, or becomes resistant to it. As a result, glucose remains in the bloodstream, unable to reach the cells that need it. Over time, this can damage blood vessels, organs, and tissues, and lead to complications such as blindness, amputations, heart disease, and kidney failure.
The most striking and insidious aspect of diabetes is that people often live with it for years without symptoms. During this time, damage continues silently. That’s why diabetes is sometimes called a “silent killer”—and why awareness, early detection, and proactive management are so essential.
Exploring the Different Faces of Diabetes
Diabetes isn’t a single entity. Instead, it comes in several distinct types, each with its own causes, progression, and treatment approach. Though the end result—elevated blood glucose—is common to all, the path each form takes to get there varies significantly.
The two main forms are Type 1 and Type 2 diabetes. There’s also gestational diabetes, which occurs during pregnancy, and several rarer forms that stem from genetic mutations or other disorders.
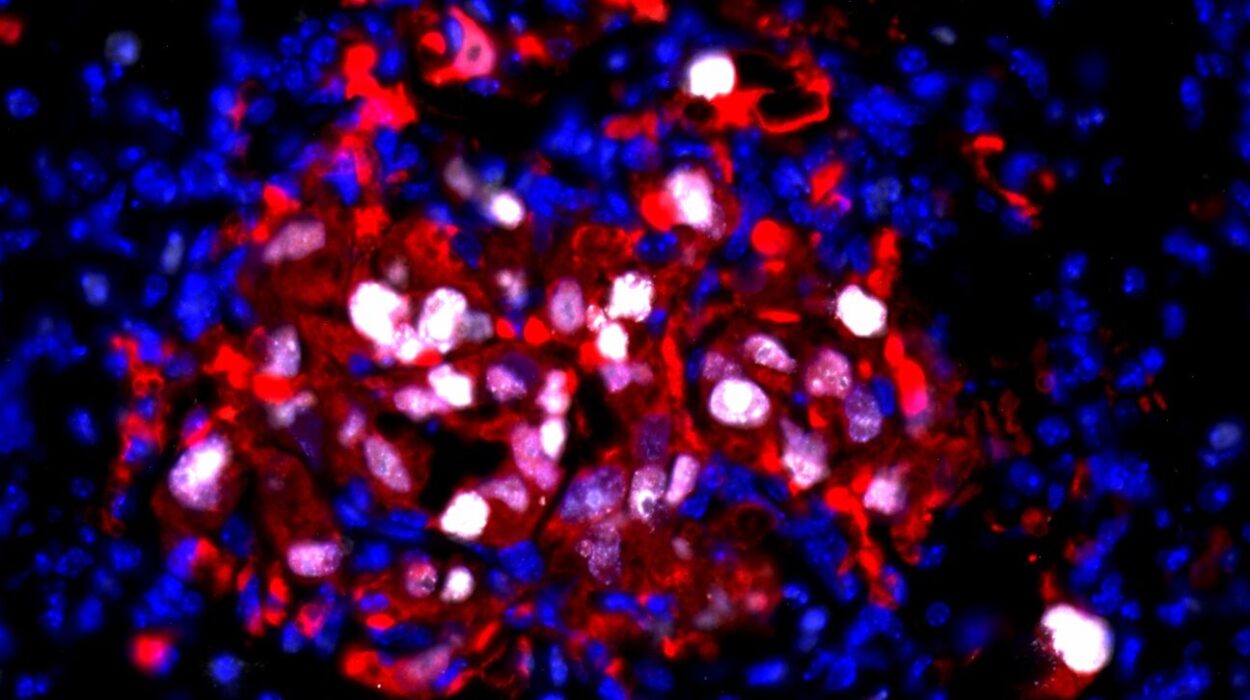
Type 1 diabetes, formerly known as juvenile diabetes, is an autoimmune disease. The body’s own immune system mistakenly attacks the insulin-producing beta cells in the pancreas. As these cells are destroyed, insulin production plummets to near zero, making people with Type 1 entirely dependent on insulin therapy to survive. It often appears in childhood or adolescence, though adult-onset Type 1 is also possible.
Type 2 diabetes, by contrast, usually develops later in life—though it is now increasingly seen in younger people, even children. In this form, the body still makes insulin, but either not enough of it, or the cells become resistant to its effects. It is deeply linked to lifestyle factors such as obesity, inactivity, and poor diet, but also influenced by genetic predisposition.
Gestational diabetes occurs during pregnancy when hormonal changes temporarily impair insulin function. Though it usually resolves after childbirth, it can increase the mother’s risk of developing Type 2 diabetes later in life, and can also affect the baby’s health.
There are also rare forms of diabetes known as monogenic diabetes, such as MODY (maturity-onset diabetes of the young), which arise from single gene mutations. Additionally, secondary diabetes can occur as a result of medical conditions like pancreatic disease or as a side effect of certain medications.
The Autoimmune Storm Behind Type 1 Diabetes
In Type 1 diabetes, the problem isn’t that the body misuses insulin—it’s that it stops making it altogether. The root cause is a misfiring immune system that turns on its own pancreas. For reasons still not fully understood, the immune system identifies the insulin-producing beta cells in the pancreas as foreign invaders and systematically destroys them.
This autoimmune process can be swift or slow. In some children, it manifests quickly, leading to abrupt symptoms such as unquenchable thirst, frequent urination, unexplained weight loss, and extreme fatigue. In other cases, it unfolds gradually over months or even years. But once a critical mass of beta cells is destroyed, the body loses its ability to regulate glucose, and insulin injections become a lifelong necessity.
There is no known way to prevent Type 1 diabetes. Genetics play a role—certain genes increase susceptibility—but environmental factors, possibly viruses or dietary triggers, also seem to be involved. Research is ongoing to better understand the precise causes and to explore interventions that might halt or delay the autoimmune attack.
The Insulin Resistance Puzzle in Type 2 Diabetes
While Type 1 diabetes is a case of autoimmune destruction, Type 2 diabetes is a tale of growing resistance. In this scenario, the body produces insulin, sometimes in abundance, but the cells no longer respond to it effectively. It’s as if the key still fits the lock, but the lock is rusted and jammed.
To compensate, the pancreas pumps out more insulin, trying to force glucose into resistant cells. Over time, this overwork wears out the insulin-producing cells. Eventually, insulin levels may drop as well, leading to a double failure of both production and sensitivity.
Obesity—especially the accumulation of fat around the abdomen—is a major driver of insulin resistance. Adipose tissue isn’t just inert storage; it secretes inflammatory molecules that can disrupt insulin signaling. Inactivity and poor diet contribute further, and genetics also play a role. Not everyone who is overweight develops Type 2 diabetes, and not all people with Type 2 are overweight.
Because Type 2 develops gradually, it often goes unnoticed for years. By the time it is diagnosed, complications such as nerve damage, kidney dysfunction, or vision problems may already be underway. But unlike Type 1, Type 2 diabetes is often preventable and, in many cases, reversible with lifestyle changes.
When Pregnancy and Blood Sugar Collide
Pregnancy is a time of profound hormonal changes. In some women, these changes impair insulin function, leading to gestational diabetes. This condition affects how cells use glucose during pregnancy and can pose risks for both mother and child.
For the mother, gestational diabetes increases the risk of high blood pressure, complications during delivery, and future Type 2 diabetes. For the baby, excessive birth weight, preterm birth, and low blood sugar after delivery are concerns.
Fortunately, gestational diabetes is usually manageable with dietary changes, exercise, and sometimes insulin. After birth, blood sugar levels typically return to normal. However, the experience serves as a red flag for future health risks and highlights the importance of long-term monitoring.
The Genetic Threads in Rare Forms of Diabetes
Monogenic diabetes is a less common but fascinating category. These forms result from mutations in a single gene that affect insulin production or function. MODY, for example, resembles Type 2 diabetes but often arises in adolescence or young adulthood and is typically passed down through families in an autosomal dominant pattern.
Other rare forms include neonatal diabetes, which appears in the first six months of life, and diabetes due to mitochondrial DNA mutations. Diagnosing these forms often requires genetic testing, but doing so can significantly change treatment. Some types of MODY, for instance, respond better to oral medications than to insulin.
The Emotional and Social Toll of Diabetes
Diabetes is more than numbers and biochemistry—it’s a psychological and social challenge. Managing it requires constant vigilance: checking blood sugar, counting carbohydrates, taking medications, exercising, and coping with the ever-present risk of complications. The burden can be exhausting.
Many people with diabetes experience “diabetes distress”—a unique emotional struggle tied to the relentlessness of care and the fear of failure. There’s also stigma: Type 2 diabetes is often incorrectly assumed to be entirely self-inflicted, leading to shame and blame. Type 1 diabetics may be misunderstood or treated as fragile.
Access to care, healthy food, and support networks also shapes outcomes. Socioeconomic inequality and systemic barriers mean that some communities face disproportionate rates of diabetes and worse outcomes. The global burden of diabetes is thus as much about social justice as it is about medical science.
The Tools and Technologies of Treatment
Modern diabetes care is a marvel of innovation. For Type 1 diabetes, insulin therapy is non-negotiable. Insulin comes in various forms—rapid-acting, long-acting, and intermediate—and is delivered through injections, insulin pens, or pumps. Continuous glucose monitors (CGMs) allow users to track blood sugar levels in real time, enabling better control and fewer surprises.
For Type 2 diabetes, lifestyle change is the first and most powerful treatment. A diet rich in whole foods, regular physical activity, weight loss, and stress management can dramatically improve insulin sensitivity and sometimes even send diabetes into remission.
When lifestyle change isn’t enough, medications step in. Metformin is often the first-line drug—it reduces liver glucose production and improves insulin sensitivity. Other drugs include sulfonylureas, SGLT2 inhibitors, DPP-4 inhibitors, and GLP-1 receptor agonists, which work through different mechanisms.
In advanced Type 2 diabetes, insulin may also become necessary. Bariatric surgery is another tool for some patients with obesity and diabetes, often leading to rapid improvements or even resolution of blood sugar problems.
Future Horizons in Diabetes Research
The quest for a cure continues. For Type 1 diabetes, researchers are exploring immune therapies to halt the autoimmune attack, as well as beta cell regeneration and transplantation. Encapsulated islet cells, gene editing technologies like CRISPR, and stem-cell derived insulin-producing cells are all under investigation.
For Type 2 diabetes, the frontier lies in precision medicine: tailoring treatments based on genetic, metabolic, and lifestyle factors. There’s also growing interest in the microbiome—the trillions of gut bacteria that influence metabolism—and how they might affect insulin sensitivity.
Artificial pancreas systems, which integrate insulin pumps and CGMs using smart algorithms, offer real-time blood sugar control. These devices represent a leap toward autonomous diabetes care and reduced burden on patients.
The Global Epidemic and the Path Forward
Diabetes is a global crisis. The World Health Organization estimates that over 500 million people worldwide live with diabetes, a number expected to climb in coming decades. The economic toll is staggering, with billions spent annually on treatment and complications.
But diabetes is also a solvable problem. Type 2 diabetes, in particular, is largely preventable through healthy lifestyle choices. Public health efforts aimed at promoting nutritious diets, active living, and early screening can dramatically reduce incidence. Reducing food deserts, taxing sugary beverages, and investing in community health workers are just some of the tools at our disposal.
On the treatment side, making insulin and other therapies affordable and accessible worldwide is critical. Many people in low-income countries still lack the basics of diabetes care—a cruel irony for a disease that, with proper management, need not be fatal.
A Story Still Being Written
Diabetes may be ancient—it was described by Egyptian physicians over 3,000 years ago—but it is also very much a disease of the modern world. Our sedentary lifestyles, processed diets, and environmental changes have collided with genetic vulnerability to create a perfect storm.
Yet within that storm lies opportunity. With better science, smarter technology, and a commitment to equity, we can transform the diabetes story from one of chronic suffering to one of empowerment and hope. Whether through community-level change or molecular breakthroughs, the arc of diabetes research bends toward solutions.
Each person with diabetes writes their own chapter in that story. Some manage with ease, others with difficulty. But all face the same essential challenge: to live well in the face of a demanding and relentless disease. And increasingly, they do—thanks to science, resilience, and the collective will to improve the lives of millions.